Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been recently published in each speciality (perioperative medicine, cardiac imaging, cardiology, cardiothoracic surgery).
Cardiology
Summarised by Sarah Catchpoole
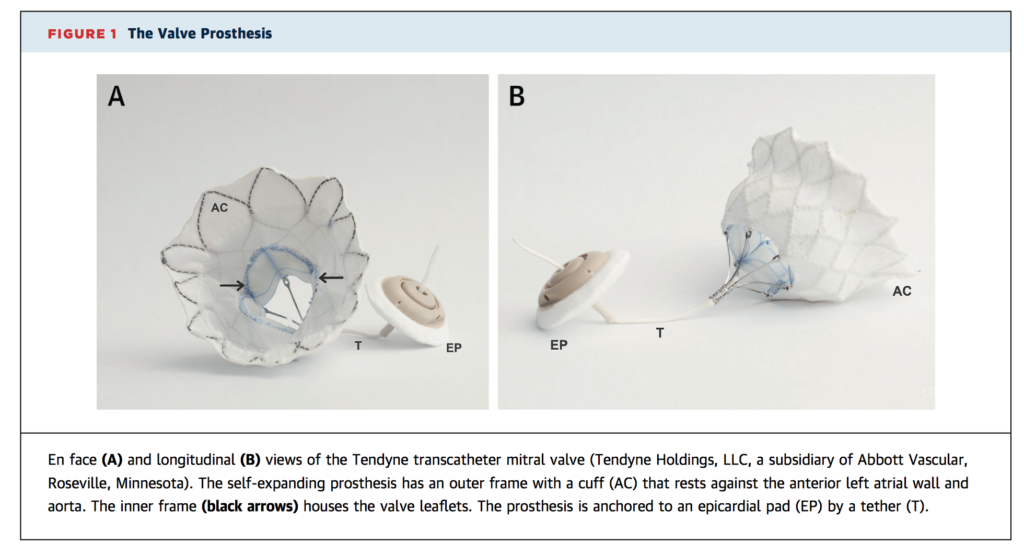
This prospective cohort study examines 30 high-risk patients with symptomatic mitral regurgitation (MR) who underwent transcatheter mitral valve replacement (TMVR). Device implantation was successful in 28 patients (93.3%). At 30 day follow up, 86.6% of patients remained free of cardiovascular mortality, stroke, and device malfunction. Transthoracic echocardiogram found no residual MR in 26 patients and mild (1+) central MR in 1 patient, and 75% reported mild or no symptoms (NYHA Class I or II). The authors conclude TMVR is safe, effective, and may provide an alternative in patients at high risk for surgery.
Stroke is a serious complication of transcatheter aortic valve replacement (TAVR) caused by embolization of particulate debris during the procedure. This multicentre randomised controlled trial is the largest to date evaluating use of a neuroprotection device during TAVR – the SentinelTM Transcatheter Cerebral Embolic Protection (TCEP) device, two filters placed in the brachiocephalic and the left common carotid arteries and removed after TAVR. A total of 363 patients were randomised to the safety cohort (n=123), or imaging cohort (n=119 control and n=121 device). Debris was found in the filters of 99% of patients, including valve tissue, arterial tissue, thrombus and foreign material. In the safety cohort, major adverse cardiac and cerebrovascular events at 30 days was not statistically different from controls (7.3% vs. 9.9%, respectively, p=0.33). In the imaging cohort, new lesion volume on MRI was no different between controls and device arms (178.0 mm3 vs. 102.8 mm3, respectively, p=0.33), nor was stroke incidence (9.1% vs. 5.6%, respectively, p=0.25) or neurocognitive function. The authors conclude that the SentinelTM TCEP device is safe and does capture embolic debris for 99% of patients. However, they note that the study was insufficiently powered to evaluate follow-up MRI findings or neurocognitive outcomes. In addition, it must be noted that the device protection excludes the territory of the left vertebral artery.
See this video for an interview with the study lead, Dr. Susheel Kodali.
