Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been recently published in each speciality (Cardiology, Cardiac Surgery, Cardiac Imaging, Perioperative Medicine).
Cardiology
Summarised by Sarah Catchpoole
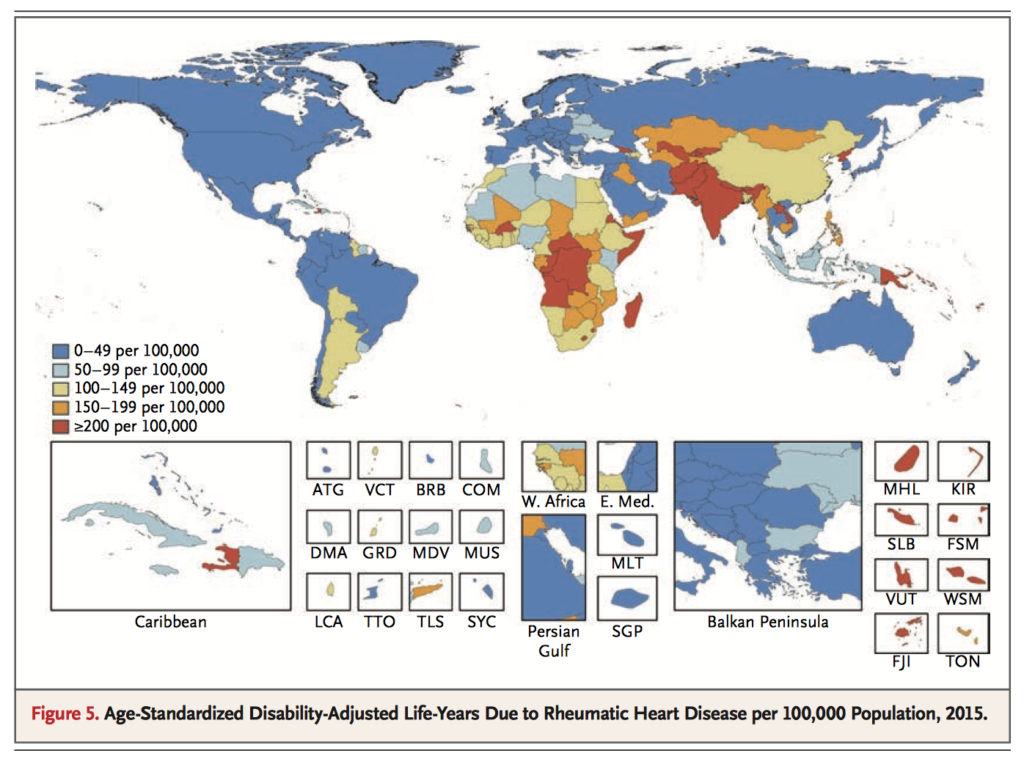
This sub-analysis from the latest Global Burden of Disease study (1990-2015) reveals that while the prevalence and mortality of rheumatic heart disease (RHD) is declining, rates remain high in lower-income countries and highest of all in Oceania. The morbidity and economic impacts of this preventable disease are high, with an estimated 33.4 million cases globally and 10.5 million disability-adjusted life years caused by RHD. Further targeted primary prevention measures could be of great benefit, especially in lower-income countries.
