Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been recently published in each speciality (Cardiology, Cardiac Surgery, Cardiac Imaging, Perioperative Medicine).
Cardiology
Summarised by Dr Sarah Catchpoole/Dr Michael Seco
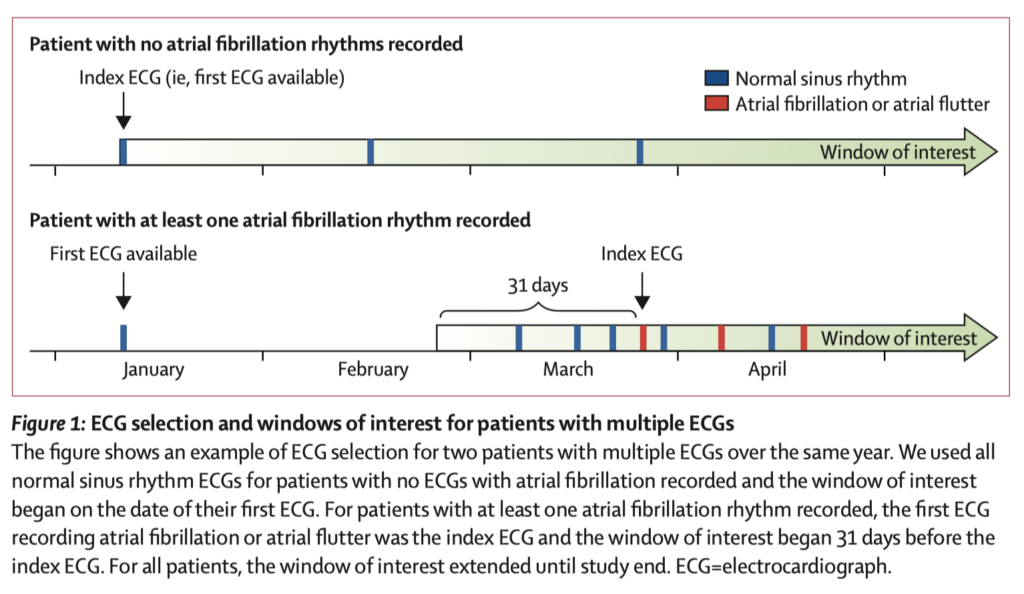
The authors have developed an AI model that can detect the electrocardiographic signature of AF present rhythm during a normal sinus ECG. They did this by taking all patients with at least one sinus rhythm ECG at the Mayo Clinic, identifying those with another showing atrial fibrillation or flutter, and using these to train a convolutional neural network. Using a single ECG, the AI was able identify AF with an AUC of 0.87 and overall accuracy of 79.4%. Using all of a patient’s ECGs a month before the first recorded AF episode improved the accuracy further (AUC to 0.90, overall accuracy to 83.3%). To put this in context, BNP for heart failure has an AUC of 0.60–0·70, and CHA2DS2-VASc Score for stroke AUC 0.57–0.72.
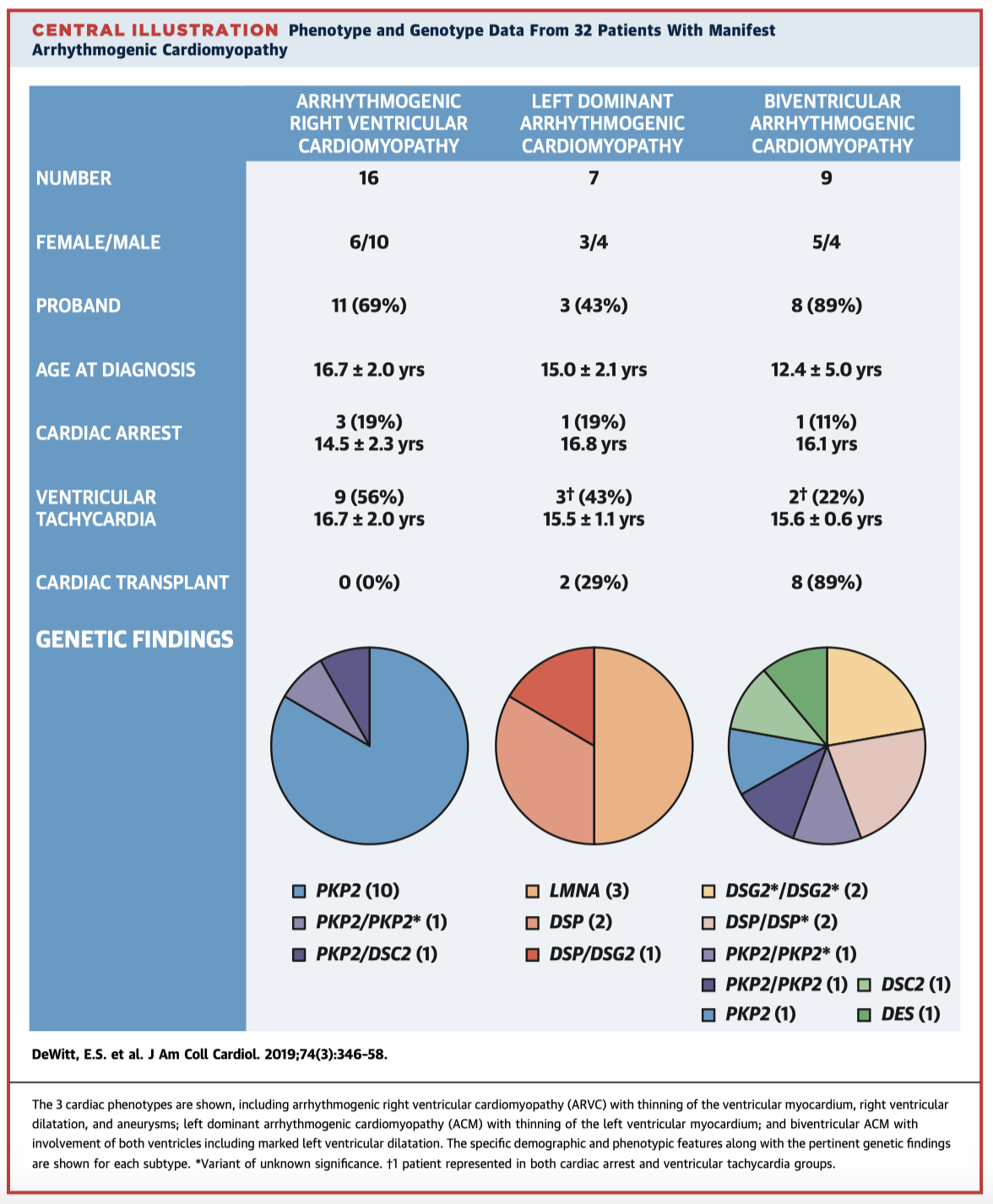
Arrhythmogenic cardiomyopathy (ACM) is caused by mutations in cardiac desmosomal proteins and typically presents in the fourth decade of life. Rare cases present from childhood, however only case series have previously been reported in the literature. Here the authors have accessed databases at the Boston Children’s Hospital for cases of ACM initially presenting <21 years of age. Manifest disease was evident in 32 patients (22 probands). The phenotypical characteristics and genotypes are summarised below (Central Illustration). Given the variability in disease expression, potential for life-threatening complications, and implications for familial screening, the authors stress the need to maintain a high clinical index of suspicion for ACM in younger populations.
