Welcome to the monthly SHDA Research Update. Our specialists have selected seminal papers that have been published recently in each speciality (cardiology, cardiac surgery, cardiac imaging, perioperative medicine).
Vemulapalli S, et al. Left atrial appendage to great cardiac vein fistula complicating watchman left atrial appendage closure. Eur Heart J. 2016 May 21
This case report outlines a left atrial appendage (LAA) closure complicated by a ‘bridging’ vessel connecting the anterior tip of the LAA to the great cardiac vein; the authors note that the effect this vessel would have on LAA closure was unclear. LAA flow velocity and anatomy is of particular importance and may increase the risk of thrombosis and stroke. The authors outline the options available, why lariat epicardial closure was not an option and why with endocardial device closure the bridging vein may act as a channel for thrombi to enter the right atrium. Ultimately, the LAA closure was achieved with a 30 mm WATCHMAN device. Images accompany the report including pre-reconstruction 3D volume rendered cardiac CT and 2D TEE and intraprocedural contrast fluoroscopy.
Kim JS, et al. The novel application of intraprocedural cardiac computed tomography for left atrial appendage occlusion. Eur Heart J. 2016 May 21;37(20):1626.
Another case report in the same journal issue outlines LAA occlusion with an Amplatzer cardiac plug (ACP). The authors report that using different imaging methods resulted in varied measurements for the size of the landing zone [18–21 mm using TEE; 19–21 mm using angiography; and 20–22 mm using multi-detector computed tomography system (MDCT)]. They based their final decision on the MDCT results and selected a 24 mm ACP.
The authors concluded that:
“The intraprocedural MDCT is able to provide more accurate information for the position of device and relationship between heart structure and device.”
This case report also includes a number of images and online supplementary videos which are available to European Heart Journal subscribers here.
Nishio M, et al. Chinese herbal drug natural indigo may cause pulmonary artery hypertension. Eur Heart J. 2016 Jul 1
This is an interesting case report outlining a possible association between natural indigo, a herb used in Chinese medicine, and the risk of pulmonary artery hypertension (PAH). A woman (aged 45) had been prescribed 2g/day of the herb to treat ulcerative colitis. She presented with symptoms including dyspnea and leg edema. Transthoracic echocardiography revealed features typical of severe pulmonary artery hypertension including flattening of the interventricular septum, dilated right ventricle and severe tricuspid regurgitation. A positive lymphocyte transformation test for natural indigo led the authors to suspect this herb was associated with PAH in this patient.
“Although no causative relationship between natural indigo and PAH has been established, clinicians should recognize a potential association between natural indigo and PAH,” the authors concluded.
Geske JB, et al. Spontaneous resolution of iatrogenic ascending aorta dissection: now you see it, now you do not. Eur Heart J. 2016 Jul 1
This case report describes an elderly woman undergoing mitral valve repair for ischaemic cardiomyopathy. Accompanying images show preoperative CT and TEE revealing an enlarged (47mm) ascending aorta. Following mitral valve repair, further TEE exhibited interval development of an ascending aortic dissection which is documented visually by a number of images in the case report. It was decided that the risks of repair outweighed benefits, however a CT angiogram <24 hours later showed that the dissection had repaired spontaneously.
“We postulate that antegrade dissection arose from the diseased axillary artery cannulated for cardiopulmonary bypass (CPB). Restoration of antegrade native flow into the ascending true lumen rapidly corrected the dissection,” the authors commented.
Kitkungvan D, et al. Detection of LA and LAA Thrombus by CMR in Patients Referred for Pulmonary Vein Isolation. JACC Cardiovasc Imaging. 2016 Jul
This prospective study of 261 patients investigated the use of comprehensive multicomponent cardiac magnetic resonance (CMR) as a tool to assess left atrial (LA) and left atrial appendage (LAA) thrombus. At present transesophageal echocardiography (TEE) is recommended as the gold standard for LA/LAA thrombus detection. For a patient undergoing preoperative assessment for pulmonary vein isolation (PVI) the battery of tests undertaken includes cardiac CT, cardiac CT scanning, TEE and CMR. Cardiac CT scanning has the disadvantage of exposing patients to increased radiation levels and also carries the risk of contrast-induced nephropathy. In this study, all patients underwent both multi-component CMR and TEE. CMR was performed using 1.5-T or 3-T whole-body scanners with a protocol that involved comprehensive evaluation using pulmonary venous anatomy (contrast-enhanced magnetic resonance angiography), cardiac function (cine-CMR) and myocardial viability (DE CMR).
