Welcome to the monthly SHDA Research Update. Our specialists have selected 3 papers that have been published recently in each speciality (cardiology, cardiothoracic surgery, cardiac imaging, perioperative medicine).
Cardiology
Summarised by Sarah Catchpoole
Results of the new DANISH randomised controlled trial call in to question the benefit of implantable cardioverter-defibrillators (ICD) in patients with non-ischaemic systolic heart failure. Symptomatic patients with a left-ventricular ejection fraction of <35% (n = 1116) were randomised into the ICD group or the control group (usual clinical care) and followed up for a median period of 67.6 months. There was no significant difference between ICD and control groups for the primary outcome death from any cause (21.6% and 23.4%, respectively, p = 0.28), nor were differences significant for the secondary outcomes death from cardiovascular causes and a variety of adverse events including device infection. However, the incidence of sudden cardiac death was reduced in patients in the ICD group (4.3% and 8.2%, respectively, p = 0.005). The authors conclude that although sudden cardiac death is reduced, the ICD for this patient population has no overall mortality benefit compared to usual clinical care.
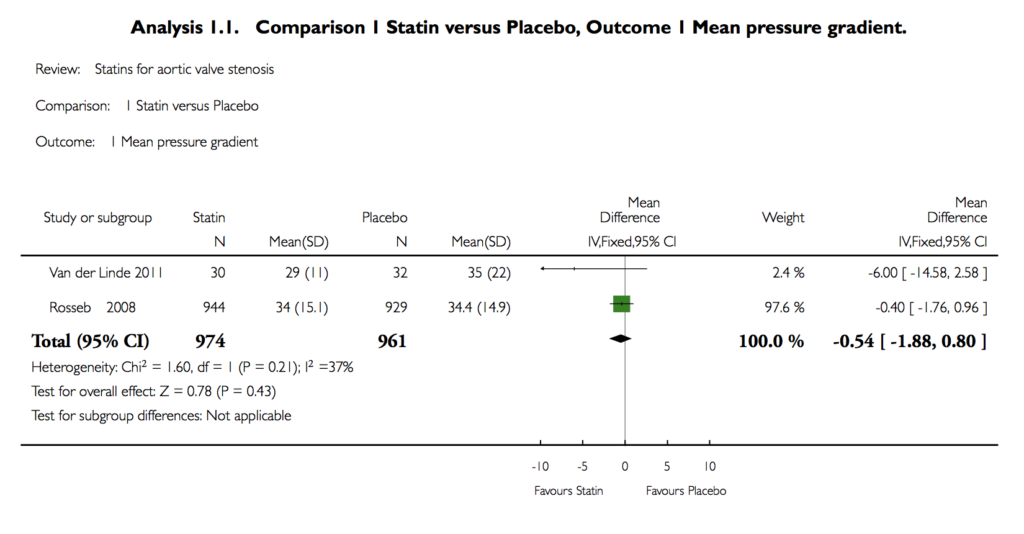
Thiago et al. Statins for aortic valve stenosis. Cochrane Database Syst Rev. 2016 Sep 5.
The developing view of calcific aortic stenosis (AS) as a progressive inflammatory disease similar to atherosclerosis has prompted investigation of the potential role of statins to modify the disease course. This new Cochrane review analyses results of four eligible randomised controlled trials (n = 2360) comparing statins alone or in combination with other therapy to placebo or control conditions. The authors found no significant differences between the groups for the primary outcomes of valve area, pressure gradient, freedom from valve replacement and death from cardiovascular disease. Remarking on the low number and poor quality of trials identified for inclusion, the authors conclude it is uncertain whether statins have a beneficial effect on AS, and further high quality RCTs are needed.
