Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been recently published in each speciality (Cardiology, Cardiac Surgery, Cardiac Imaging, Perioperative Medicine).
Cardiology
Summarised by Sarah Catchpoole
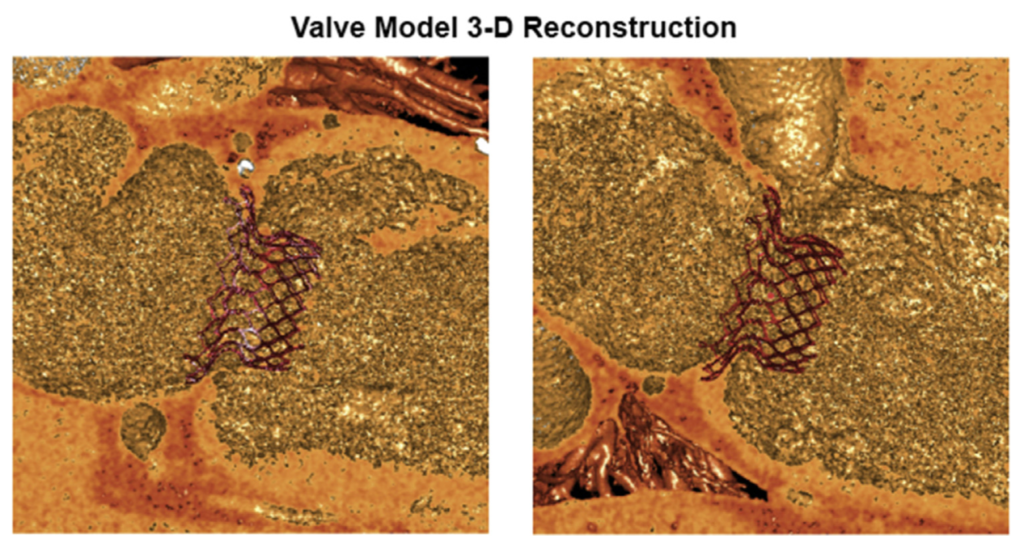
This paper details the successful first-in-human implantation of the HighLife transcatheter mitral valve system in two patients with severe functional mitral regurgitation. The device consists of two parts (Figure 1) – a subannular ring, which is implanted first via the transfemoral route, followed by deployment of the mitral bioprosthesis over the ring using an apical approach. Both patients who received the valve did not experience any intraoperative complications. Post-operative assessment demonstrated good haemodynamic prosthetic function, with only mild intraprosthetic regurgitation. One patient passed away 4 days post-operatively due to declining left ventricular function non-responsive to inotropes. The second patient retained excellent prosthetic function at five month follow up, with an improvement to NYHA Class II symptoms.
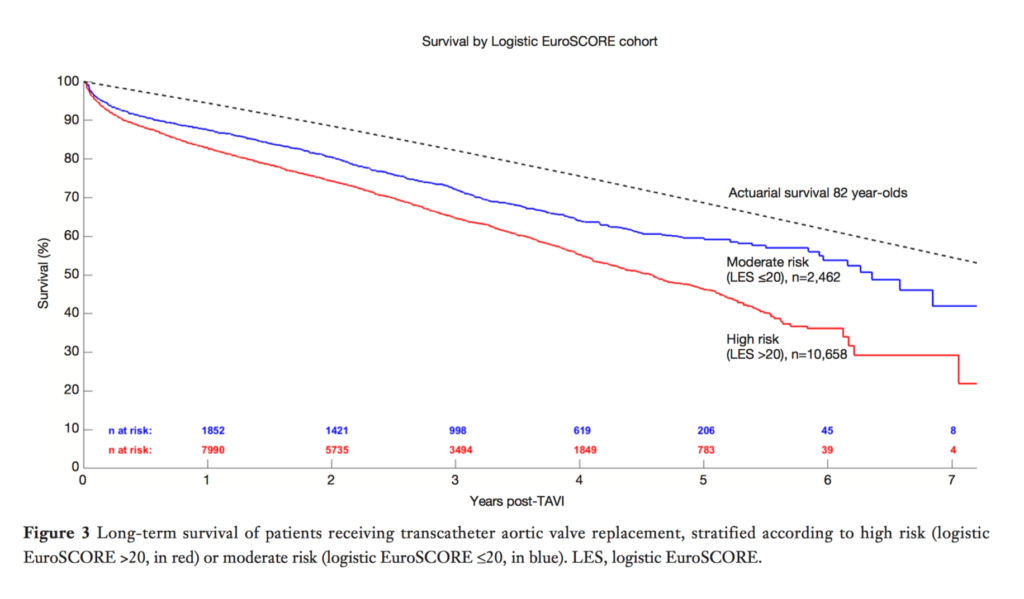
This new systematic review of long-term outcomes (>5 years) post transcather aortic valve implantation (TAVI) provides a much needed benchmark for the current status of this novel and increasingly popular therapy. Chakos et al. have combined data from 31 studies featuring a total of 13,857 patients. Common short term (30 day) complications of TAVI included cerebrovascular accidents (2.8%), permanent pacemaker implantation (13.4%), and acute kidney injury (14.4%), with an overall 30 day mortality of 8.4%. Long term survival was acceptable compared to the actuarial survival of 82 year olds – Figure 3 (below) shows Kaplan-Meier curves for overall survival, stratified by risk as determined by EuroSCORE. It should be noted that the review captures many initial experiences, and does not discriminate by device. The review finishes with four expert opinions to give further qualitative perspective to the current state and future possibilities of TAVI.
