Summarised by Andrew Haymet
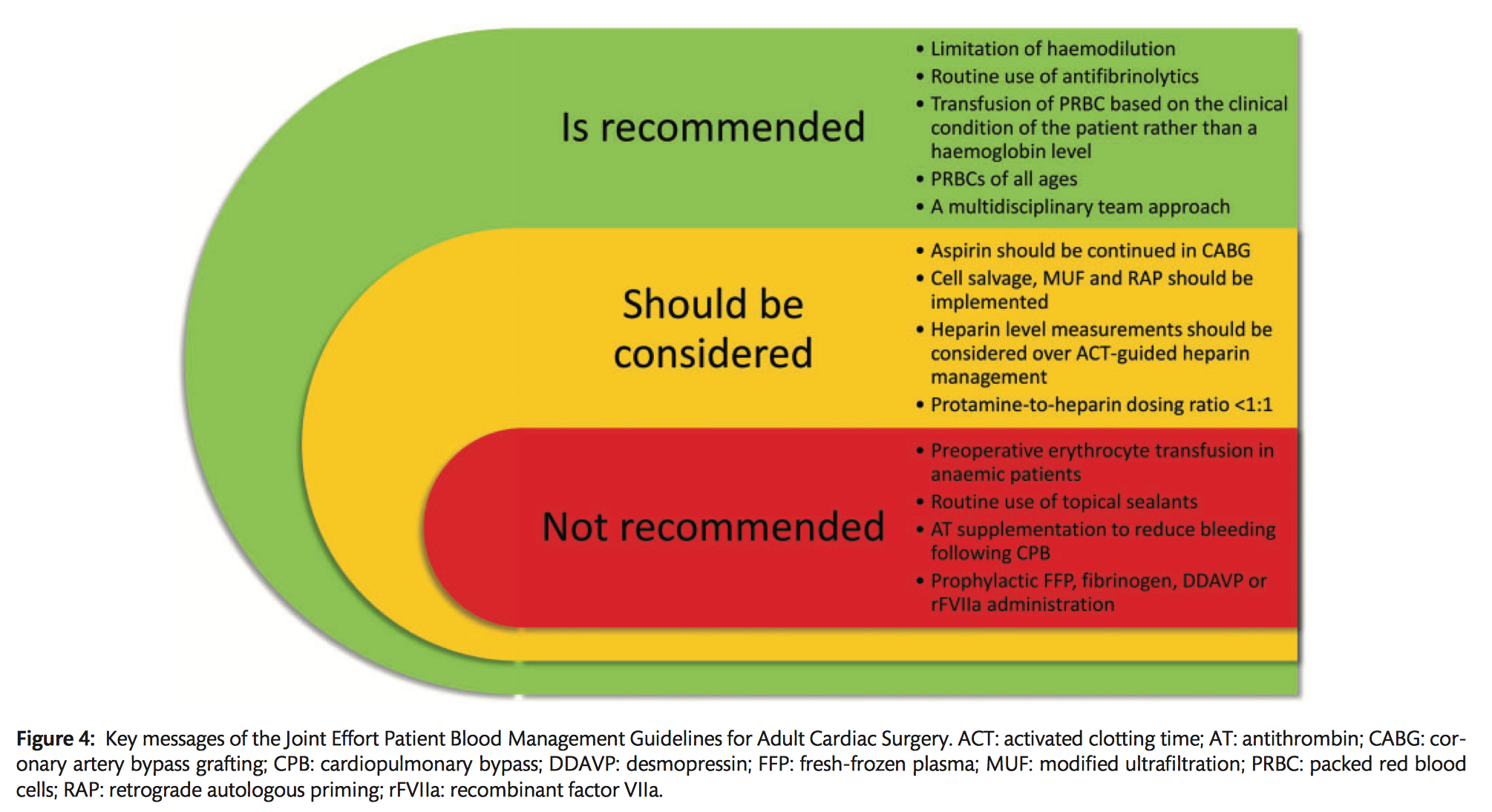
This joint EACTS/EACTA publication provides a series of evidence based recommendations with regard to patient blood management in cardiac surgery.