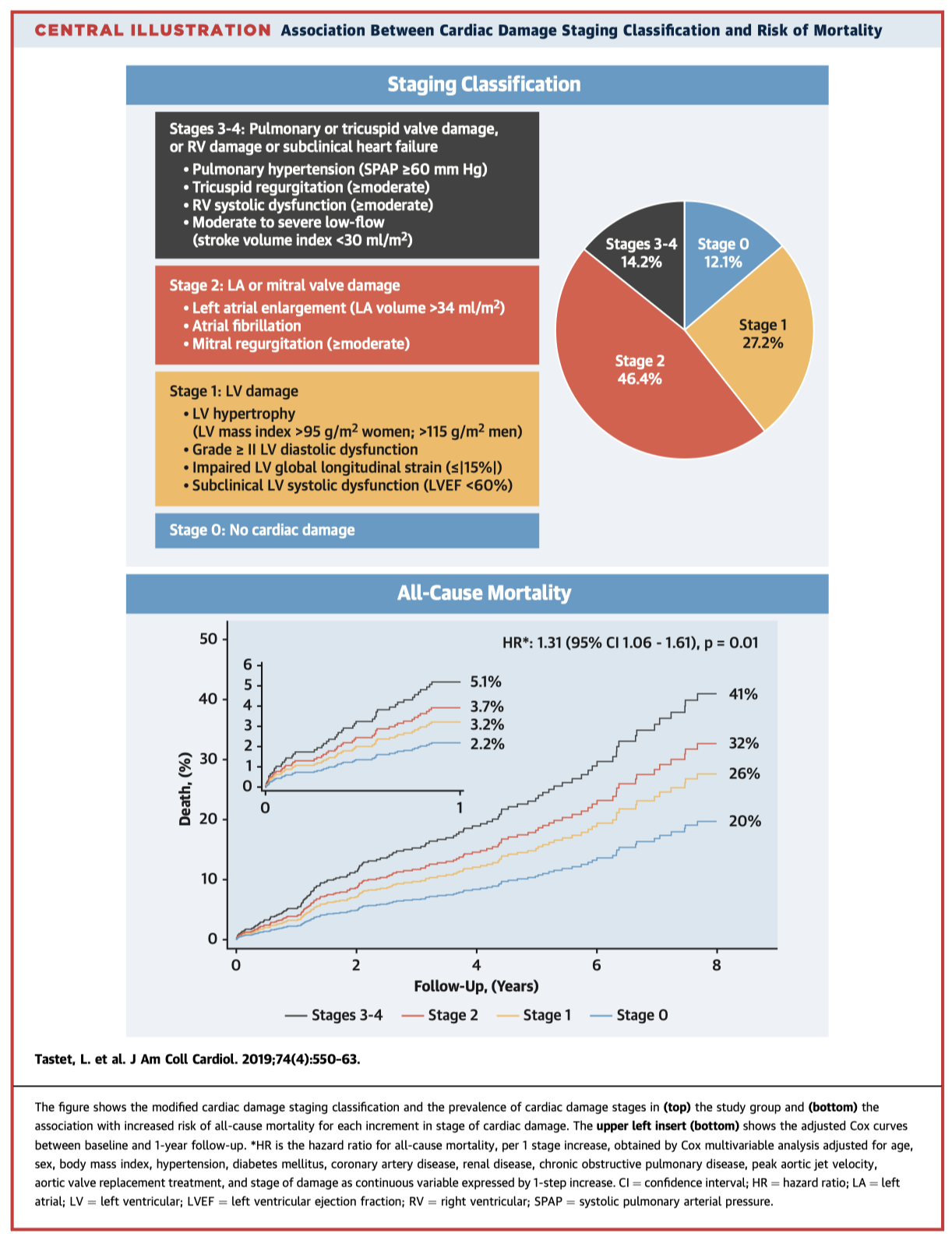
This follows a recent article looking at staging cardiac damage in patient with symptomatic severe AS. In this article they have applied a similar classification of cardiac damage (Stages 0-4) to asymptomatic patients with moderate-severe AS. Over a median follow-up of 2.6 years, they demonstrated a stepwise increase in mortality according to stage (58% in stages 3 & 4). The predictive significance of their staging system was confirmed with multivariable analysis. This system may therefore be useful in determining the timing of aortic valve intervention in these patients.