This is the largest prospective study to date to examine the benefit of cerebral embolic protection devices during transfemoral aortic valve replacement (TAVR). Of the 802 total patients enrolled over two years, the Claret Sentinel cerebral embolic protection device was successfully used in 280 of 305 patients (91.8%). A control group of 522 patients (65.1%) underwent the procedure without the device. After propensity matching, use of cerebral embolic protection was associated with lower rates of all-cause mortality or all-stroke within 7 days (2.1% vs. 6.8%, p=0.01; odds ratio: 0.30). In addition, the rate of disabling and non-disabling stroke was significantly reduced (1.4% vs 4.6%, p= 0.03, absolute risk reduction 3.2%, NNT 31). The authors conclude this data provides strong further evidence for the benefit of cerebral embolic protection during TAVR.
Cardiac Surgery
Summarised by Andrew Haymet
On-pump cardiac surgery provokes a predictable perioperative myocardial ischaemia–reperfusion injury which is associated with poor clinical outcomes. This prospective observational single-centre cohort and randomized study investigated the incidence of major adverse cardiac events in patients with severe aortic stenosis and preserved left ventricular ejection fraction undergoing either afternoon or morning aortic valve replacement surgery. In the cohort study of patients undergoing either morning surgery [n=298] or afternoon surgery [n=298]), the incidence of major adverse cardiac events 500 days postoperatively was lower in the afternoon surgery group than in the morning group (hazard ratio 0. 50; (95% CI 0·32–0·77; p=0·0021)). In the randomised study, 88 patients were randomly assigned to undergo surgery in the morning (n=44) or afternoon (n=44); perioperative myocardial injury assessed with the geometric mean of perioperative cardiac troponin T release was significantly lower in the afternoon group than in the morning group (estimated ratio of geometric means for afternoon to morning of 0·79 [95% CI 0·68–0·93; p=0·0045]). The authors concluded that perioperative myocardial injury is transcriptionally orchestrated by the circadian clock in patients undergoing aortic valve replacement, with Rev-Erbα antagonism appearing to be the appropriate pharmacological cardioprotective strategy. Afternoon operations may provide superior perioperative myocardial protection and improved patient outcomes compared with morning operations.