Cardiothoracic Surgery
Summarised by Andrew Haymet
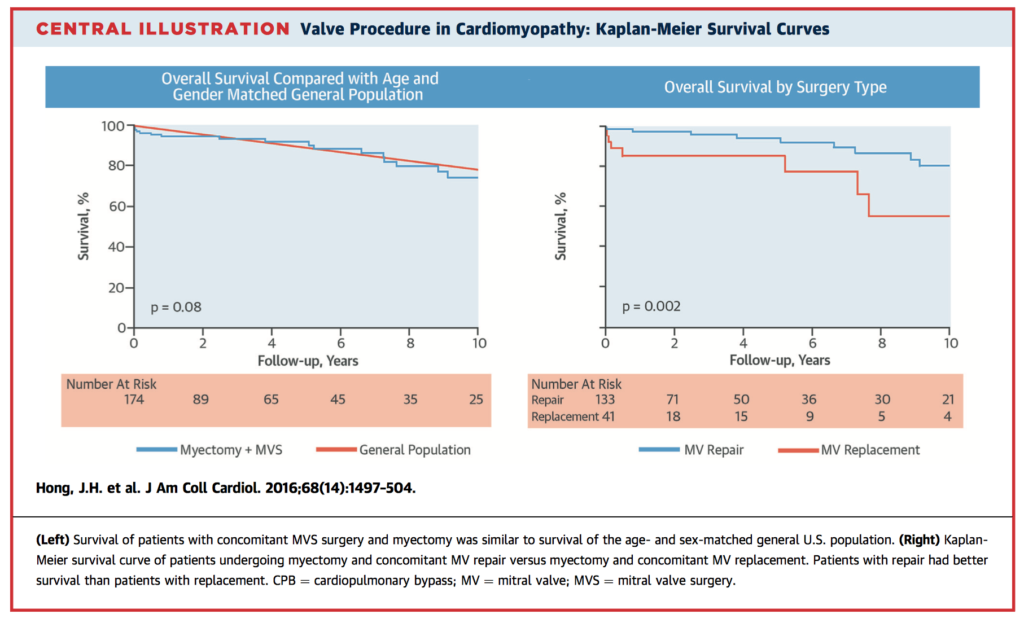
This study aimed to define indications and suitable operative strategy for mitral regurgitation (MR) in patients with hypertrophic obstructive cardiomyopathy (HOCM) undergoing extended transaortic septal myectomy. 2,107 operations performed between January 1993 to May 2014 were retrospectively reviewed. After isolated septal myectomy, the percentage of patients with MR grade ≥3 decreased from 54.3% to 1.7% on early postoperative echocardiogram (p=0.001). Most patients with HOCM experience improvement in MR related to systolic anterior motion of the MV. If MV procedures are indicated, repair delivers improved survival over replacement.
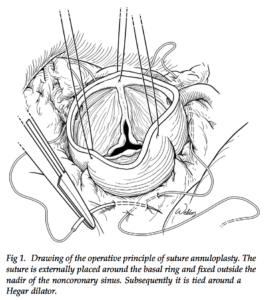
The durability of isolated repair of the regurgitant bicuspid aortic valve (BAV) has been controversial. This paper investigated whether the addition of a suture annuloplasty (SA) improved repair stability. 268 patients between July 1999 and September 2014 underwent isolated repair. Of these, 164 consecutive patients received SA from January 2009 to September 2014 using either braided polyester (n=37) or polytetrafluoroethylene (n=127). Those operated on prior to January 2009 served as controls (n=104). In the control group, freedom from reoperation at 5 and 10 years was 73.2% and 63.7% respectively. With SA, 5-year stability was significantly improved to 92.6% (p=0.0006), with 96.7% for PTFE versus 83.5% for polyester SA (p=0.0132). The use of SA significantly improves repair of regurgitant BAV stability, with PTFE providing optimal stability and fewer local complications.
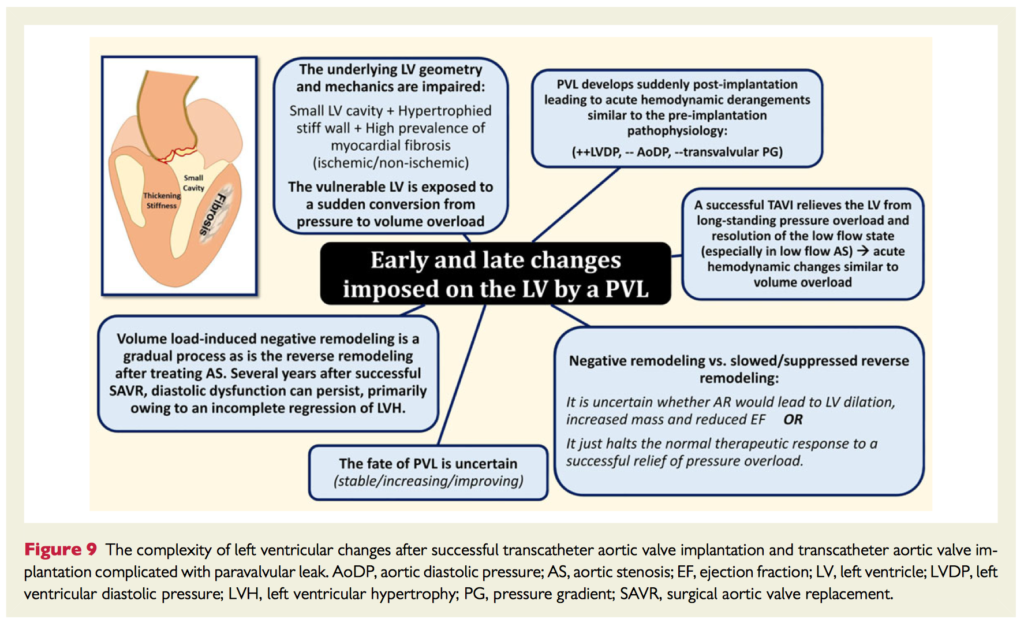