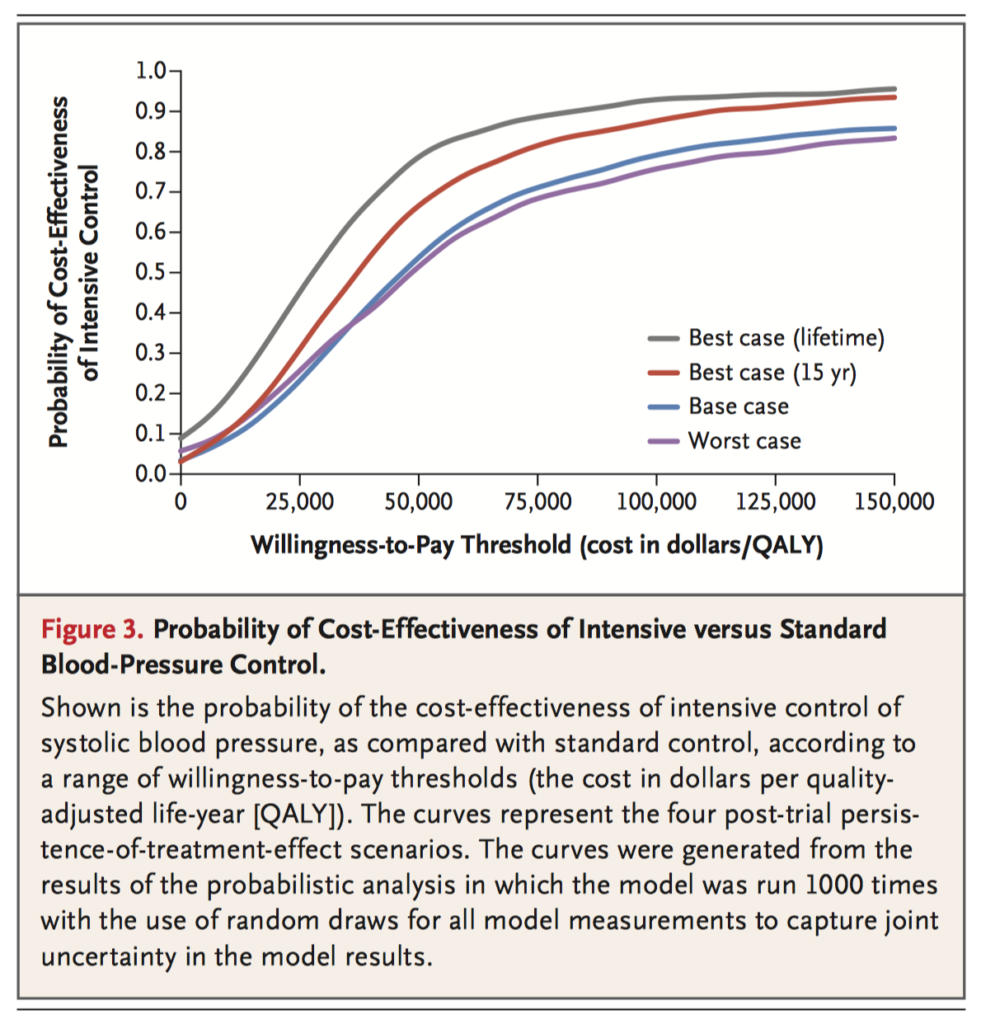
Using data from the Systolic Blood Pressure Intervention Trial (SPRINT), the authors used a microsimulation model to compare the lifetime cost-effectiveness of two regimes of systolic blood pressure control in a hypothetical cohort of SPRINT eligible adults. The intensive regime (target <120mmHg) would prevent more cardiovascular adverse events and improve mortality compared to the standard regime (target <140mmHg), even in the base-case scenario. The increased costs of the regime were offset by reductions in costs for the management of cardiovascular disease, with overall cost effectiveness maximised between 10-20 years of treatment. The authors conclude their estimated cost per quality adjusted life-year gained is below common willingness-to-pay thresholds, even if treatment benefits do not persist beyond 5 years.
In the growing population of adults with adult congenital heart disease (ACHD), the decision to prophylactically place an implantable cardioverter-defibrillator to prevent sudden cardiac death (SCD) is difficult. This study evaluated two recent guidelines (2015 European Society of Cardiology Guidelines, 2014 Pediatric and Congenital Electrophysiology Society/Heart Rhythm Society expert consensus statement) using case-controls taken from an international, multicentre database of 25 790 patients with ACHD. Only 35-41% of SCD cases were correctly identified, with the area under receiver operating characteristic curves between 0.6 and 0.7. The low discriminative power of these guidelines is worrying, as up to 60% of high-risk SCD cases may go unrecognised. The authors stress that the current guidelines are consensus statements derived largely from the literature on acquired heart disease and not randomised controlled trials in ACHD. Clinical decision making remains essential, with further trials needed.