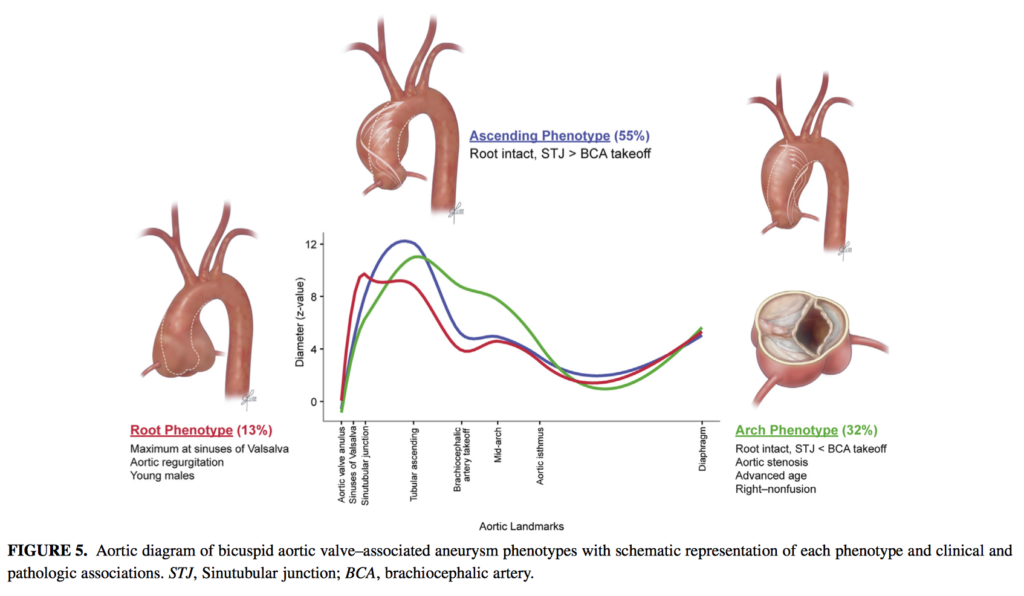
Bicuspid aortic valves (BAV) are associated with incompletely characterized aortopathy. This preoperative analysis of 656 patients with BAV undergoing ascending aortic surgery between January 2002 and January 2014 aimed to identify distinct patterns of aortopathy and characterize their association with valve morphology and patient characteristics. Three distinct aneurysm phenotypes were identified root (n=83; 13%), with predominant dilatation at sinuses of Valsalva; ascending (n=364; 55%), with supracoronary enlargement rarely extending past the brachiocephalic artery; and arch (n=209; 32%), with aortic arch dilatation. Patient age increased as the extent of aneurysm became more distal (root, 49 years; ascending, 53 years; arch, 57 years; P<.0001), and root phenotype was associated with greater male predominance compared with ascending and arch phenotypes (94%,76%, and 70%, respectively; P<.0001). The authors concluded that root, ascending aorta, and arch aneurysm are associated with distinct patient characteristics and thus should be taken into account in future studies on bicuspid aortopathy.
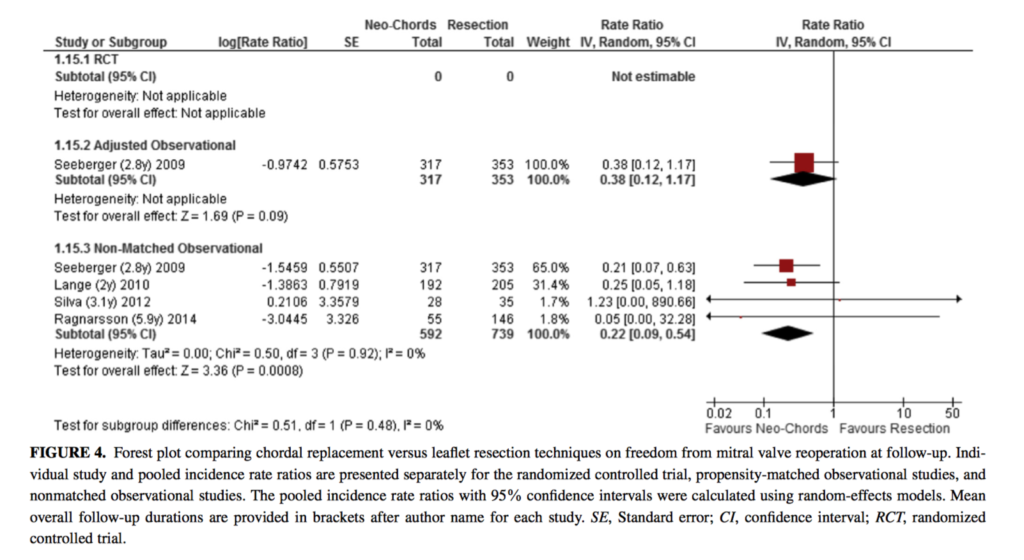
This systematic review and meta-analysis with a total of 1926 patients aimed to compare outcomes of chordal replacement versus leaflet resection techniques for repair of isolated posterior mitral leaflet prolapse. Based on limited data, postprocedural left ventricular ejection fraction may be greater in the neo-chord group, but this difference reached statistical significance only in the RCT (þ3.4%; P=0.03), and not in 2 observational studies that reported this outcome (þ2.7%; P=0.10). Whilst there was no difference in recurrent mitral regurgitation at follow up between the resection and neo-chord groups, patients in the neo-chord group had a lower rate of mitral valve reoperation at follow-up in the unadjusted follow up studies (incidence rate ratio, 0.22; P= 0.0008 [I2= 0%; 4 studies, 1331 patients]). The authors concluded that chordal replacement may be associated with greater freedom from reoperation and may lead to improved postoperative left ventricular function compared with leaflet resection. However, high quality RCTs of chordal replacement versus leaflet resection are required.