A significant complication of transcatheter aortic valve implantation (TAVI) is paravalvular leakage (PVL). Whilst newer generation TAVI devices offer effective paravalvular sealing, as well as retrieval and repositioning mechanisms which lower the risk of PVL, methods to detect and quantify PVL accurately and in a timely fashion are comparatively lacking. The Valve Academic Research Consortium (VARC) -standardized criteria of PVL assessment are based on echocardiography and inadequately validated according to expert consensus. For immediate post-implantation diagnosis, the combination of transthoracic echocardiography (TTE), quantitative angiography, and a haemodynamic index is often feasible. For follow up imaging, echocardiography is the most convenient. Clinical utility of cardiac magnetic resonance (CMR) velocity mapping is currently limited due to its intrinsic technical demands, the high rates of ICED in patients undergoing TAVI, and the lack of unified definitions of AR severity.
Cardiac Imaging
Summarised by Sarah Catchpoole
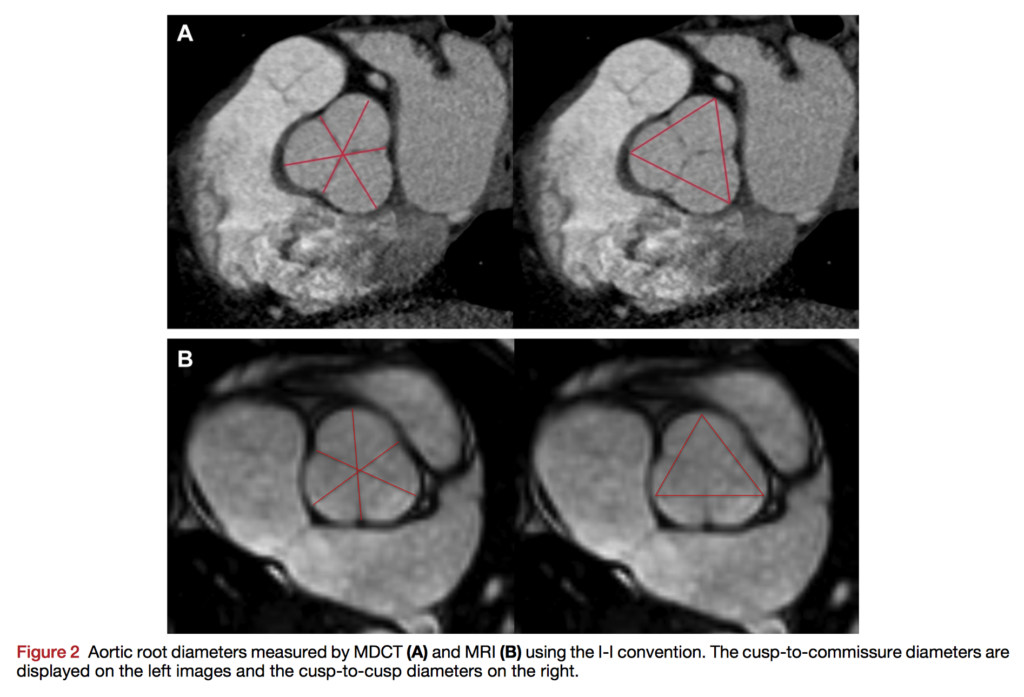
Due to the lack of clear consensus for the best imaging modality to monitor aortic diameters, the authors compared 2D Transthoracic echocardiography (TTE) to multidetector CT (MDCT) and MRI in patients with severe aortic disease. Of the 140 enrolled, 70 were evaluated using TTE and MDCT, and 70 with TTE and MRI. All three imaging methods showed excellent inter- and intraobserver variability. While TTE underestimated values compared to MRI or MDCT using the the inner edge–to–inner edge (I-I) convention (p < 0.0001), accuracy was excellent using the leading edge to leading edge (L-L) convention. The authors suggest that contrary to the AHA and American College of Cardiology recommendations, TTE aortic measurements using the I-I convention underestimates values, while the L-L convention has better agreement with MRI and MDCT. They stress the importance of avoiding disparities in measurements in an era of multi-modality imaging.