Landmark Study
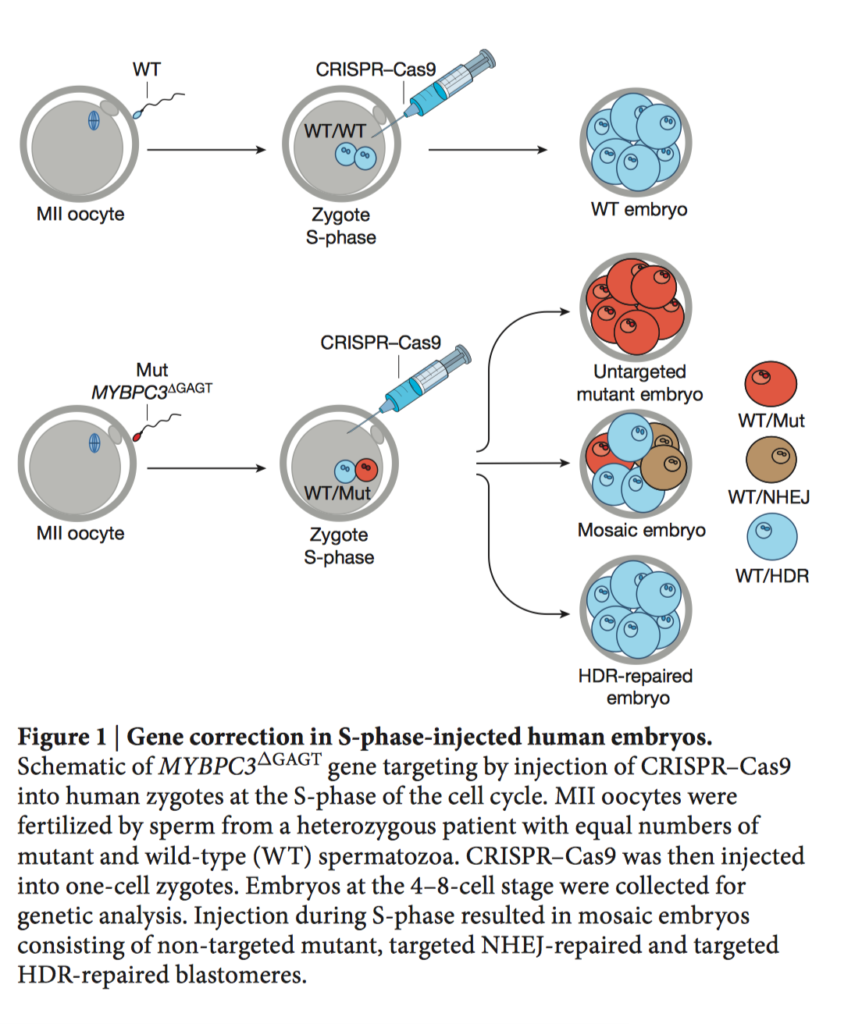
Ma H, et al. Correction of a pathogenic gene mutation in human embryos. Nature. 2017 Aug 2
There are more than 10 000 known monogenetic inherited disorders, including the MYBPC3 mutation which causes hypertrophic cardiomyopathy (HCM). In human preimplantation embryos with heterozygous MYBPC3 mutations, CRISPR-Cas9 technology achieved correction of the mutant paternal allele using a homologous wild-type maternal gene. This successful outcome indicates future clinical application of gene correction in pre-implantation genetic diagnosis is feasible.