Cardiac Imaging
Summarised by Sarah Catchpoole
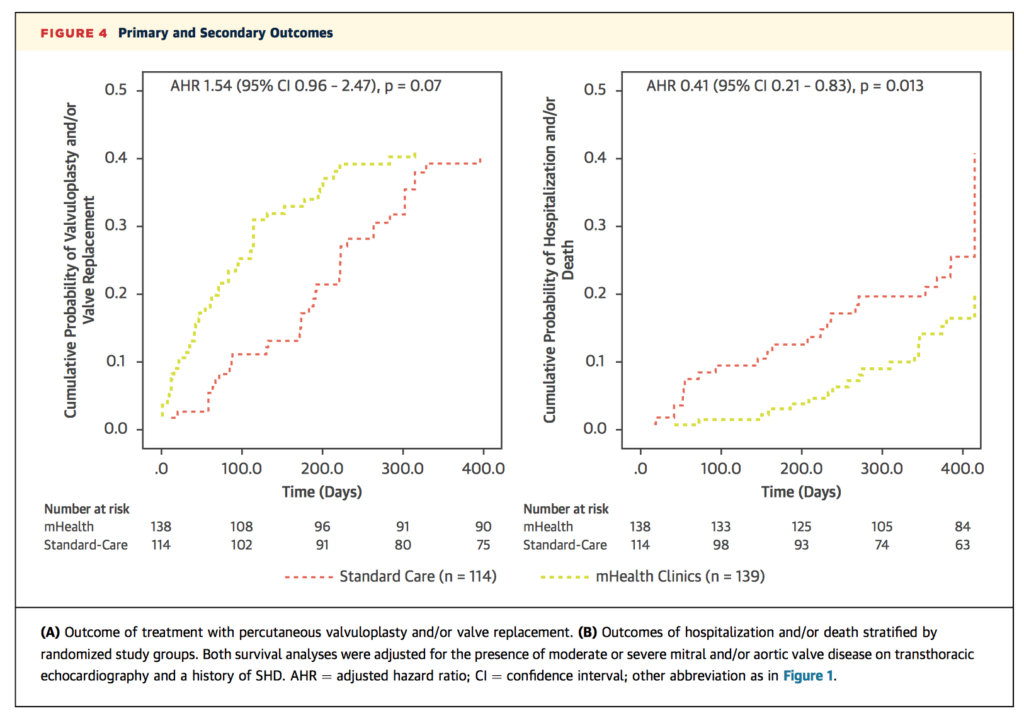
Mobile and low-cost medical devices have perhaps the most potential to change patient outcomes in resource-limited settings. At a tertiary care centre in Bangalore, India, 253 patients with known structural heart disease were randomised to either standard care or a mobile health (mHealth) assessment, including point-of-care echocardiography, ECG, pulse oximetry and BNP testing. At 12 month follow up, those who underwent the mHealth assessment had shorter referral times for valvuloplasty and/or valve replacement (83±79 days vs. 180±101 days, p<0.001), as well as a lower risk of hospitalisation or death (15% vs. 28%, p=0.013). The authors conclude point-of-care devices can improve time to treatment and outcomes in this setting.