Preoperative management
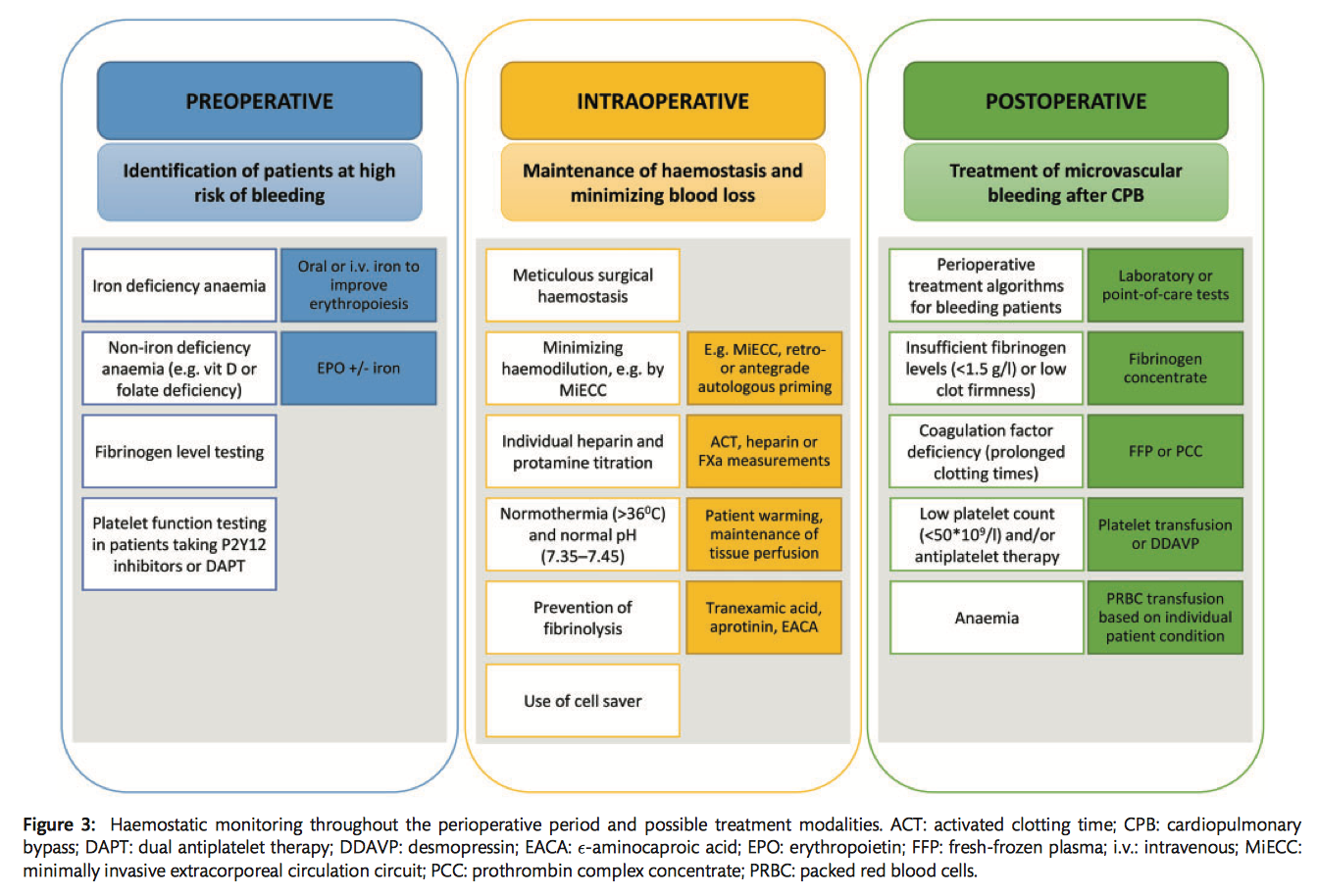
- There is no association between preoperative prothrombin time (PT) or activated partial thromboplastin time (APTT) and perioperative blood loss or transfusion requirements. The most commonly identified risk factor for postoperative bleeding is a low fibrinogen level. Whilst preoperative fibrinogen levels and thrombin generation assays may be considered to identify patients at high risk of bleeding (eg aortic/emergency surgery) thrombin generation assays are not yet validated for routine clinical usage (Class IIb C).