Cardiac Surgery
Summarised by Dr Michael Seco
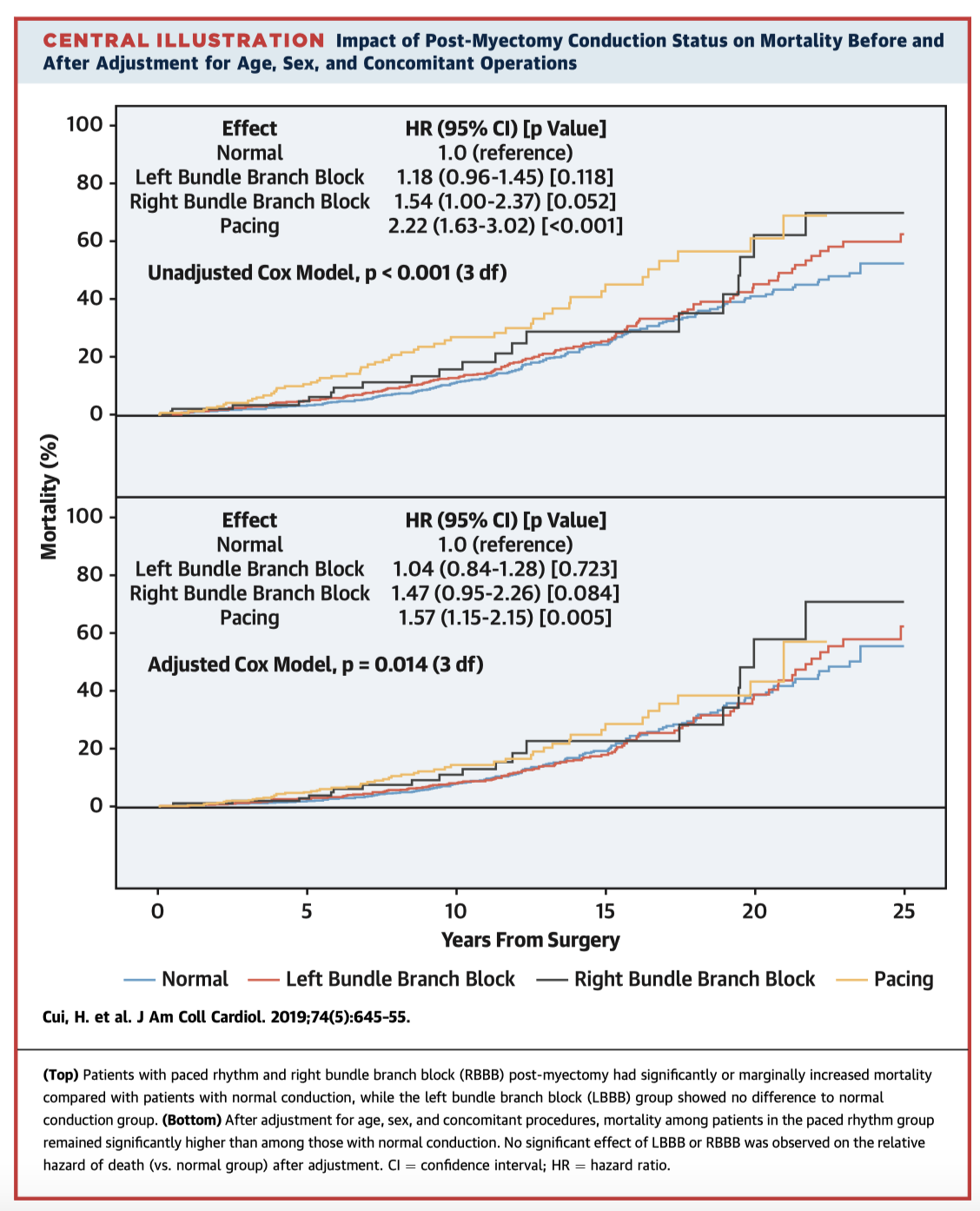
This study looked a very large cohort of septal myectomy patients over a median follow-up time of 8.6 years. In patients who had normal conduction preoperatively, 38.8% developed LBBB, 1 .1% developed RBBB, & 0.6% developed CHB postoperatively. In patients with RBBB preoperatively, 34.8% developed CHB postoperatively – a significantly higher proportion. Mortality was significantly higher in patients needing pacing (HR. 1.75, 95CI 1.15-2.14), but there was no difference in mortality with LBBB or RBBB.
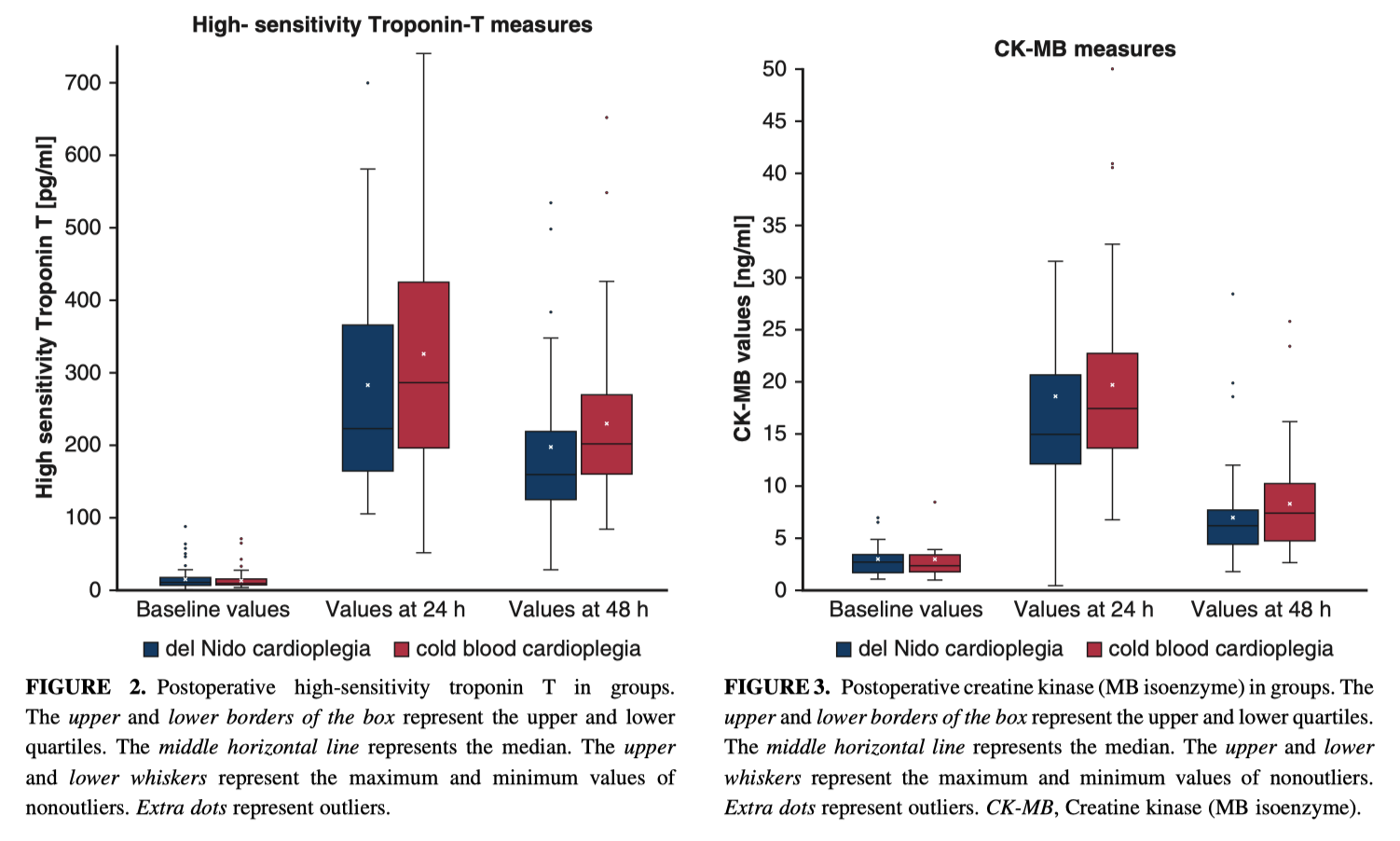
This trial randomised 150 patients undergoing AVR to receive del Nido cardioplegia (every 90min) vs cold blood cardioplegia (every 20-30min or electrical activity). Rates of electrical activity during cross-clamp were similar. VF after removing the clamp occurred less