Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been recently published in each speciality (Cardiology, Cardiac Surgery, Cardiac Imaging, Perioperative Medicine).
Cardiology
Summarised by Sarah Catchpoole
Transcatheter aortic valve replacement (TAVR) has typically been reserved for surgically high-risk patients. This multi-centre randomised controlled trial examined whether TAVR can also benefit intermediate-risk patients with severe aortic stenosis. Of the 1746 patients randomised, 864 underwent TAVR and 796 underwent surgical replacement. Follow up at 24 months revealed no difference between groups for the primary end points death or severe stroke (12.6% and 14.0%, respectively , posterior probability of noninferiority, >0.999). TAVR was associated with greater rates of pacemaker implantation and residual aortic regurgitation. Surgical replacement was associated with greater rates of transfusion requirements, acute kidney injury, and atrial fibrillation. These results suggest TAVR is non-inferior to surgical replacement in intermediate risk patients. The New England Journal of Medicine QuickTake video summarises the findings (link).
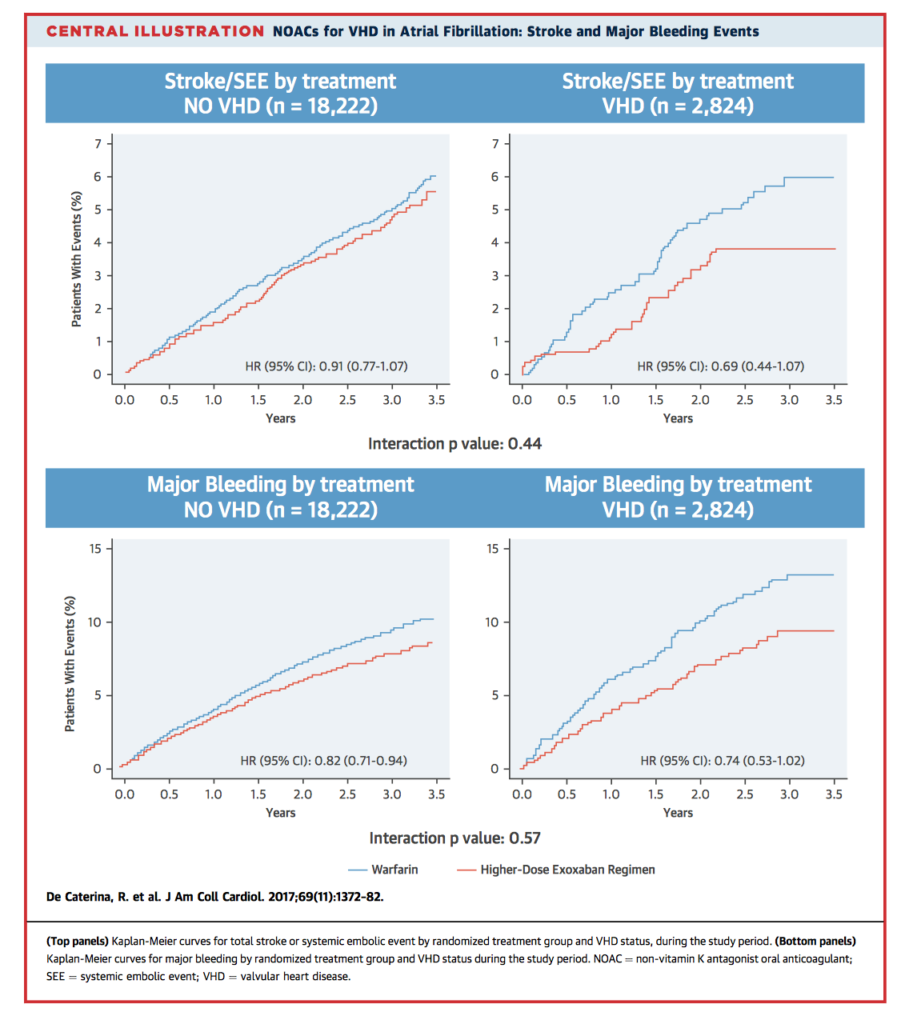
There is uncertainty regarding the best antithrombotic prophylaxis for patients with concurrent valvular heart disease (VHD) and atrial fibrillation (AF). This paper analyses data from patients with AF randomised to Edoxaban or Warfarin as part of the ENGAGE AF–TIMI 48 trial, according to the presence or absence of VHD. Exclusion criteria included patients with mechanical valves and moderate-severe mitral regurgitation. There were 18,222 non-VHD and 2,824 VHD patients; those with VHD had increased overall risk of death, major adverse events, and bleeding. However, there was no significant effect of VHD on the efficacy and safety of Edoxaban when compared to Warfarin. Edoxaban was associated with fewer bleeding complications overall. The authors conclude Edoxaban and other novel oral anticoagulants (NOACs) are safe to use in a subset of patients with VHD and AF.