Cardiac Surgery
Summarised by Andrew Haymet
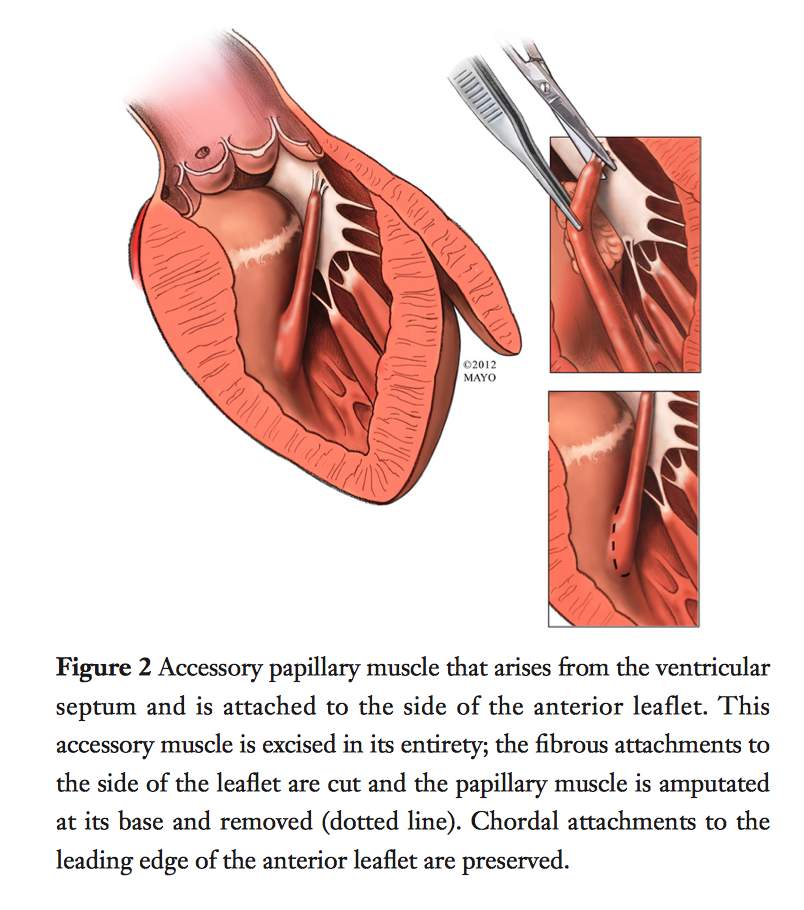
First line management of HOCM is medical therapy, followed by septal myectomy if the condition is intractable. More than 3,000 patients underwent myectomy at the Mayo Clinic, MN, USA between 1993 to 2016. Risk of hospital death after isolated myectomy was <1%. Complications such as complete heart block were uncommon (<2%), however partial or left bundle branch block was a common finding postoperatively. More than 90% of severely symptomatic patients improved by at least two functional classes postoperatively. The authors concluded septal myectomy is an effective and definitive treatment for LVOT obstruction in patients with HOCM, with excellent results in experienced centres which continue to improve.
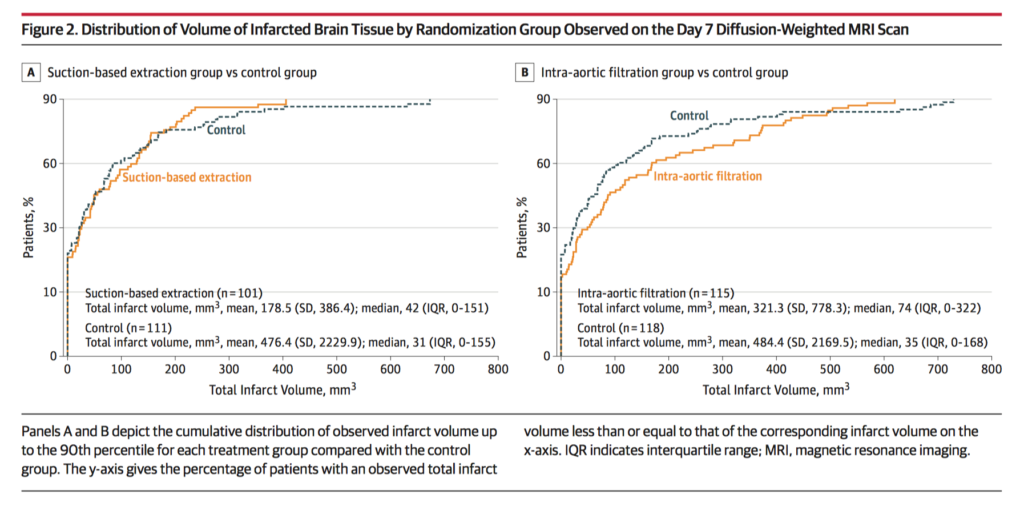
This randomized clinical trial evaluated the efficacy of two cerebral embolic protection devices in 383 patients with calcific aortic stenosis undergoing surgical AVR between March 2015 and July 2016. Use of 1 of 2 cerebral embolic protection devices was evaluated (suction-based extraction, n = 118; intra-aortic filtration device, n = 133 ) vs a standard aortic cannula (control; n = 132). Freedom from CNS infarction at 7 days was 32.0% with suction-based extraction versus 33.3% with control (between-group difference, −1.3%; 95% CI, −13.8% to 