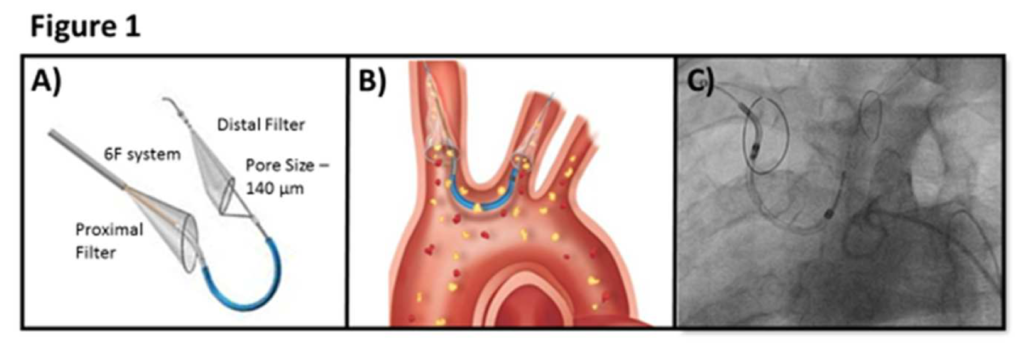
Figure 1: Panel A shows the Sentinel device. Panel B shows the proximal filter is placed in the innominate artery and the distal filter is placed in the left carotid artery. The pore size of the filters is 140 micron. Panel C shows fluoroscopic image of the device.
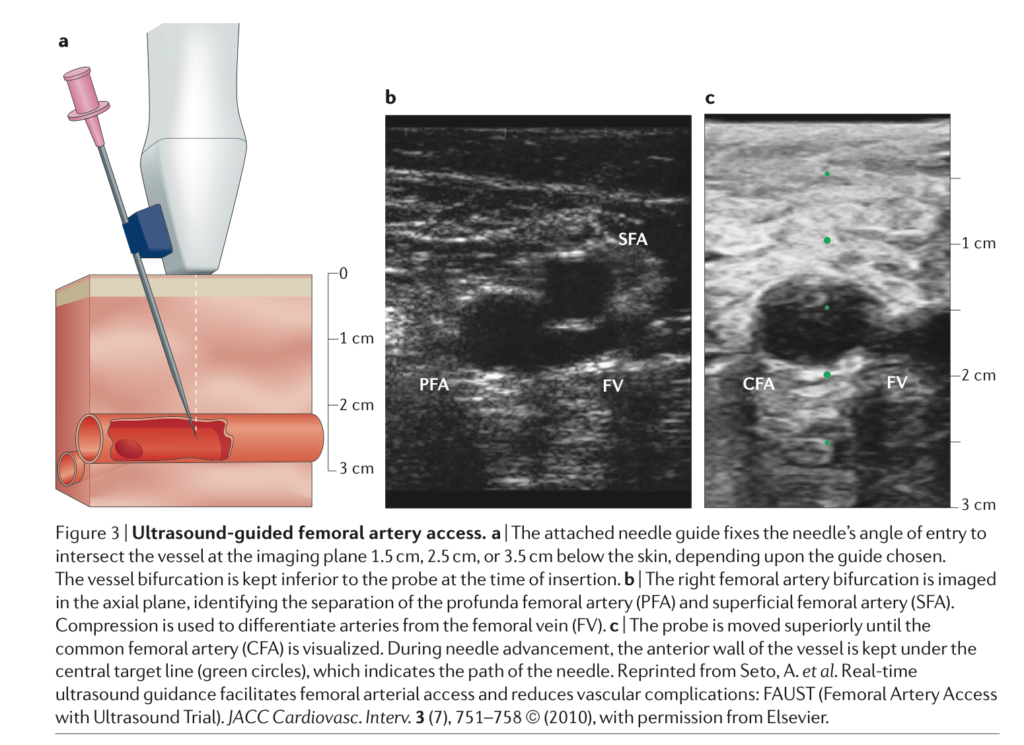
An overview of arterial access in cardiac catheterisation and intervention, including historical perspectives, techniques and devices, current practice and future directions. Of note, the authors compare the benefits of femoral vs. radial approaches. While they note trials are inconsistent, a radial approach is associated with greater patient comfort, faster time to ambulation, reduced access site bleeding and a reduction in mortality.