Aortic stenosis (AS) is primarily associated with age-related valve leaflet calcification and shows a strong male preponderance. However, imaging studies have shown that for the same amount of valve calcification, women have more severe AS than men. To test the hypothesis that there could be sex-mediated differences in the pathogenesis of AS, the authors examined pre-operative imaging and post-operative valvular histology in 103 matched patients (64 men, 39 women) who underwent surgical aortic valve replacement for calcific AS. The findings demonstrated female sex is an independent risk factor for higher fibrosis (p=0.003), with women having lower median aortic valve calcification (p<0.0001), lower valve weight (p<0.0001), and stronger staining for collagen fibres (p=0.01) and dense connective tissue (p=0.02).
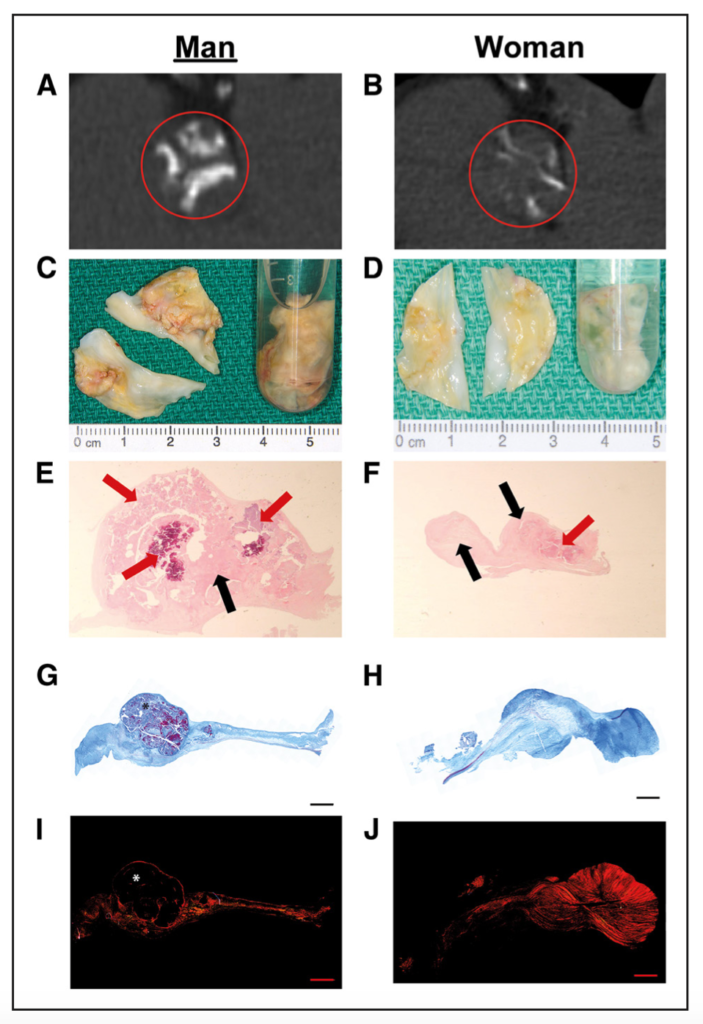
Figure 1. Radiological, macroscopic, and microscopic evaluation of stenotic aortic valve morphology and histology.
MRI remains contraindicated in patients with non-MRI-conditional pacemakers and implantable cardiovertable defibrillators (ICDs). In the prospective, multi-centre MagnaSafe Registry Study, 1000 pacemaker cases and 500 ICD cases (818 and 428 patients, respectively) underwent clinically indicated non-thoracic MRI at 1.5 tesla. There were no deaths, device or lead failures during MRI in patients who had their devices reprogrammed for imaging according to the study protocol. There were six cases of partial electrical reset and six cases of atrial fibrillation or flutter during or immediately after MRI. Pre and post MRI device settings changed for a percentage of patients at both immediate and 6 month follow up (see Table 4, below). This data could help clinicians with regard to balancing risk and benefit in patients with implanted devices who require non-thoracic MRI.