11.2%) and 25.6% with intra-aortic filtration vs 32.4% with control (between-group difference, −6.9%; 95%CI, −17.9% to 4.2%). Neither the 30-day composite end point (mortality, stroke or acute kidney injury) nor mortality were significantly different between the three groups. Mortality and overall serious adverse events at 90 days was also not significantly different. The authors concluded that these cerebral embolic protection devices did not significantly reduce the risk of CNS infarction at 7 days compared with standard aortic cannulation.
Cardiac Imaging
Summarised by Sarah Catchpoole
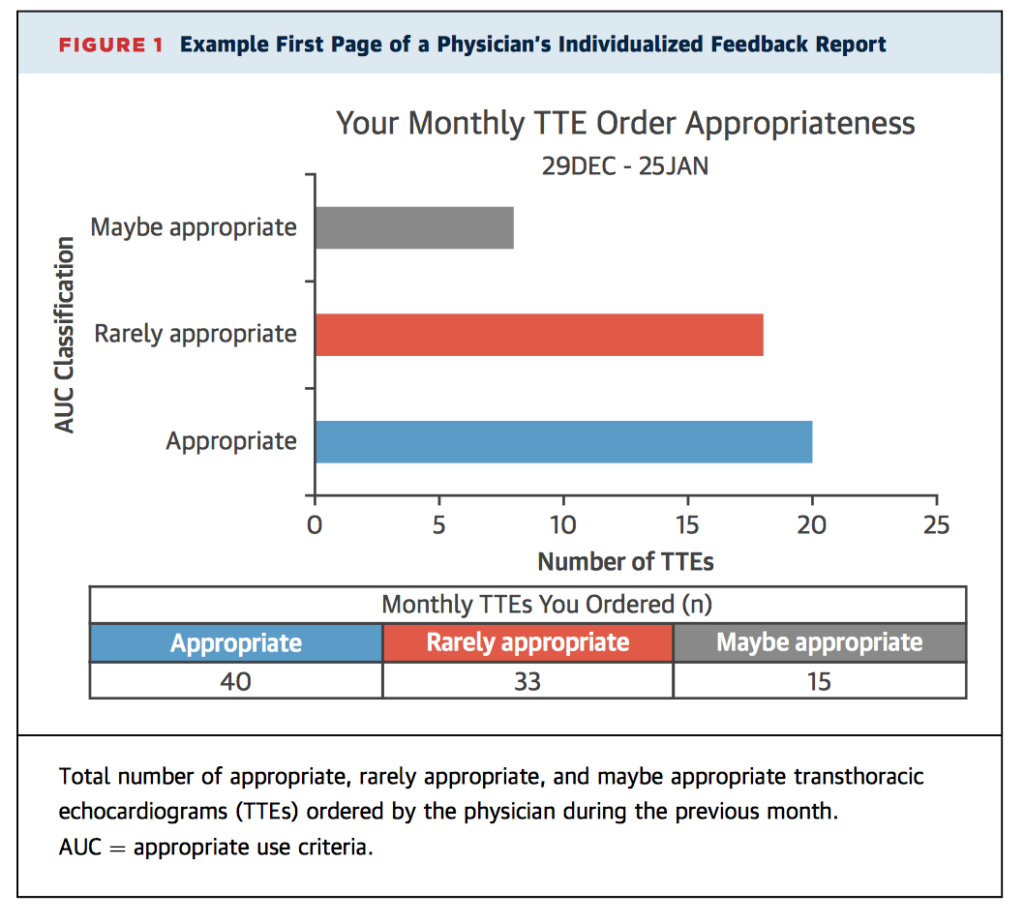
Reserving costly investigations for cases with appropriate indications is becoming increasingly important in health-care systems of limited resources. This multicentre, blinded, prospective, randomised controlled trial examined the effectiveness of an educational intervention on the amount of transthoracic echocardiograms (TTE) ordered by 179 physicians in an outpatient setting over period of 16 months. In the intervention arm, physicians received electronic educational resources on appropriate use of TTE, together with a monthly individual feedback report (Figure). Of the 14 697 TTEs ordered, the number assessed as rarely appropriate was significantly lower in the intervention group (8.8% vs. 10.1%; odds ratio 0.75; p=0.039).