Results of the TEE showed that 9 patients (3.5%) had LA/LAA thrombi. With long TI DE CMR a high level of diagnostic accuracy (99.2%) was observed with excellent sensitivity (100%) and specificity (99.2%) when compared to the gold standard of TEE.
The authors concluded:
“In patients referred for PVI, CMR could be a single complete diagnostic study for assessment of pulmonary venous anatomy as well as presence of LA/LAA thrombi, thus reducing the number of pre-operative tests before PVI.”
Berthelot-Richer M, et al. Discordant Grading of Aortic Stenosis Severity: Echocardiographic Predictors of Survival Benefit Associated With Aortic Valve Replacement. JACC Cardiovasc Imaging. 2016 Jul
This study of 1,710 patients investigated the survival benefit of aortic valve replacement (AVR) compared to medical management and also analysed findings by stratification according to aortic stenosis severity. Patients with an aortic valve area of from 0.8 cm2 – 1 cm2 were of particular interest as there has been debate regarding the severity of stenosis, due to a lack of correlation between the aortic valve area and mean gradient in this group. Some experts have even advocated for the redefinition of severe AS to an aortic valve area of ≤ 0.8 cm2.
Results showed that patients with an aortic valve area ≤1 cm2 had significant survival benefit from AVR compared to medical treatment (Figure A below).
The authors concluded that:
“Patients with discordant aortic grading, with an AVA ≤ 1.0 cm2 but MG or Vpeak in the non-severe range (ie, MG 25-40 mmHg or Vpeak 3-4 m/s) exhibited a significant improved survival associated with AVR. Hence, our results do not support the previously proposed suggestion of lowering the AVA threshold for AS severity to 0.8 cm2.”
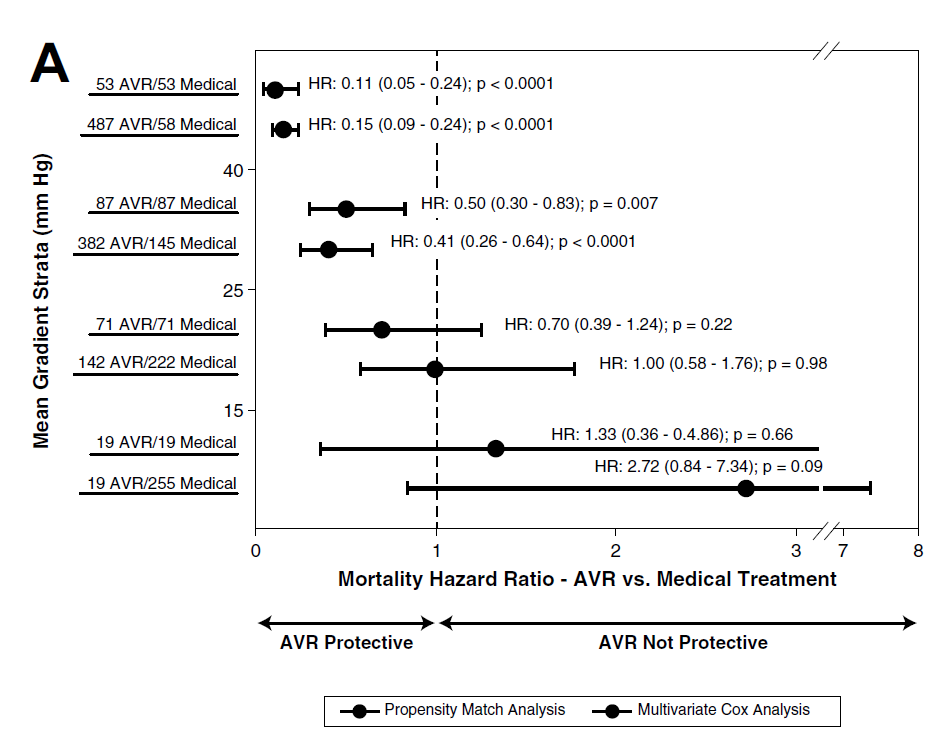
Figure A. Mortality hazard ratios for aortic valve replacement versus medical treatment according to strata of aortic valve area in the whole cohort.