Accurate pre-operative localisation of mitral valve prolapse by three dimensional transoesophageal echocardiography remains expertise dependent. The authors investigated whether a semi-automatic novel computer learning technique, Anatomical Intelligence in ultrasound (AIUS), could improve accuracy. In this retrospective study, four non-expert and two expert echocardiographers assessed 24 patients who later underwent mitral valve repair; accuracy was assessed by comparing to surgical findings. As expected, non-experts had significantly lower sensitivity, specificity and accuracy compared with experts. AIUS was able to improve their accuracy from 83% to 89% (p = 0.003), while expert’s accuracy remained consistent at 95%. AIUS was also significantly more efficient, reducing time required for analysis by more than 50% for both experts (1.9 ± 0.7 vs 9.9 ± 3.5 min, P < .0001) and nonexperts (5.0 ± 0.5 vs 13 ± 1.5 min, P < .0001), especially for complex lesions.
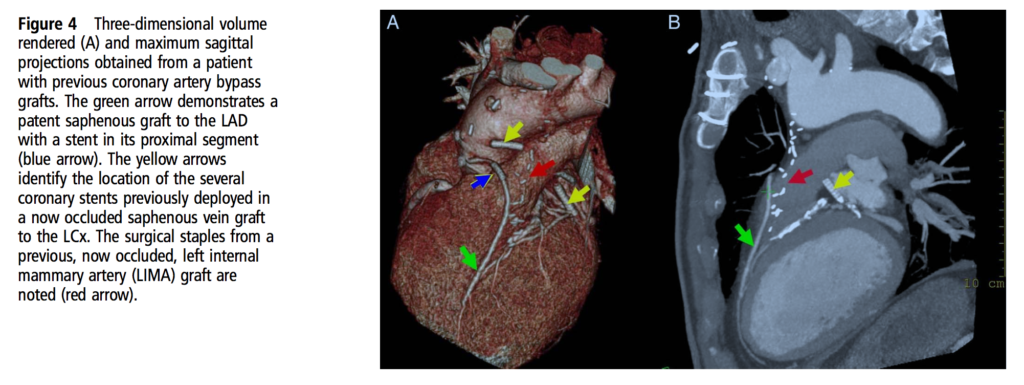
Chahal et al. Cardiac CT: present and future applications. Heart. 2016 Sep 13
A short educational review for clinicians summarising present and potential future applications in the rapidly evolving area of Cardiac CT. While most emphasis is on the role of CT in coronary disease, applications in structural, valvular and congenital heart disease are reviewed.
Perioperative Medicine
Summarised by Andrew Haymet
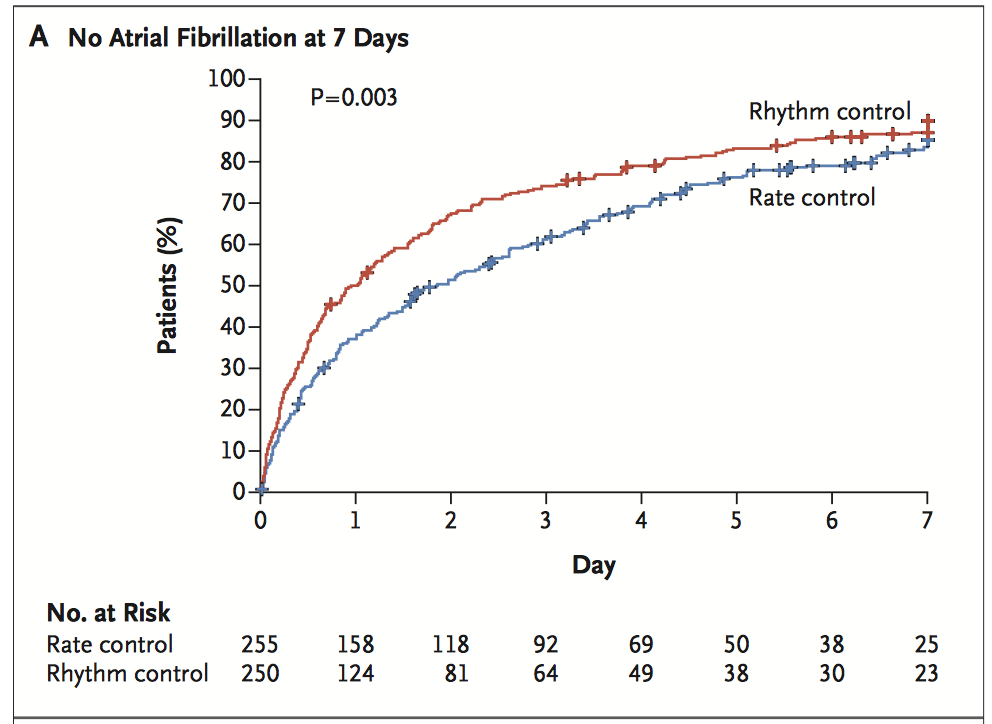
This randomised controlled trial enrolled 2109 patients undergoing elective cardiac surgery for coronary artery or valve disease with no history of atrial fibrillation (AF). Rates of post-operative AF were high, occurring in 28.1% of patients undergoing CABG, 33.7% of those undergoing valve surgery, and 47.3% of those undergoing combined CABG and valve surgery, averaging 33.0% overall. Patients with new AF were then randomised to either rate control (target heart rate >100bpm) or rhythm control (amiodarone with or without a rate slowing agent) conditions. There were no significant differences between the groups for rates of death, adverse events, and duration of hospital stay. In both groups, the majority of patients remained in stable heart rhythm at 60 days after discharge, with 84.2% from the rate control group and 86.9% from the rhythm control group stable for at least 60 days, p=0.41). The authors conclude neither rate control nor rhythm control is superior for management of postoperative AF. However, it must be noted that around 25% of patients in each group deviated from the assigned therapy.