This retrospective analysis of 135 patients compared the value of transthoracic echocardiography (TTE) with the more invasive transoesophageal echocardiography (TOE) for detection of bioprosthetic mitral valve dysfunction. Patients were clinically stable and had undergone both TTE and TOE within 6 months. The ratio of mitral inflow velocity time integral to left ventricular outflow tract velocity-time integral (VTIMV /VTILVOT) was found to be 100% sensitive and 99% specific for bioprosthesis dysfunction at values >2.5. The authors suggest the VTIMV /VTILVOT can be used to select patients to undergo further characterisation of dysfunction with TOE.
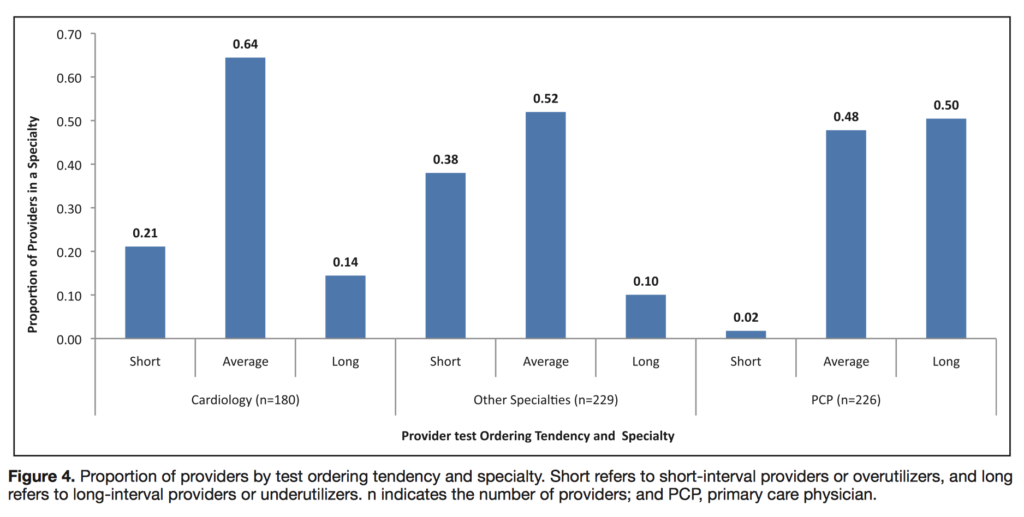
Routine surveillance of primary mitral regurgitation (MR) can help detect deterioration and guide early management decisions. The authors examined the ordering practices of physicians at a single large American centre involving 635 providers and 55 773 transthoracic echocardiograms (TTE) from 2001-2016, comparing time intervals between TTEs with best practice as per surveillance guidelines. Mixed-effects linear regression modelling revealed substantial variation in TTE follow-up intervals, with significant effects of provider specialty and experience. Overall, 25% of providers were under-utilisers and 20% of providers were over-utilisers.