frequently in the del Nido group (22.7% vs 54.7%; RR 2.41, p significant). Postoperative troponin and CK-MB levels were not significantly different. Therefore de Nido appeared to be an acceptable alternative to cold blood cardioplegia for myocardial protection.
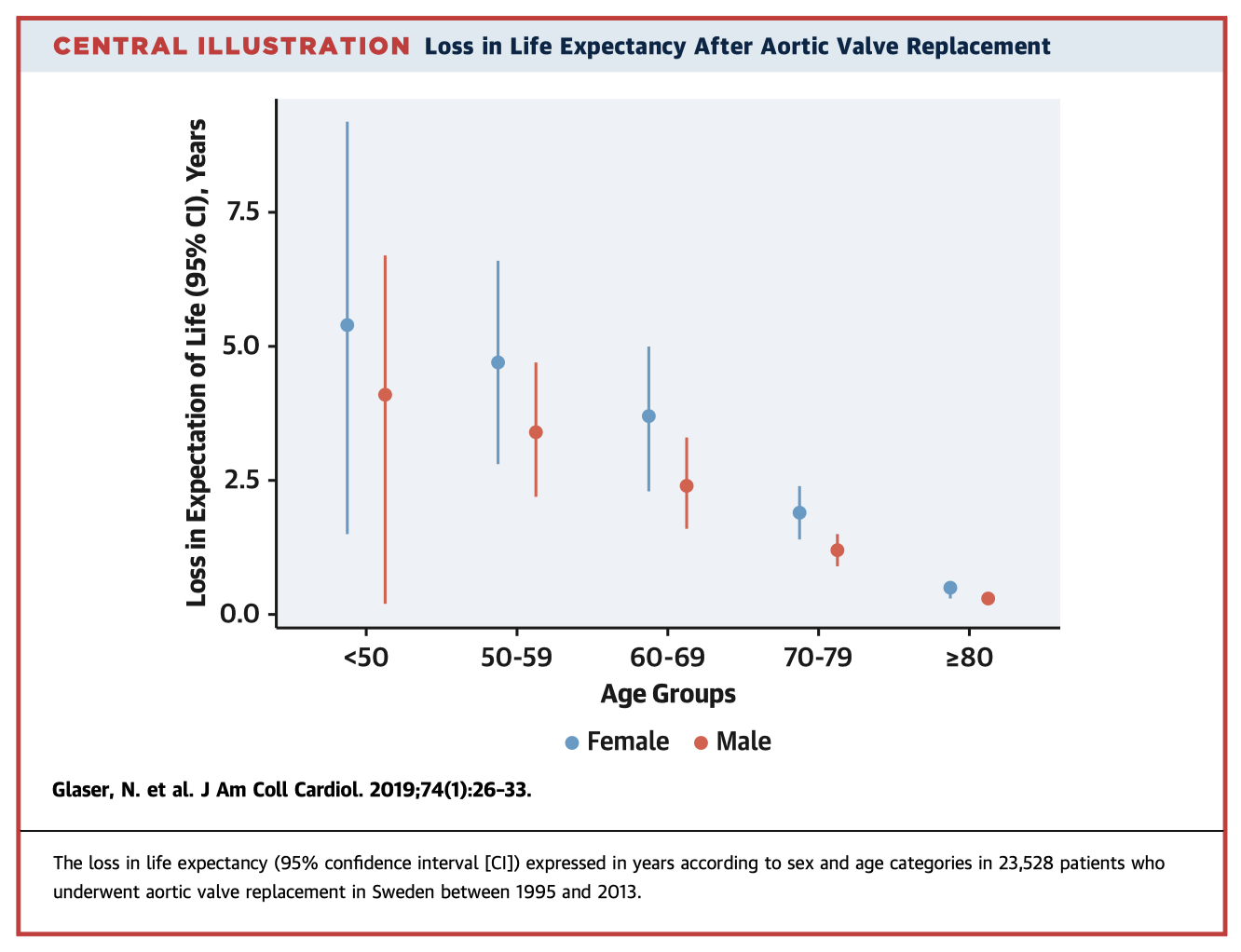
The SWEDEHEART study is nationwide registry of all cardiac surgery in Sweden since 1992. In this analysis they have included 23,528 patient who underwent primary surgical AVR +/- CABG. The mean follow-up time was 6.8 years. The 19-year observed, expected, and relative survival was 21%, 34%, and 63%, respectively. Compared to the general Swedish population (age, sex & year of surgery matched), there was a loss of life expectancy of 1.9yrs. The loss of life expectancy was higher in younger patients (4.4yrs in <50 year olds, and 0.4yrs in ≥80 year olds). There was no difference between men & women.