Cardiothoracic Surgery
Summarised by Andrew Haymet
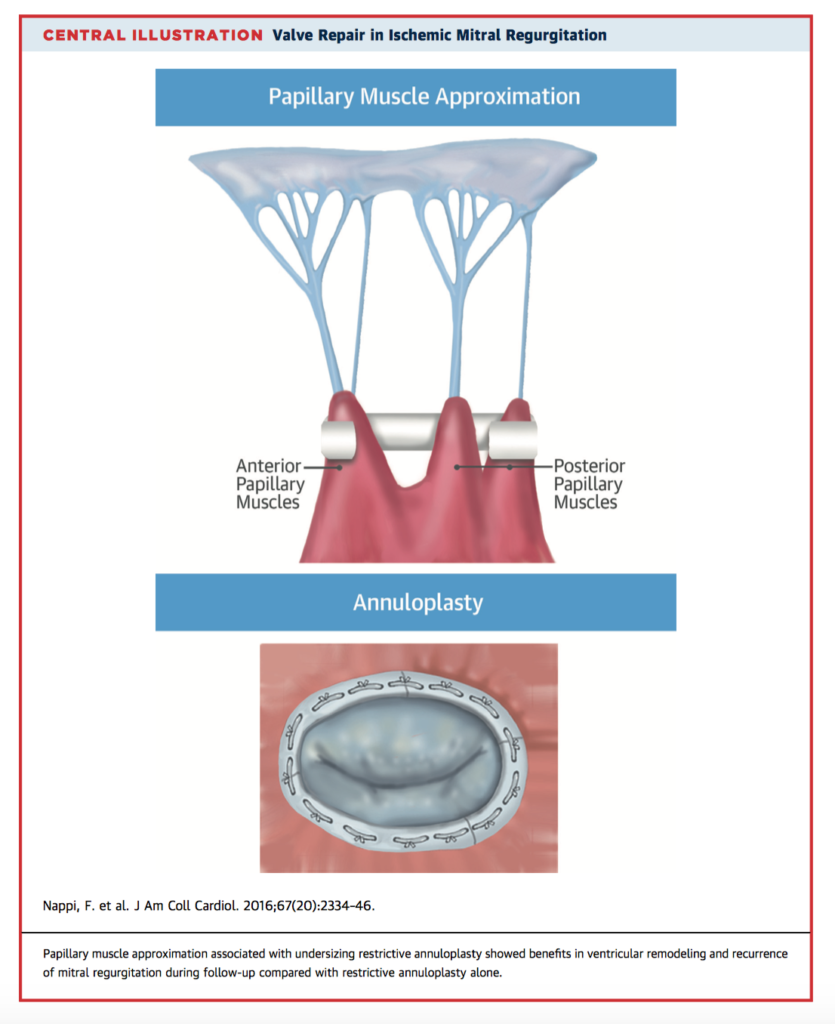
Current guidelines suggest that patients with severe ischaemic mitral regurgitation (MR) should undergo surgery. This study of 96 patients with ischaemic MR investigated the long term clinical outcomes of papillary muscle surgery. Patients were randomized to either undersizing restrictive mitral annuloplasty (RA) or papillary muscle approximation with undersizing restrictive mitral annuloplasty (PMA) associated with complete surgical myocardial revascularization. At five years, mean left ventricular end-diastolic diameter (LVEDD) was 56.5 +/-5.7mm with PMA versus 60.6 +/-4.6mm with RA (mean change from baseline -5.8+/-4.1mm and -0.2 +/-2.3mm, respectively; p<0.001). There was no significant difference in mortality at 5 years. Freedom from major adverse cardiac and cerebrovascular events (MACCE) favoured PMA in the final year of follow up. PMA was shown to effectively restore MV geometry and facilitated improved long term LV remodelling compared to RA alone, however these did not extend to improved mortality or QOL.