- Preoperative platelet function may be used to guide the timing of surgery for patients on dual antiplatelet therapy (DAPT), but not in patients without ongoing or recently stopped DAPT (Class IIb B).
Preoperative anticoagulant/antiplatelet drugs
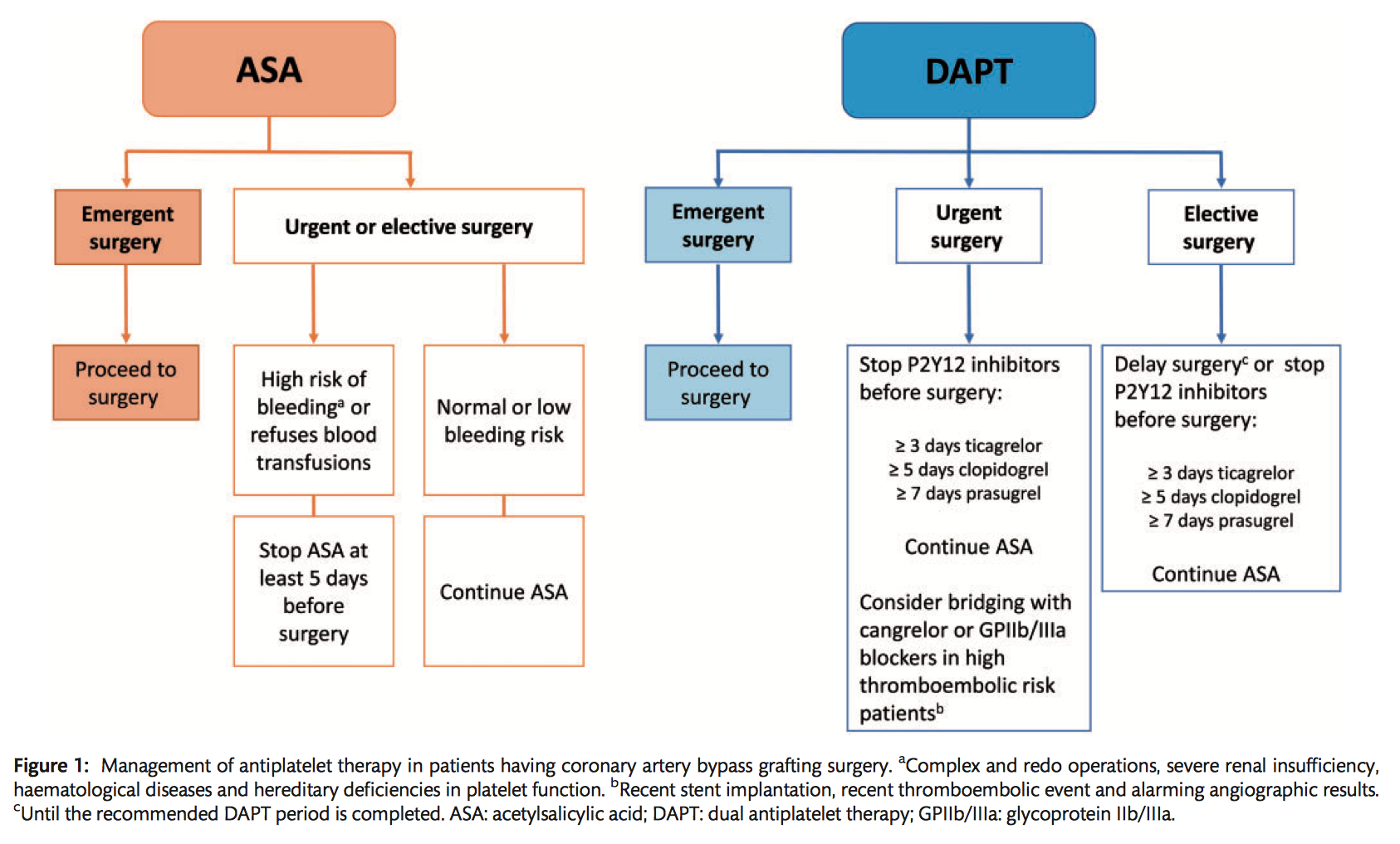
- Acetylsalicylic acid agents (ASA, eg aspirin) are recommended to be continued before cardiac surgery, and if discontinued, should be given to all patients having CABG as soon as there is no concern over bleeding to prevent thromboembolic complications (Class IB).