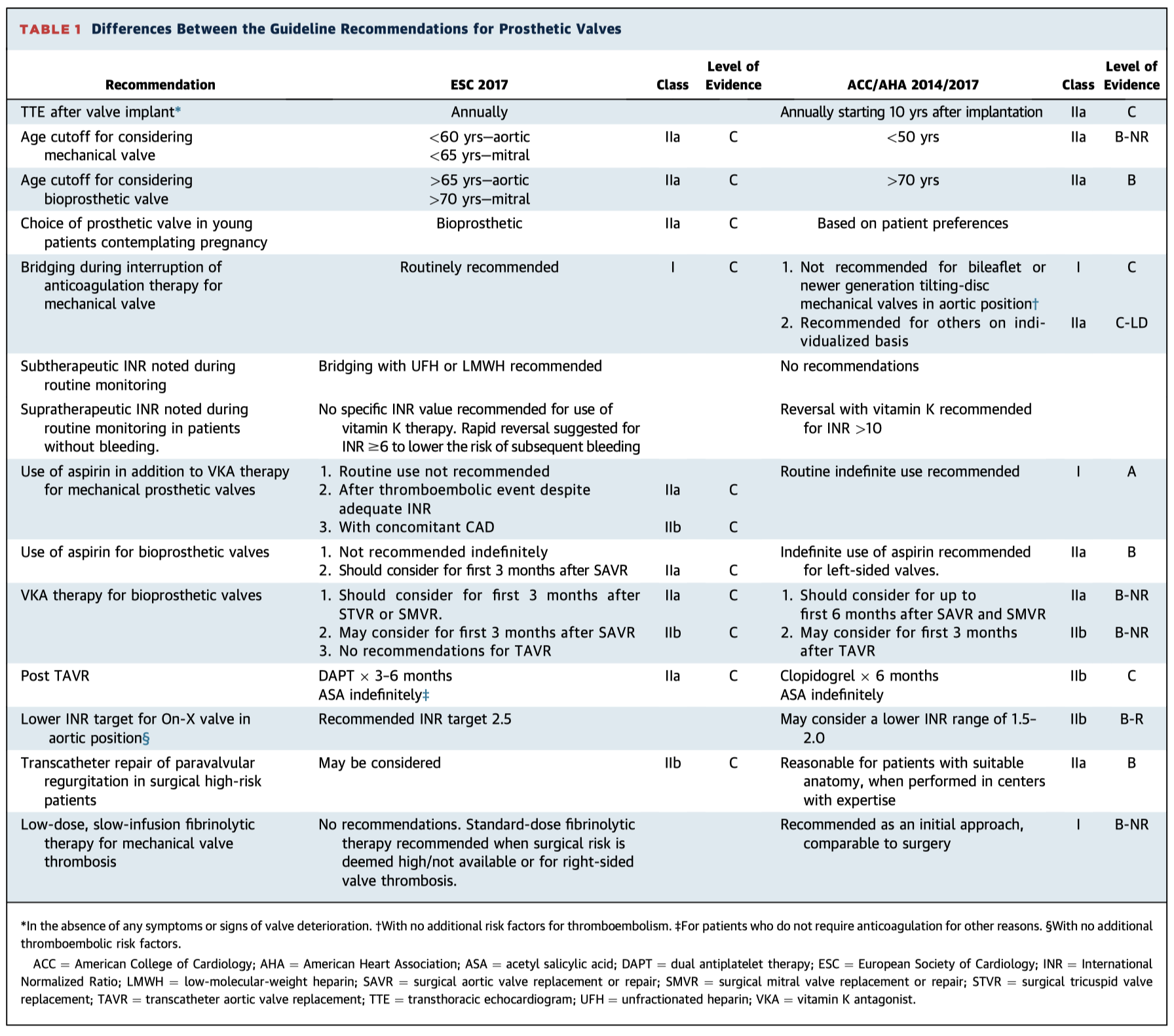
This is a highly useful article comparing the American and European guidelines on prosthetic heart valves, both from 2017. They differ in age recommendations for bioprosthetic vs mechanical prostheses, anticoagulation therapy, role of aspirin and more. Table 1 below has a useful summary.
See also comparisons of Heart Failure, Hypertension, NSTE-ACS, and DAPT guidelines.
Cardiac Imaging
Summarised by Dr Sarah Catchpoole
Optimal sizing of left atrial appendage (LAA) occlusion devices is crucial for procedural success, but is complicated by the complex and variable anatomy of the LAA. In this paper, the authors demonstrate improved outcomes using individual, 1:1 scale, 3D printed models of the LAA. For the 72 patients in the retrospective cohort, post hoc 3D models were created and compared to the size of the actual device implanted. Where there was mismatch between the 3D model and in vitro device, there were significantly higher rates of poor procedural outcomes and complications including device thrombus, ischaemic stroke, and death over 3 ± 2.3 years of follow-up. In the prospective cohort, a 3D printed model was used to guide device sizing prior to implantation. For these patients (n=32), there were significantly higher procedural success rates and shorter procedure time, with no complications over 9.4 ± 4.1 months of follow-up.