Aortic disease is complex and not fully explained by aortic dimensions alone. In this study of 45 subjects, individualised computational fluid dynamics were used to assess changes in velocity profiles, flow patterns, helicity, wall shear stress (WSS) and oscillatory shear index (OSI) in the thoracic aorta. Five groups were created: aortic regurgitation-tricuspid aortic valve (AR-TAV), aortic stenosis-tricuspid aortic valve (AS-TAV), aortic stenosis-bicuspid aortic valve right-left cusp fusion (BAV[RL]), and aortic stenosis-right-non cusp fusion (AS-BAV[RN]). Subjects underwent magnetic resonance angiography, and combined with haemodynamic data, patient-specific CFD was performed. BAV exhibited eccentric flow with high helicity, whilst the presence of AS led to greater WSS and lower OSI in the greater curvature of the ascending aorta. Individual patient CFD studies may allow more tailored, noninvasive approaches to diagnosis and management over and above those suggested by guidelines.
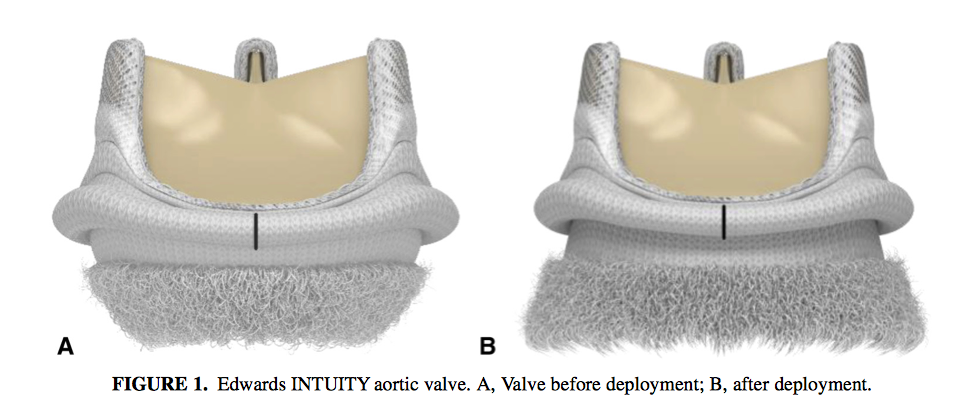
This prospective, nonrandomized, multicentre single arm trial investigated the performance of the INTUITY rapid deployment aortic valve replacement (RDAVR) system in patients with severe aortic stenosis. 839 patients underwent RDAVR between 2012 and 2015. At 30 days, all-cause mortality was 0.8%; valve explant 0.1%; thromboembolism, 3.5%; and major bleeding, 1.3%. At 1 year, mean effective orifice area was 1.7cm2; mean gradient, 10.3mmHg; and moderate and severe paravalvular leak, 1.2% and 0.4%, respectively. However, 11.9% of patients with isolated AVR required permanent pacemaker implantation. INTUITY RDAVR displayed robust haemodynamic performance and may lead to a reduction in aortic crossclamp and cardiopulmonary bypass time.