This study compared outcomes of monitored anaesthesia care (MAC) with general anaesthetic (GA) in 1,494 patients undergoing transfemoral transcatheter aortic valve replacement (TAVR). Rates of 30-day mortality and the risk of paravalvular regurgitation (mild or worse) of MAC compared to GA were similar (3.9% vs 4.8%, p=0.564 and 49.5% vs 57.0%, p=0.858). Two patients in the MAC group developed severe paravalvular regurgitation, which was not observed in the GA group. Permanent pacemaker implantation was 19.1% in the MAC group vs 14.8% in the GA group (p = 0.168). Mean intensive care unit stay was 3.5 days for the GA group vs 2.9 days for the MAC group (p = 0.086). A similar 3-year survival rate was observed (MAC 69.4% v GA 69.9%, p = 0.966). Transfemoral TAVR can be performed under MAC with similar early and late outcomes compared with GA. Further studies are required to investigate a potential added risk of severe paravalvular regurgitation and requirement of pacemaker insertion with TAVR under MAC.
This single hospital, retrospective observational study tested the hypothesis that average precardiopulmonary bypass (pre-CPB) transoesophageal echocardiographic (TEE) mean gradient and aortic valve area values (AVA) would differ significantly from preoperative transthoracic (TTE) values in the same population, and thus alter the pre-CPB TEE grading of aortic stenosis. 92 patients were studied who underwent aortic valve replacement with or without coronary artery bypass grafting between 2000 and 2012. PGm with pre-CPB TEE was lower by 6.6 mmHg (95% CI, -4.0 to -9.3mmHg, p<0.001), whilst AVA was higher by 0.10cm2 (95% CI, 0.04 to 0.15 p<0.001), compared with preoperative TTE values. The authors confirmed their hypothesis that pre-CPB TEE generates different PGm and AVA values compared with preoperative TTE, and these differences frequently underestimate AS severity.
Veno-arterial (VA) extracorporeal membranous oxygenation (ECMO) is being increasingly used for patients with refractory cardiorespiratory failure. This retrospective cohort study of 131 patients evaluated the short term (to discharge) and long term (1 year) survival among older (≥65 years) versus younger (<65 years) adults receiving VA-ECMO treatment, adjusted for a diverse range of comorbidities.
The survival rate following VA-ECMO was 48% (n=68/131) and 44% (n=58/131) to discharge and one year respectively. Age ≥65 versus <65 was significantly associated with increased mortality during hospitalization (HR 2.03; 95% CI = 1.23-3.33) and at one year (HR 1.81; 95% CI= 1.12-2.93), however these associations did not maintain statistical significance after adjustment for comorbidities. The authors concluded that older age was not independently associated with short or longer term survival among VA-ECMO patients, but may suggest greater comorbidity, and that age alone may not preclude patients from VA-ECMO treatment.