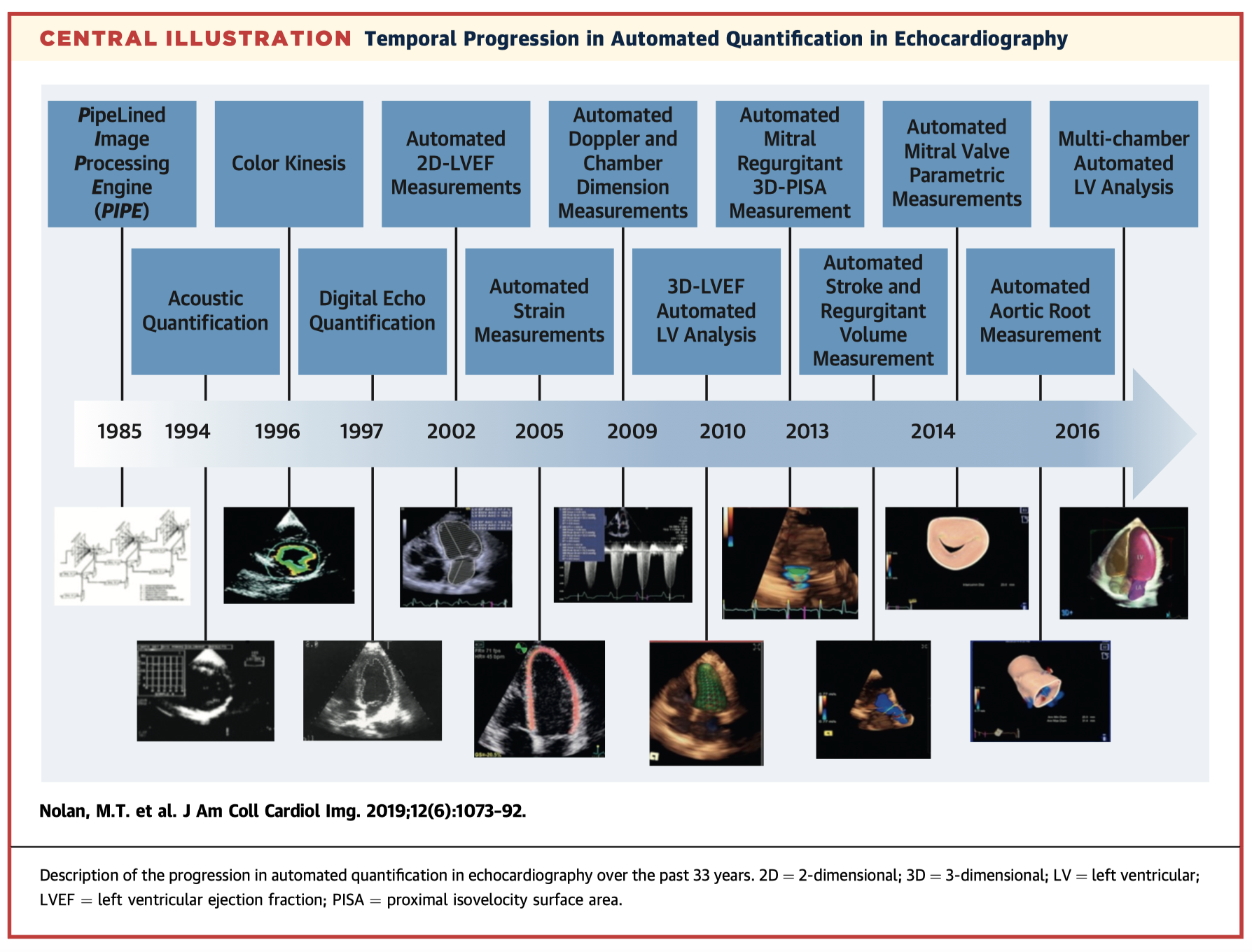
Automated measurement techniques in echocardiography are becoming increasingly sophisticated and have the potential to improve accuracy and reliability, streamline workflows, and reduce costs. However, uptake in clinical practice remains slow. This state-of-the-art review discusses current automated quantification techniques, their benefits and limitations including future research directions, and current barriers to wide-spread implementation.
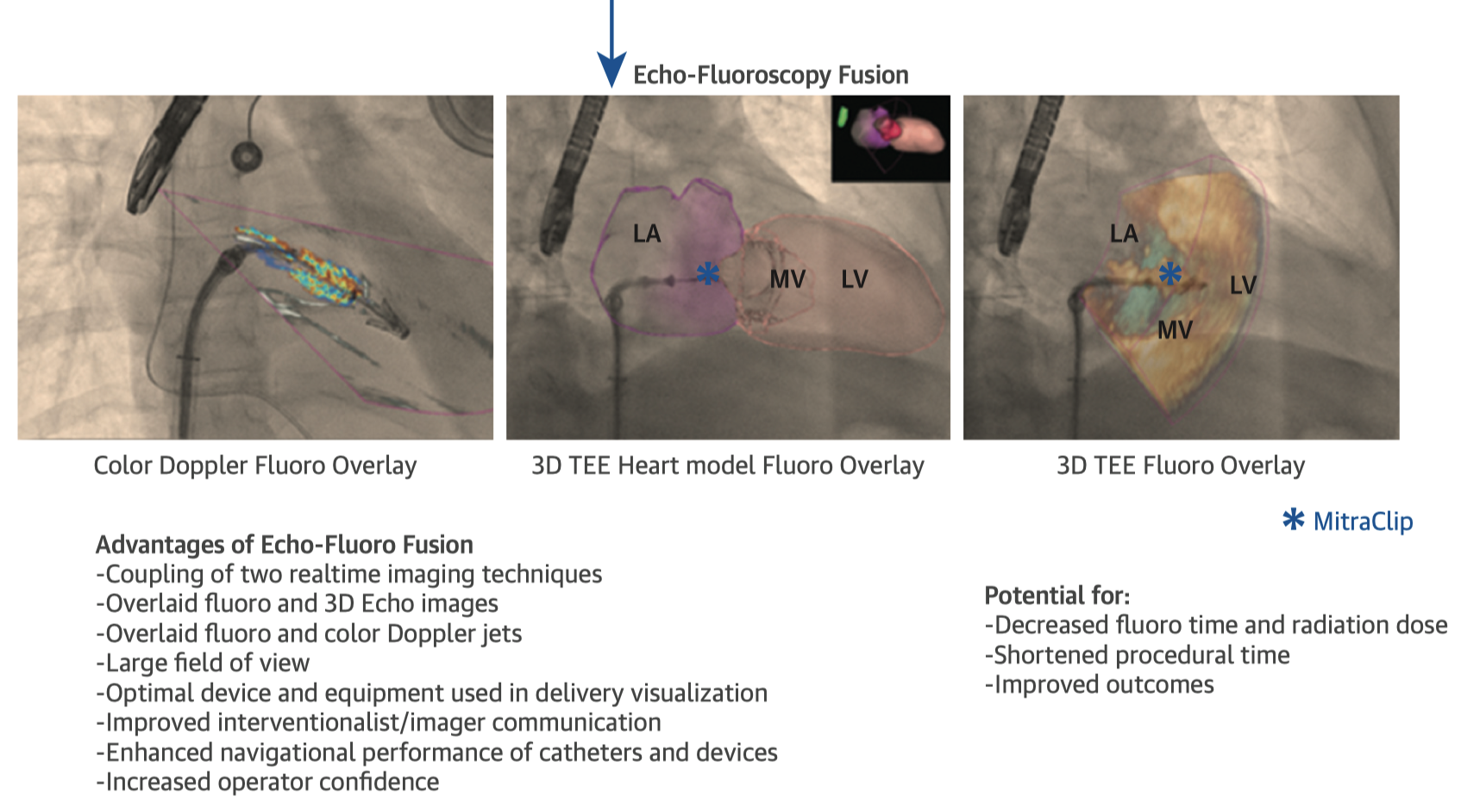
Echocardiography-fluoroscopic fusion (EFF) combines the benefits of soft-tissue and doppler information from echocardiography with the large field of view and excellent device visualisation of fluoroscopy. This brief imaging vignette demonstrates the use of EFF in a variety of catheter interventions for structural heart disease. The