Cardiac Imaging
Summarised by Sarah Catchpoole
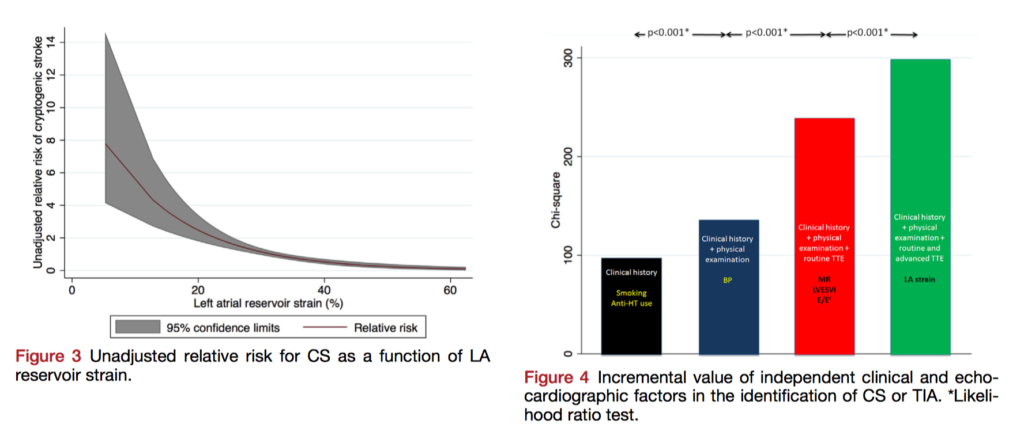
The precise aetiology of many strokes is never found despite investigations; research to better understand these “cryptogenic” strokes (CS) and improve primary prevention is needed. This retrospective case-control study investigates whether abnormalities of left atrial (LA) mechanical function, associated both with subclinical atherosclerosis and AF, could predict CS. 371 patients with CS were compared with 371 controls; LA strain on speckle-tracking echocardiography was significantly lower in patients with CS compared to controls (30±7.3% vs 34±6.7%, p< .001) and lower LA strain was independently associated with CS (OR, 1.07 per 1% reduction, p< .001). The authors conclude there is an independent and incremental (likelihood ratio P < .001) association of LA strain with CS, which may assist risk-stratification for prevention.
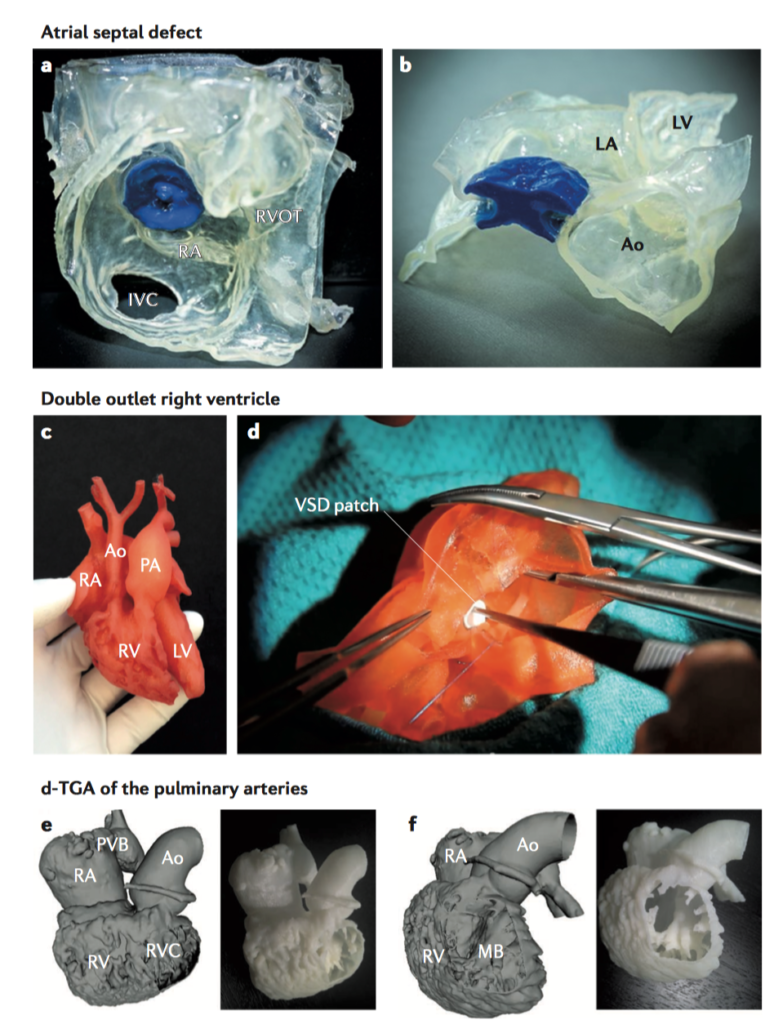
3D printing is widely heralded to transform medicine and cardiology; this summary from Nature Reviews Cardiology will provide an overview to clinicians wanting to familiarise themselves with its scope and potential. It begins with a summary of the 3D printing process from image acquisition to model creation, covers potential applications in cardiology including structural, valvular and vascular heart disease, finishing with current and future perspectives. Benefits to education and research, bioprinting vs. molecular printing, and the cost-effectiveness of 3D printing are also discussed.