Cardiothoracic Surgery
Summarised by Andrew Haymet
Transcatheter aortic valve replacement therapy, having initially only been performed in inoperable or surgically high-risk groups, is now including patients of moderate risk. This contemporary analysis of aortic valve replacement (AVR) using a composite end point of 30-day death, stroke and dialysis for 2,979 patients undergoing isolated AVR or with coronary bypass grafting (CABG) between 2007 and 2015. The Society of Thoracic Surgeons predicted risk of mortality (PROM) was between 4 and 8% (mean 5.5%, interquartile range 4.5-6.3%). 30-day mortality was 3.9%. Morbidity included stroke in 2.3%, and renal failure, defined as Acute Kidney Injury Network stage 1 to 3, in 43.7%, although only 5.4% required dialysis. The authors concluded that moderate risk patients undergoing AVR experience favourable outcomes.
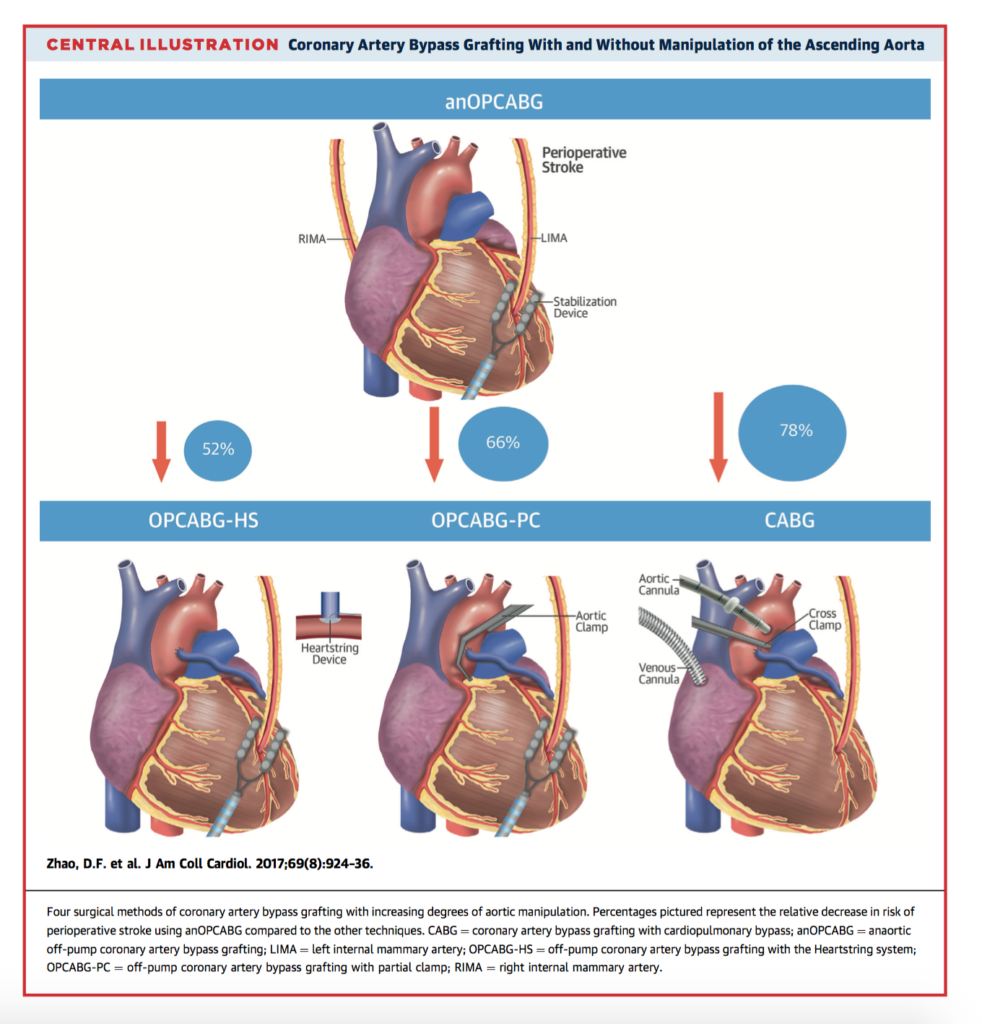
Anaortic “no touch” or anaortic off-pump CABG (anOPCABG) is a technique of surgical revascularization which eliminates all manipulation of the ascending aorta and reliance on cardiopulmonary bypass. One significant benefit may be a reduced risk of neurological injury due to dislodged atherosclerotic plaques. This network meta-analysis included a total of 37,720 patients receiving anOPCABG, OPCABG with a partial clamp (OPCABG-PC), anOPCABG with a Heartstring device (anOPCABG-HS), and CABG with cardiopulmonary bypass. In the primary outcome of stroke, anOPCABG was associated with a reduction of 78% in the 30 day risk of stroke compared with CABG (OR:0.22; 95% CI: 0.14 to 0.33), 66% compared with OPCABGPC (OR: 0.34; 95% CI: 0.22 to 0.52), and 52% compared with OPCABG-HS (OR: 0.48; 95% CI: 0.27 to 0.86). This study found that the risk of post-operative stroke, mortality, renal failure, atrial fibrillation, bleeding and length of ICU stay were lowest using an anOPCABG technique.