Perioperative Medicine
Summarised by Andrew Haymet
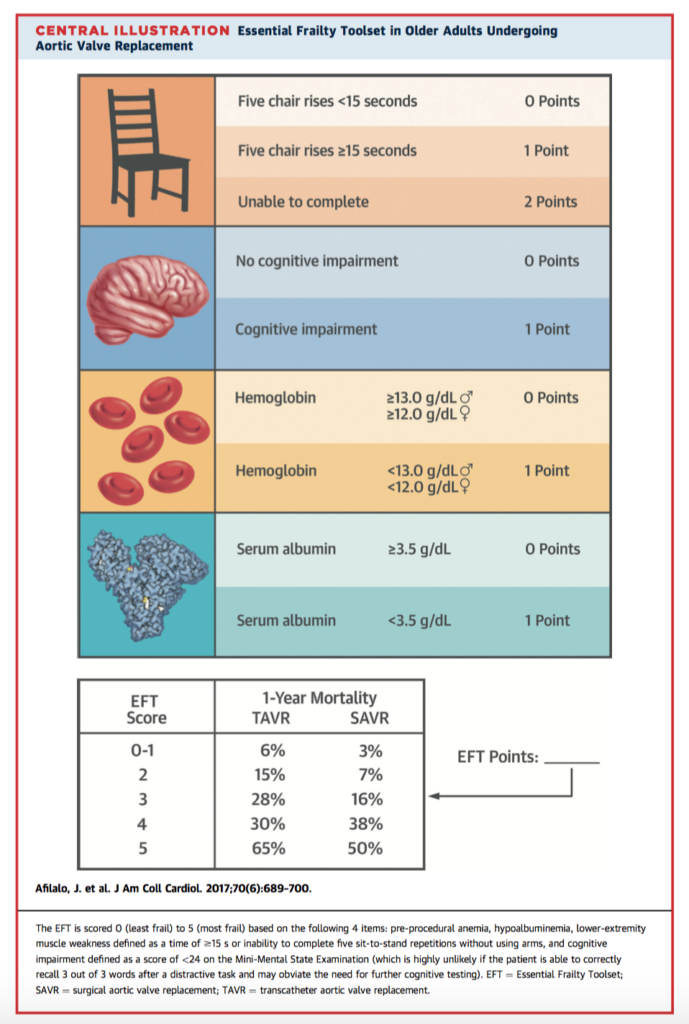
Frailty is a geriatric syndrome which diminishes potential for functional recovery, however its integration in clinical practice is confounded by the lack of a clear method to measure it. This prospective cohort study of aimed to compare the predictive value of 7 different frailty scores in 1,020 patients undergoing TAVR or SAVR. Depending on the scale used, prevalence of frailty ranged from 26% to 68%. Frailty as measured by the Essential Frailty Toolset (EFT) was the strongest predictor of death at 1 year (adjusted odds ratio [OR]: 3.72; 95% confidence interval [CI]: 2.54 to 5.45) with a C-statistic improvement of 0.071 (p < 0.001) and integrated discrimination improvement of 0.067 (p < 0.001). A brief 4-item scale encompassing lower-extremity weakness, cognitive impairment, anaemia and hypoalbuminaemia outperformed other frailty scales and is recommended for use in this application.