authors hope the technique has potential to reduce radiation doses and procedure times, as well as improve team communication and patient outcomes.
Perioperative Medicine
Summarised by Dr Andrew Haymet/Dr Michael Seco
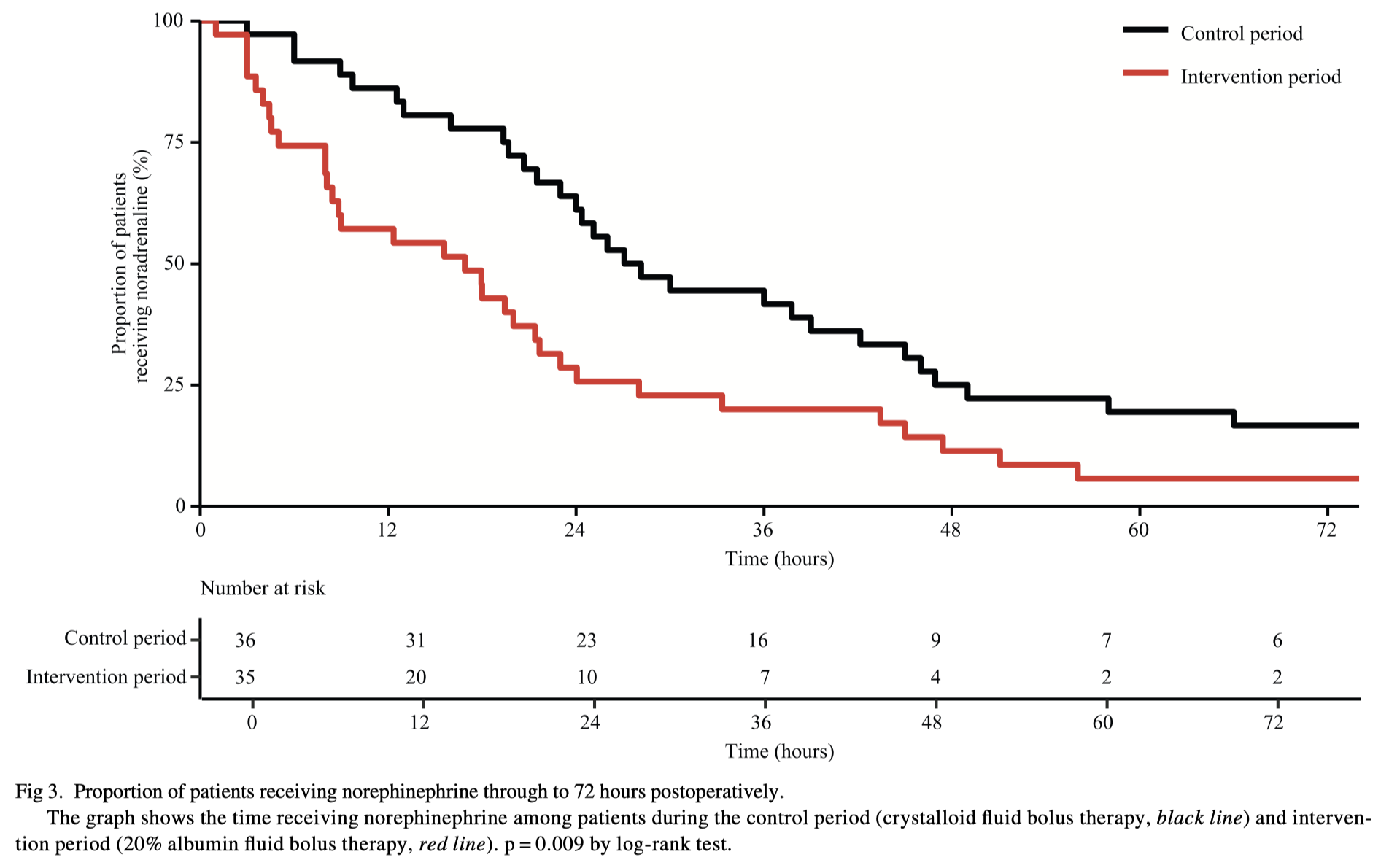
Patients often receive a large volume of fluid administration after cardiac surgery to optimize cardiac output and blood pressure. This study was designed as a ‘sequential period’, open label, pilot study to compare crystalloid bolus therapy (first 50 patients) vs up to 2x 100 mL 20% albumin boluses followed by crystalloid (second 50 patients). They found that giving the concentrated albumin reduce the fluid balance in the first 24hrs, patients needed fewer fluid boluses, and there a decrease in overall dose of noradrenaline. Given this was a pilot study further investigation is now warranted.