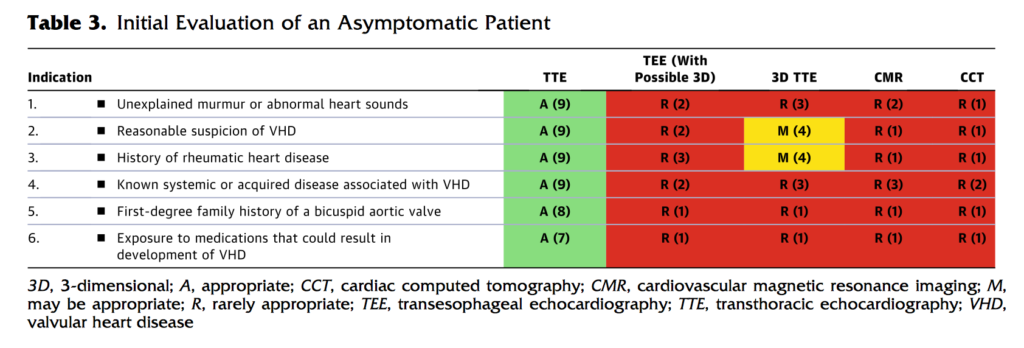
Appropriate use criteria (AUC) provide an invaluable reference for clinicians, patients and health policy makers in an era when the indications and variety of available imaging are expanding. These new guidelines, including a second companion document on structural heart disease, have adopted a new format presenting imaging choices for a given disease state, rather than evaluating by imaging modality. 92 common clinical scenarios were developed and imaging choices scored for appropriateness by a separate independent panel. Table 3 (below) gives an example of the format. The authors believe this approach better reflects day to day clinical decision making by offering the available diagnostic options for a given patient situation.
Quantifying radiation exposure and its consequences is increasingly important as minimally invasive fluoroscopic procedures become more commonplace. This is the first study to investigate potential individual differences in radiation susceptibility, using three biomarkers of radiation exposure (gamma-H2AX (ɣ-H2AX), DNA damage response (DDR) marker, and phosphorylated ataxia telangiectasia mutated (pATM)). 15 proceduralists had blood samples collected before, during and 24 hours after performing endovascular and open aortic repair. There was no change in ɣ-H2AX and pATM after open aortic repair, however both rose significantly after endovascular repair (p <0.0003), and returned to baseline by 24 hours (p<0.003). There was no significant increase in these markers if proceduralists wore additional lower leg lead pads, demonstrating the protective effect of lower leg shielding against scatter radiation (Figure, below).
Perioperative Medicine
Summarised by Andrew Haymet
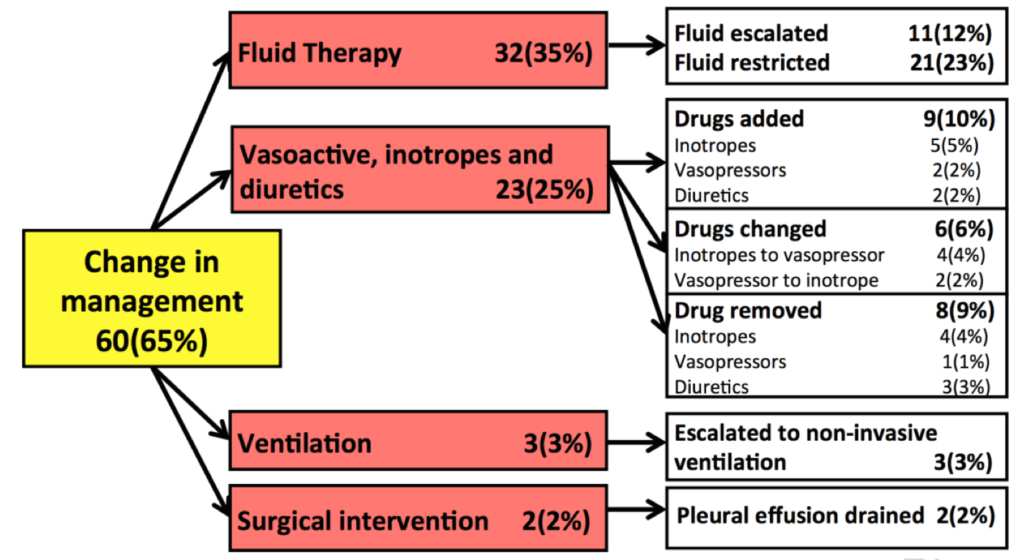
This prospective, observational study of evaluated the feasibility and impact of routine combined limited transthoracic echocardiography and lung ultrasound on the diagnosis and management of 93 critically ill patients admitted to ICU. The hemodynamic diagnosis was altered in 66% of participants, including new (14%) or altered (25%) abnormal states or exclusion of clinically diagnosed abnormal states (27%). Lung pathology diagnosis was changed in 58% of participants, including consolidation (13%), interstitial syndrome (4%) and pleural effusion (23%) and exclusion of clinically diagnosed consolidation (6%), interstitial syndrome (3%) and pleural effusion (9%). Management was altered in 65% of participants, including increased (12%) or decreased (23%) fluid therapy, initiation (10%), changing (6%) or cessation (9%) of inotropic, vasoactive or diuretic drugs, non-invasive ventilation (3%), and pleural drainage (2%). The authors concluded that routine combined limited TTE and lung ultrasound on admission frequently alters diagnosis and management.