To increase the acceptance and durability of mechanical support, new devices with superior technology are needed. The novel HeartMate 3 is a new compact left ventricular assist device (LVAD) featuring a fully magnetically levitated pump, artificial pulse, large pump gaps, and a modular driveline. 27 patients were included in this retrospective study who received HM3 implantation. Within 1 year post implantation, 1 patient received a heart transplant, and 3 patients died. 30-day survival was 88.9% and 6-months 85.2%. No pump thromboses or strokes were observed within 6 months. Right heart failure was diagnosed in one patient (3.7%) after implantation. The HeartMate 3 has shown sound CE mark trial results with excellent midterm outcomes and low rates of other complications.
Cardiac Imaging
Summarised by Sarah Catchpoole
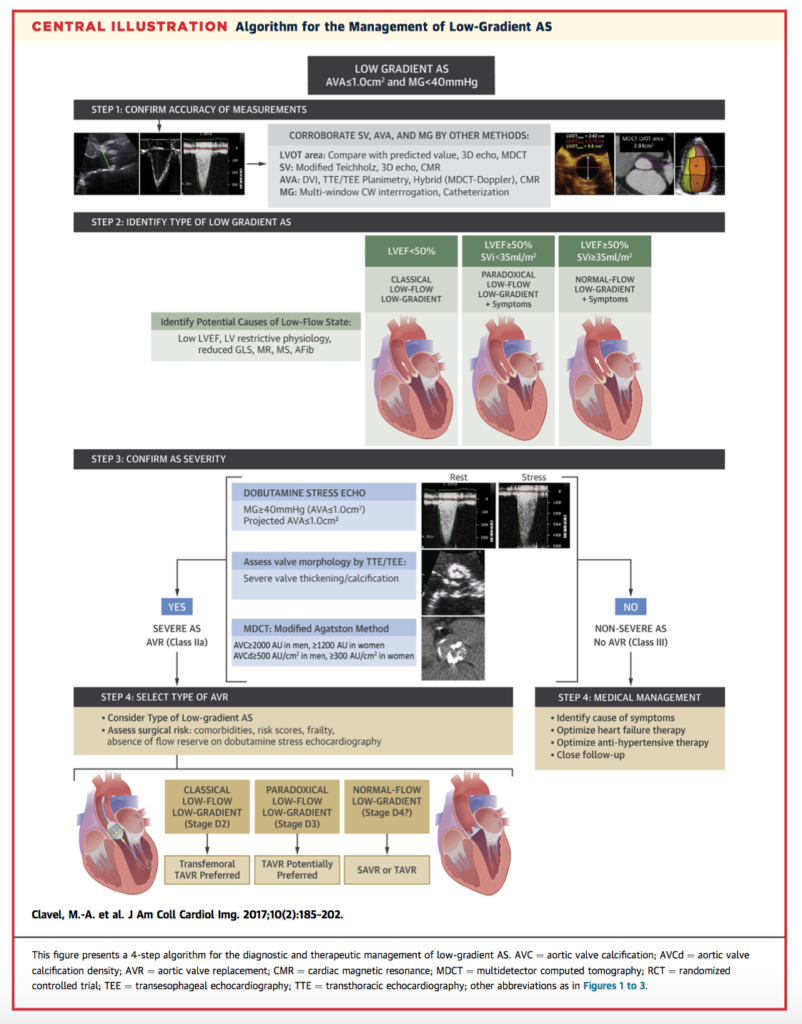
Assessment and management of low-gradient aortic stenosis (AS), where a small aortic valve area indicates severe disease but the transvalvular pressure gradient is moderate (< 40mmHg), is challenging. This discordance leads to uncertainty as to the “actual” severity of the disease. This review and summary provides guidance for clinicians on the benefits of multi-modality imaging for classification and grading of low-gradient AS, and accordingly which patients could benefit most from surgical or transcatheter aortic valve replacement. The central illustration, below, provides a summary of the recommendations.