Cardiac surgery Summarised by Andrew Haymet
Fibromuscular dysplasia (FMD) is a noninflammatory disease affecting arterial vasculature, with a predilection towards females. This study compared the frequency, location and outcomes of patients with FMD with aneurysm and/or dissection to those without. Of the 921 patients with FMD enrolled as at October 2014, 384 (41.7%) had an aneurysm and/or a dissection by the time of FMD diagnosis. Sites frequently implicated with aneurysms included extracranial carotid, renal and intracranial arteries, whilst those of dissection included extracranial carotid, vertebral, renal and coronary arteries. FMD patients with dissection were younger at presentation (48.4 vs. 53.5 years of age, respectively; p < 0.0001) and experienced more neurological symptoms and other end-organ ischemic events than those without dissection.
The authors recommended that, “every patient with FMD undergo one-time cross-sectional imaging from head to pelvis with computed tomographic angiography or magnetic resonance angiography”.
The surgical management of the aortic root in type A acute aortic dissection (TAAAD) remains disputed. This propensity matched study compared short and long term outcomes of root replacement (RR) versus conservative root management (CR). 296 patients were treated for TAAAD between 1999 and 2014, with 119 (40%) receiving RR and 177 (60%) receiving CR. The matched cohort hospital mortality rate was 26% and 21% respectively (P = 0.45). Patients in the RR group maintained greater freedom from proximal aortic re-intervention (at 7 years RR: 96 ± 3% vs CR: 80 ± 6%, log-rank P = 0.02) and this extended to the matched group (at 7 years RR: 98 ± 2 vs CR: 86 ± 6, log-rank P = 0.06). Whilst results were similar for early and late mortality for both groups, a more aggressive root intervention appeared to be protective against subsequent re-intervention.
Pulmonary hypertension is a common complication of mitral stenosis. This paper aimed to address the paucity of data pertaining to the management of concomitant mitral stenosis and pulmonary hypertension based on short and long term outcomes following mitral valve surgery.
317 patients who had undergone mitral valve replacement (78%) or repair (22%) between 1992 and 2014 were reviewed. Pulmonary hypertension (PH) was graded as mild, moderate and severe (pulmonary artery pressures (PAP) of 35 to 44, 45 to 59, or >60 mmHg). Primary outcomes were 30-day mortality and long term survival. Ten- and 12-year survival were significantly worse in the moderate–severe PH group (58% and 51%, respectively) compared with the normal PAP–mild PH group (83% and 79%, respectively) with a hazard ratio of 2.98 (95% confidence interval, 1.55-5.75; P = .001).
The authors concluded that “patients with mitral stenosis and mild PH (systolic PAP of 35-44mmHg) should be considered for mitral valve surgery”.
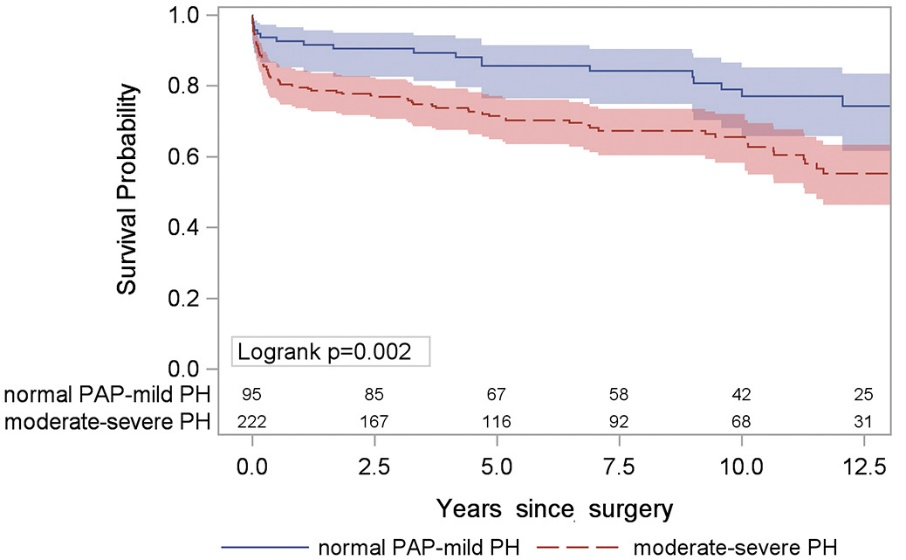
Figure above: Survival stratified by moderate–severe PH versus normal PAP–mild PH.