Letter to the Editor & Author’s Reply
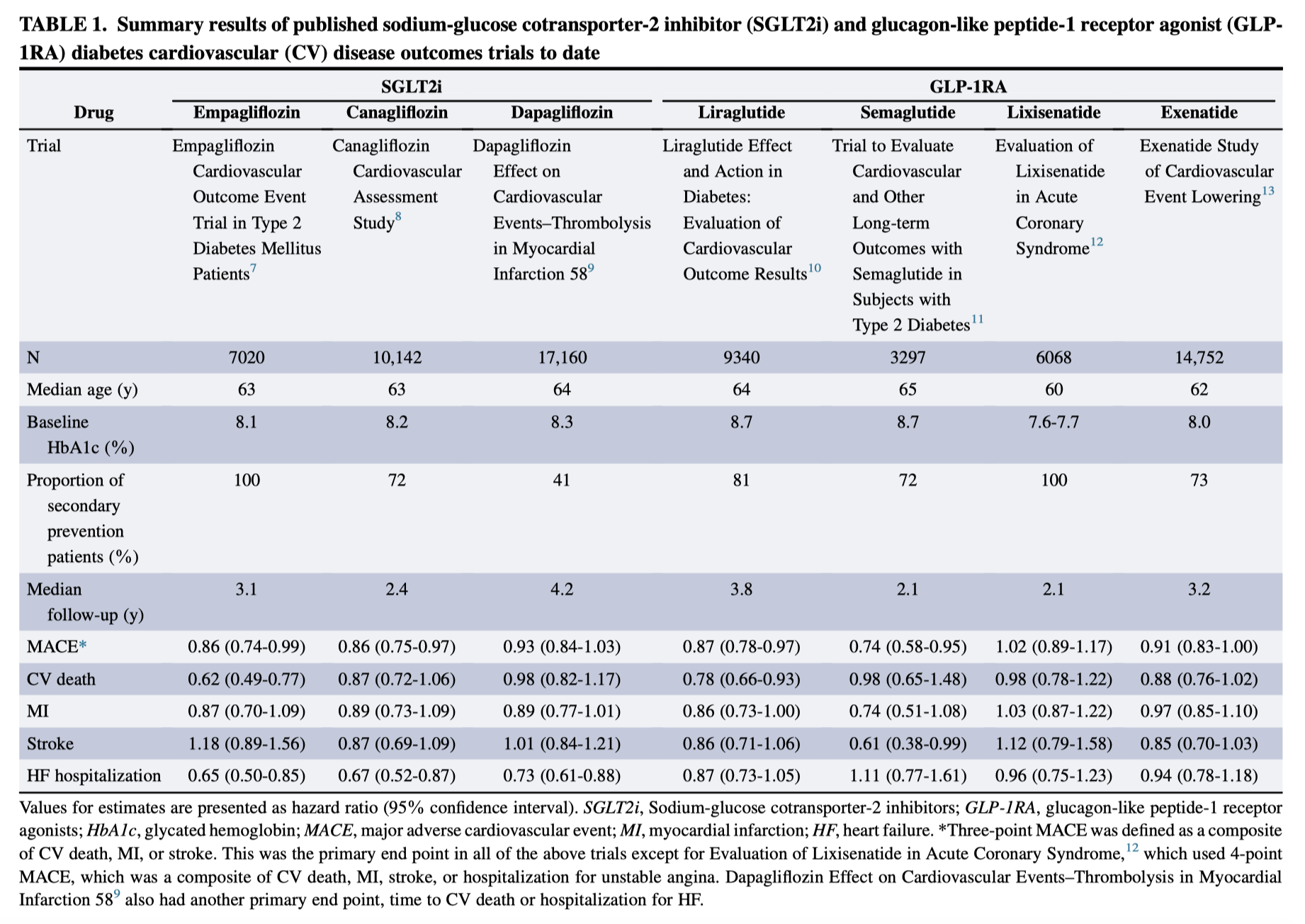
This paper is a useful summary for surgeons (and others!) of two new classes of antihyperglycaemics – SGLT2 inhibitors (inc dapagliflozin & empagliflozin) and GLP-1RAs (inc liraglutide). Both of these drug classes improve glycaemic control, and have been shown to improve cardiovascular outcomes in a number of patients groups as well. Therefore, they are likely to become much more frequent in surgical patients. Both can have potential adverse effects, and SGLT2 inhibitors in particular can cause euglycaemic ketoacidosis, that clinicians need to be aware of.
Anaemia is common in patients with cardiac disease. This review focuses on pre, intra and postoperative strategies to detect, prevent and treat anaemia as part of patient blood management (PBM) in cardiac surgery. PBM aims to reduce perioperative blood loss, the need for RBC transfusion, morbidity, length of hospital stay, costs, and in-hospital mortality. Preoperative anaemia in cardiac surgery patients is an independent risk factor for transfusion of RBC, postoperative morbidity, and mortality. A relevant proportion of anaemic patients in cardiac surgery shows potential for preoperative anaemia therapy, particularly by iron supplementation. Prevention of intraoperative anaemia includes the use of cell salvage and autologous blood retransfusion, and blood saving techniques. Postoperative anaemia management comprises postoperative iron supplementation, a restrictive transfusion strategy, and the use of blood conserving measures.