- With regard to DAPT in patients awaiting nonemergent cardiac surgery, postponement of surgery for at least 3 days after discontinuation of ticagrelor, 5 days after clopidogrel and 7 days after prasugrel should be considered to reduce the risk of postoperative bleeding. ASA therapy should be continued whilst P2Y12 inhibitors are being withheld (Class IIa B).
- GPIIb/IIIa inhibitor discontinuation should be considered at least 4 hours before surgery to minimize the risk of postoperative bleeding (Class IC).
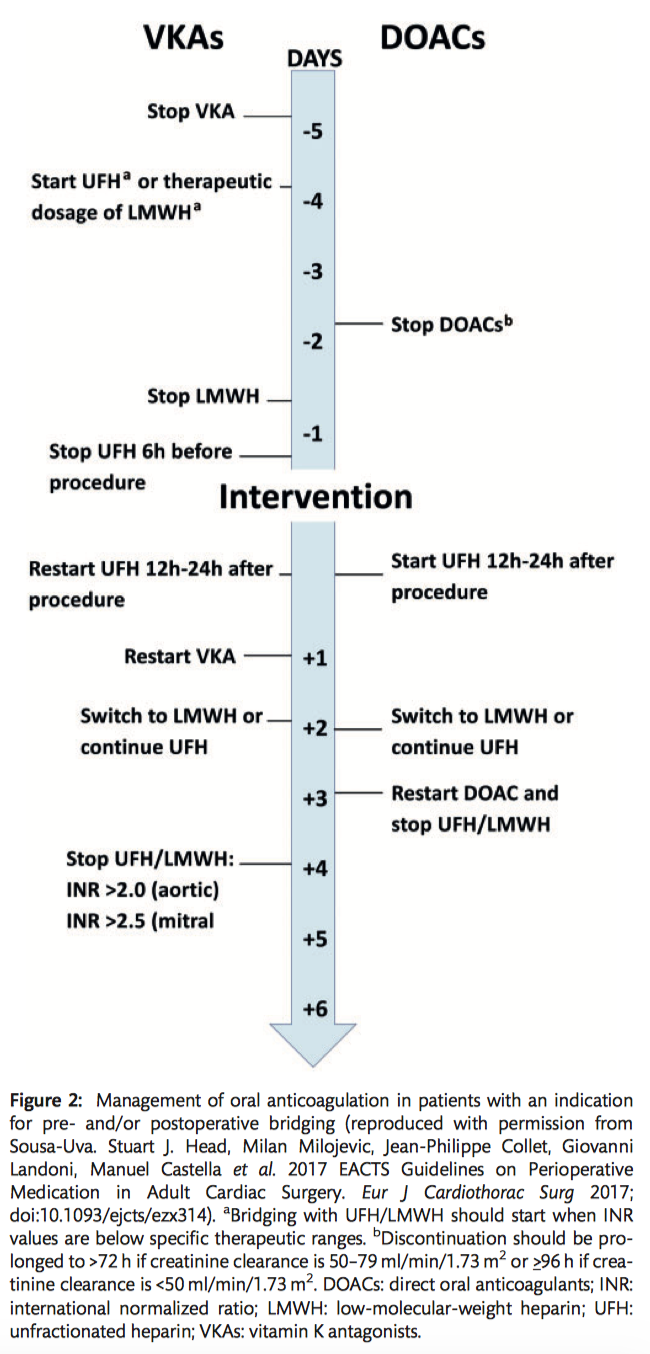
- Preoperative bridging of oral anticoagulation with unfractionated heparin (UFH)/low molecular weight heparin (LMWH) is only indicated in patients at high risk of thrombotic events. Prophylactic LMWH should be discontinued 12 hours, and fondaparinux 24 hours, before surgery. Longer intervals may be required in patients with impaired renal function (Class IB).