Perioperative Medicine Summarised by Andrew Haymet
The impact of surgical (SAVR) or transcatheter (TAVR) aortic valve replacement on longitudinal and circumferential right ventricular (RV) function was assessed using data from the NOTION randomized controlled trial. Echocardiographic data from 220 patients were used (SAVR, n= 106 vs. TAVR, n=114), with tricuspid annular systolic excursion (TAPSE) and fractional area change (RVFAC) used to assess RV function. In the SAVR group TAPSE was reduced by 35% three months postoperatively (p<0.001) and 30% after 12 months (P < 0.001). RVFAC was reduced by 12% after three months (P = 0.001), but had improved at 12 months (P = 0.34). In the TAVR group neither TAPSE nor RVFAC changed significantly after valve replacement (P > 0.05). Given the preoperative baseline similarity of the two groups, these findings are likely to be related to the type of intervention however, the clinical relevance remains to be clarified.
A single institution retrospective study was conducted to observe any association between left atrial appendage (LAA) velocity and the development of postoperative atrial fibrillation (POAF). In total, 562 adult patients undergoing cardiac surgery involving cardiopulmonary bypass were studied between January and December 2013. LAA velocity was quantified using transoesophageal echocardiogram, which ranged from 8 to 126cm/sec. 38.3% of patients developed POAF within 3 days postoperatively. In the adjusted logistic regression model, there was an 11% decrease in the odds of POAF for each 10-unit (cm/sec) increase in the LAA velocity (P = 0.044). Decreasing LAA velocity was found to be an independent predictor of risk for the development of POAF following cardiac surgery with cardiopulmonary bypass.
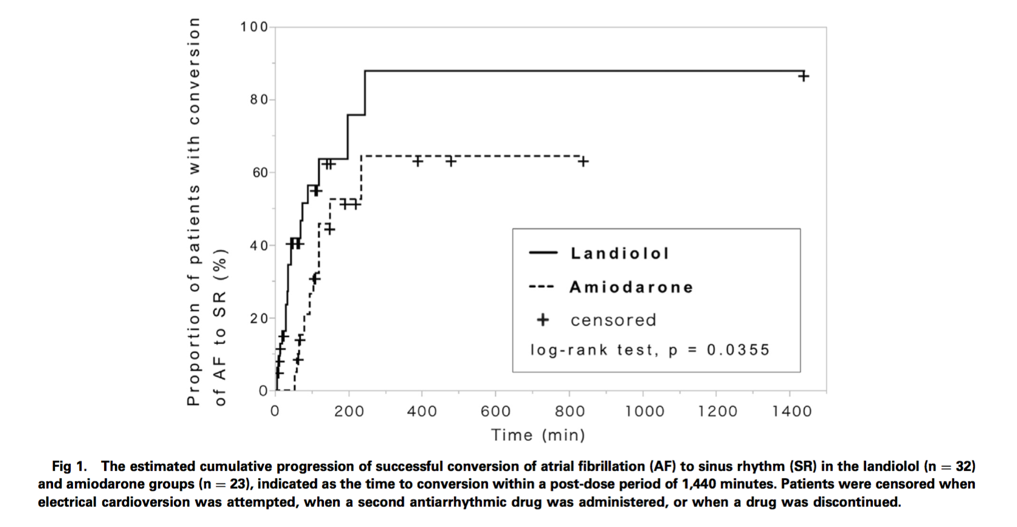
The efficacy and safety of landiolol, an ultra-short-acting beta-blocker, was compared with amiodarone in restoring sinus rhythm in patients in the intensive care unit (ICU) with postoperative atrial fibrillation (POAF). A retrospective analysis was performed on 276 patients who developed POAF after ICU admission between 2012 and 2015. The median time required for conversion to sinus rhythm was shorter in landiolol patients compared with amiodarone patients (75 vs. 150 min respectively, P = 0.0355), however after 24 hours treatment success rates were not significantly different (odds ratio 1.25, 95% confidence interval 0.17-9.09, P = 0.60). Landiolol rapidly restored sinus rhythm safely in ICU patients with POAF and could be considered as an alternative pharmacological choice over amiodarone in this population.