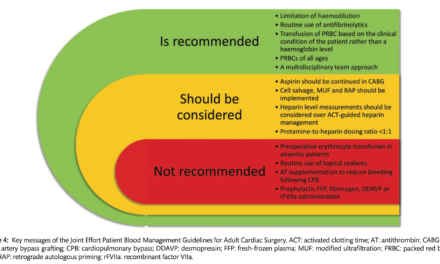
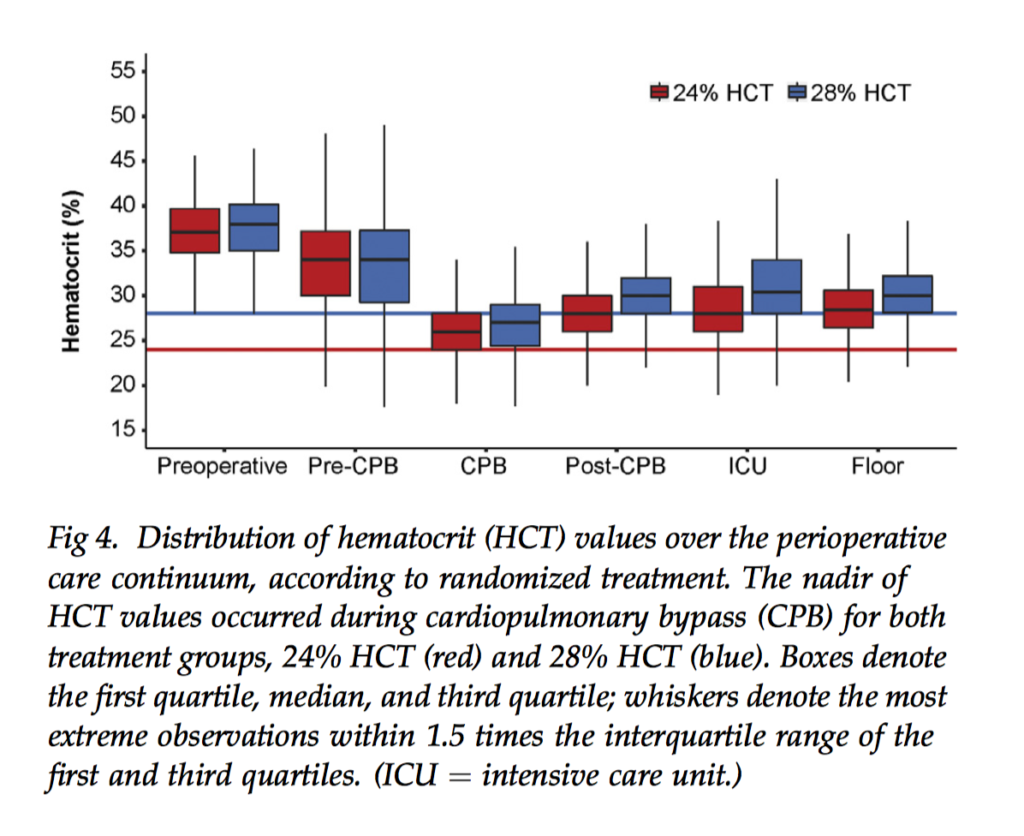
There is a lack of Class I evidence supporting a threshold for transfusion in the cardiac surgical setting. This randomized trial aimed to compare morbidity, mortality and resource use in 722 adults undergoing coronary artery bypass grafting randomly allocated to a transfusion haematocrit trigger of 24% versus 28%. There was no detected treatment effect on the composite outcome of postoperative morbidities and mortality (average relative effect odds ratio, low versus high, 0.86, 95% confidence interval: 0.29 to 2.54, p=0.71). However, the low group received fewer red blood cell transfusions than the high group (54% versus 75%, p < 0.001). The authors concluded that because red blood cell use was less with a 24% trigger without adverse effects, aggressive blood conservation efforts in cardiac surgery are warranted.
Low cardiac output drives substantial morbidity and mortality in the postoperative course of paediatric patients undergoing congenital cardiac surgery. Levosimendan, a calcium sensitizer, generates more energy-efficient myocardial contractility than with catecholamines. Five randomized controlled trials were included in this study, enrolling 212 participants, to assess whether levosimendan was a favourable postoperative prophylactic alternative to standard treatment to avoid low cardiac output syndrome. Levosimendan showed no clear effect on risk of mortality (risk ratio (RR) 0.47, 95% confidence interval (CI) 0.12 to 1.82; participants = 123; studies = 3) and no clear effect on low cardiac output syndrome (RR 0.64, 95% CI 0.39 to 1.04; participants = 83; studies = 2) compared to standard treatments. Quality of evidence was low according to the GRADE approach. The current level of evidence is insufficient to judge whether prophylactic levosimendan prevents low cardiac output syndrome and mortality in paediatric patients undergoing surgery for congenital heart disease.