Echocardiographic measurement of transvalvular pressure gradients are used to non-invasively estimate the severity of valvular pathologies such as aortic stenosis. However, they rely on the Bernoulli equation which incorporates just the single peak velocity value, although the fluid dynamics are doubtless more complex. In 32 patients with bicuspid aortic valve, the authors compared the traditional Bernoulli formula with the work-energy relative pressure (WERP) method, which uses cardiac MRI velocity fields to obtain a 3D picture of the blood flow. They found the Bernoulli method consistently overestimates the transvalvular gradient (mean 54%, range 5 -136%) compared to the WERP. The authors propose this more accurate measurement could enhance clinical decision making, and propose how the formula can also be adapted for echocardiographic parameters.
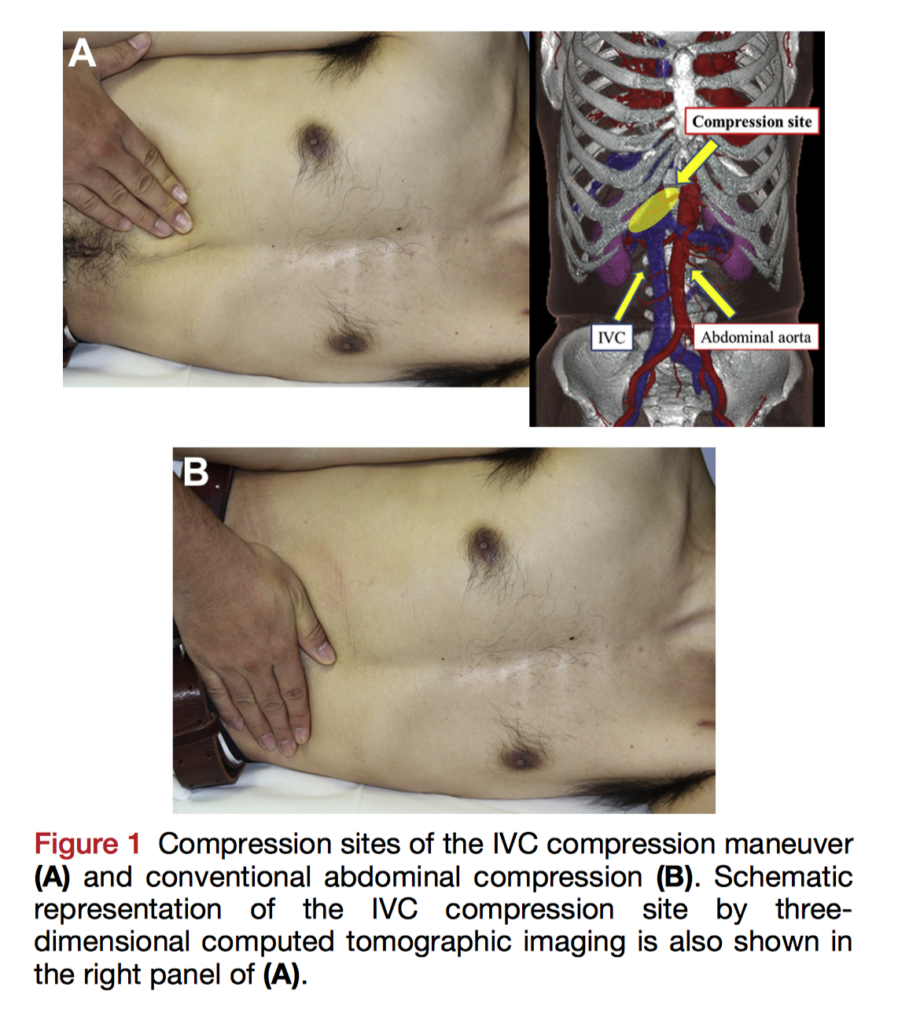
Detection of Patent Foramen Ovale (PFO) using transoesophageal echocardiography (TOE) can be enhanced by the Valsalva manoeuvre. However, the manoeuvre can be difficult for patients to perform. In this prospective study, the authors sought to evaluate inferior vena cava (IVC) compression as a patient-independent alternative to the Valsalva. 293 patients with paroxysmal atrial fibrillation undergoing TOE before ablation received agitated saline at rest, during Valsalva, and during IVC compression under deep sedation. The PFO detection rate was lowest at rest (5.2%), increased with Valsalva (12.8%), and highest with IVC compression (19.7%). There was no significant difference between the Valsalva and IVC compression for PFO detection, p = 0.31. The authors conclude IVC compression is not inferior to the Valsalva and is a good alternative for patients who cannot adequately perform the manoeuvre or require deep sedation.