- Vitamin K antagonists are commonly used to prevent and treat thromboembolism in patients with atrial fibrillation, venous thromboembolic disease and mechanical heart valves (especially mitral or tricuspid). Anticoagulatin effect is monitored with prothrombin time and expressed as an international normalized ratio (INR). VKAs are usually stopped 3-5 days before surgery to obtain an INR of 1.5. In emergent settings, VKA reversal may be performed with prothrombin complex concentrate (PCC). Bridging to cardiac surgery is only recommended in patients at a very high risk of thrombotic events (eg recent (<4weeks) pulmonary embolism, prosthetic valve, atrial fibrillation with rheumatic valvular disease or AF with CHA2DS2-VASC score >4. In these patients, VKA should be stopped 5 days preoperatively and bridged with LMWH (Class IIa C).
- Direct oral anticoagulants (DOACs, eg dabigatran, rivaroxaban, apixaban or edoxaban) should be ceased at least 48 hours prior to surgery due to their association with severe or fatal bleeding in emergency surgery. DOACs may be bridged by heparins with acute thrombotic events <4 weeks (Class IIaC).
Preoperative anaemia
- According to retrospective studies, preoperative anaemia is considered a risk factor for adverse clinical outcomes such as acute kidney injury and death, as well as greater blood transfusion requirements. Iron supplementation may reduce transfusion requirements in patients undergoing cardiac surgery with iron deficiency anaemia, however the optimal time to begin supplementation is not clear (Class IIb C).
- Erythropoetin (EPO) with or without iron supplementation should be considered in patients with non-iron deficiency anaemia undergoing elective surgery to reduce postoperative transfusion requirements. Benefits of an EPO infusion may be conferred up to several days before surgery (Class IIa B).
- Preoperative blood transfusions are not routinely recommended for patients with preoperative anaemia, except in emergency surgery or cases of life threatening anaemia (Class IIIC).
Intraoperative management
- For severely anaemic patients, it is recommended that members of the multidisciplinary team (cardiologists, surgeons, anaesthetists and perfusionists) discuss optimal strategies, including surgical techniques, the limitations of haemodilution and improved CPB systems to avoid massive transfusions and bleeding (Class IC).
- Off-pump surgery may be considered a technique associated with fewer transfusion requirements compared to on-pump surgery (Class IIb B).
- Minimally invasive extracorporeal circulation circuits (MiECC) compared with traditional CPB circuits are associated with reduced PRBC transfusions (Class IIa B).
- Until minimally invasive surgery becomes more widely adopted and large RCTs are performed, there is not enough evidence to suggest broad adaption for the purpose of blood conservation (Class IIb B).
- The routine use of topical sealants in cardiac surgery is not recommended and may be considered in cases of persistent bleeding which is localized (Class III B).
Cardiopulmonary bypass (CPB)
- Implementation of institutional measures to reduce haemodilution by fluid infusion and CPB during cardiac surgery to reduce the risk of bleeding and the need for transfusions is recommended (Class IC).
- Closed extracorporeal circulation circuits (ECC) may reduce bleeding and transfusions, but adequately sized RCTs are lacking (Class IIb B).
- The use of a biocompatible coating may be considered within circuit tubing to reduce perioperative bleeding and transfusions (Class IIb B).
- The routine usage of cell salvage should be considered to prevent transfusions, but the retransfusion of large volumes of cell salvaged blood (>1000mL) may impair coagulation (Class IIa B).
- Modified ultrafiltration may be considered as part of a blood conservation strategy to minimize haemodilution (Class IIb B).
- Retrograde and antegrade autologous priming should be considered as part of a blood conservation strategy to reduce transfusions (Class IIa A).
- Normothermia during CPB (temperature >36 degrees C) and maintenance of a normal pH (7.35–7.45) may contribute to a reduced risk of postoperative bleeding (Class IIb B).