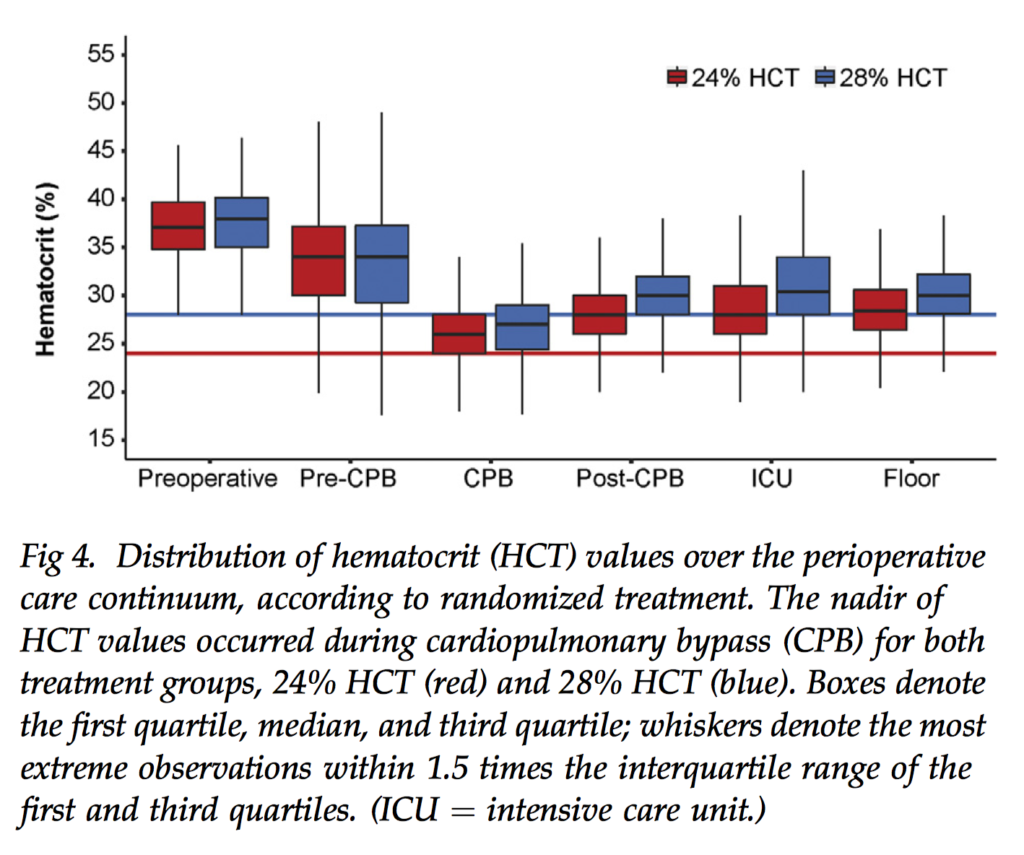
Class I evidence supporting a threshold for transfusion in the cardiac surgical setting is scarce. This study randomly allocated 722 adults undergoing coronary artery bypass graft surgery or valve procedures between March 2007 and August 2014 to a haematocrit transfusion trigger of 24% versus 28% to compare morbidity, mortality and resource usage. The study was stopped early after the a priori futility barrier was crossed. There was no detected treatment effect on the composite outcome (average relative effect odds ratio, low versus high, 0.86, 95% confidence interval: 0.29 to 2.54, p= 0.71). Negative exposures differed between treatment groups, with lower hematocrit in the 24% trigger group and more red blood cells used in the 28%group, but adverse outcomes did not differ. The authors concluded that because red blood cell usage was lower with a 24% trigger without adverse effects, aggressive blood conservation efforts are justified in cardiac surgery.