A joint consensus document from the European Association of Cardiovascular Imaging and the American Society of Echocardiography reviewing the application and role of 3D echocardiography in congenital heart disease. This review could provide an excellent reference resource to clinicians regarding technical considerations, optimal image orientation, application of 3D echocardiography to different lesions. It finishes with recommendations for training and discussion of advances and future directions.
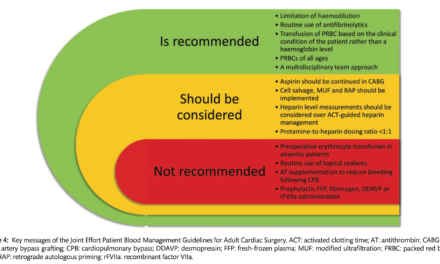
Perioperative Medicine
Summarised by Andrew Haymet
This retrospective review aimed to evaluate differences in the inclusion of anaesthetists in mobile extracorporeal membrane oxygenation (ECMO) teams between North American and European centres. 25 articles were published between 1986 and 2015 reporting the composition of personnel of mobile ECMO teams: 6 from North American centres and 19 from European centres. Of the North American studies, 0 of 6 (0%) reported the inclusion of an anaesthetist on mobile ECMO teams. In contrast, 10 of 19 (53%) of European studies reported the inclusion of an anaesthetist (Fisher exact p for difference = 0.05). Significant geographical discrepancies were found between European and North American mobile ECMO personnel, with European centres more likely to involve an anaesthetist.
This prospective, randomized study of 90 patients within a tertiary-care centre aimed to investigate the protective effect of L-carnitine against myocardial ischaemia-reperfusion injury and its mechanism. All patients received valve replacement under cardiopulmonary bypass. 3 groups were created, with two receiving L-carnitine added to the crystalloid cardioplegia solution (3g/L and 6g/L respectively), with the third group as control receiving no L-carnitine. Postoperatively, levels of serum aspartate aminotransferase, creatine kinase, creatine kinase-MB isozyme, and lactic acid dehydrogenase and the apoptotic index were all lower in the 2 experimental groups than those of the control. L-carnitine may reduce cardiopulmonary bypass-induced myocardial apoptosis through modulating the expressions of Bcl-2 and Bax, delivering a protective effect to the myocardium from ischaemic-reperfusion injury.
A retrospective analysis between 2007-2013, inclusive, of the American College of Surgeons National Surgical Quality Improvement Project Database was conducted. The aim was to determine the incidence, timing, risk factors for and outcomes following unplanned reintubation after adult cardiac surgery. A total of 18, 571 cardiac surgical patients over 18 years of age were included. Reintubation incidence was 4.0%, with risk factors including advanced age, preoperative partial or total dependence, dyspnoea at rest or on exertion, chronic kidney disease, chronic obstructive pulmonary disease, previous cardiac surgery, congestive heart failure, emergency or longer duration of surgery, and mitral or tricuspid surgery. Patients requiring reintubation had a mortality rate 7.5 times higher (21.9% vs 2.9%). They also experienced longer hospital admissions (22.2 vs 7.8 days) and were less likely to be discharged home within 30 days (35% vs 80%). In conclusion, patients reintubated after cardiac surgery had significantly higher mortality, complication rates and length of stay.