Intraoperative anticoagulation
- Antithrombin (AT) supplementation is indicated in patients with AT deficiency to improve heparin sensitivity (Class I B).
- Heparin level-guided heparin management should be considered over ACT-guided heparin management to reduce bleeding (Class IIa B).
- Protamine should be administered in a protamine-to-heparin dosing ratio <1:1 to reduce bleeding (Class IIa B)
- Heparin level-guided heparin management should be considered over ACT-guided heparin management to reduce bleeding (Class IIa B)
- AT supplementation is not recommended to reduce bleeding following CPB (Class III C).
- In patients with HIT antibodies for whom surgery cannot be postponed, anticoagulation with bivalirudin should be considered when the bleeding risk is acceptable. The use of heparin in the pre- and postoperative periods should be avoided (Class IIa C).
Intravascular volume
- Limitation of haemodilution is recommended as part of a blood conservation strategy to reduce bleeding and transfusions (Class I B).
- The use of goal-directed haemodynamic therapy to reduce transfusions is not recommended (Class III C)
- The use of modern low-molecular weight starches in priming and non-priming solutions to reduce bleeding and transfusions are not recommended (Class III C).
- Preoperative autologous blood donation in patients with high haemoglobin levels (>110g/dL) may be considered to reduce postoperative transfusions (Class IIb B).
- Acute normovolaemic haemodilution may be considered to reduce postoperative transfusions (Class IIb B).
Procoagulant interventions
- Antifibrinolytic therapy (TXA, aprotinin and EACA) is recommended to reduce bleeding and transfusions of blood products and reoperations for bleeding (TXA and aprotinin) (Class IA).
- The prophylactic use of FFP to reduce bleeding is not recommended (Class IIIB).
- The use of PCC or FFP may be considered to reverse the action of VKAs (Class IIb B).
- In patients with factor XIII activity <70% after CPB, the administration of factor XIII may be considered to reduce bleeding (Class IIb B).
- Prophylactic fibrinogen administration is not recommended (Class III B).
- In the bleeding patient with a low fibrinogen level (<1.5 g/l), fibrinogen substitution may be considered to reduce postoperative bleeding and transfusions (Class IIb B).
- In patients where bleeding is related to coagulation factor ciency, PCC or FFP administration should be considered to reduce bleeding and transfusions (Class IIa B).
- The prophylactic use of DDAVP to reduce bleeding is not recommended (Class III B).
- In bleeding patients with platelet dysfunction on the basis of an inherited or acquired bleeding disorder, the use of DDAVP should be considered to reduce bleeding and the requirement for transfusions (Class IIa C).
- The prophylactic use of rFVIIa to prevent bleeding is not recommended (Class III B).
- In patients with refractory, non-surgical bleeding, off-label use of rFVIIa may be considered to reduce bleeding (Class IIb B).
Transfusion strategies
- Implementation of a PBM protocol for the bleeding patient is recommended (Class I C).
- The use of PRBCs of all ages is recommended, because the storage time of the PRBCs does not affect the outcomes (Class I A).
- The use of leucocyte-depleted PRBCs is recommended to reduce infectious complications (Class I B).
- Pooled solvent detergent FFP may be preferred to standard FFP to reduce the risk of TRALI (Class IIb B).
- Perioperative treatment algorithms for the bleeding patient based on viscoelastic POC tests should be considered to reduce the number of transfusions (Class IIa B).
- It is recommended that one transfuse PRBCs on the basis of the clinical condition of the patient rather than on a fixed haemoglobin threshold (Class I B).
- A haematocrit of 21-24% may be considered during CPB when an adequate DO2 (>273 mL O2/min/m2) level is maintained (Class IIb B).
- Platelet concentrate should be transfused in bleeding patients with a platelet count below 50 x109/L or patients on anticoagulant therapy with bleeding complications (Class IIa C).
Anticoagulation management during extracorporeal life support
- Bivalirudin and argatroban may be considered as alternatives for heparin anticoagulation for prolonged ECLS/ECMO therapy to prevent HIT type 2 (Class IIb C).