Perioperative Medicine
Summarised by Andrew Haymet
Acute left ventricular dysfunction is a major complication of cardiac surgery and is associated with increased mortality. This multicentre, randomized, double-blinded, placebo-controlled trial investigated 30-day mortality in patients randomly receiving levosimendan infusions or placebo for up to 48 hours, or until discharge from the intensive care unit, in addition to standard care. The trial was stopped for futility after 506 patients were enrolled. There was no significant difference in 30-day mortality between the levosimendan group and the placebo group (32 patients [12.9%] and 33 patients [12.8%], respectively; absolute risk difference, 0.1 percentage points; 95% confidence interval [CI], −5.7 to 5.9; P =0.97). The authors concluded that in patients who required postoperative haemodynamic support after cardiac surgery, low dose levosimendan in addition to standard care did not result in lower 30-day mortality than placebo.
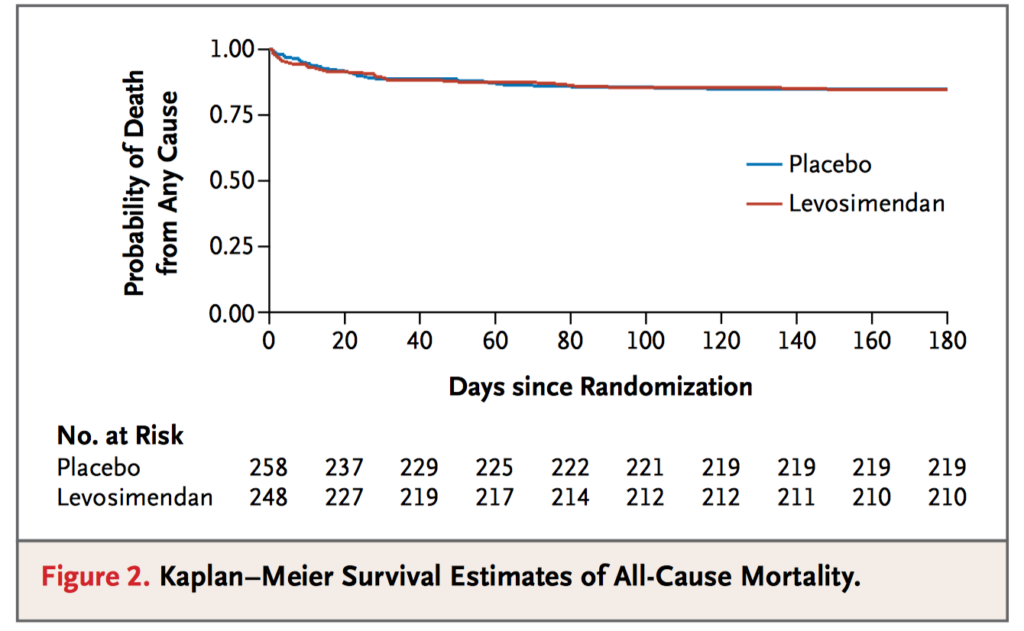
Levosimendan is an inotrope that has been shown in small studies to prevent or treat the low cardiac syndrome output after cardiac surgery. This multicentre, randomized, placebo-controlled phase 3 trial of 882 patients evaluated the efficacy and safety of levosimendan in patients with a left ventricular ejection fraction (LVEF) of 35% or less who were undergoing cardiac surgery with the use of cardiopulmonary bypass (CPB). The four-component primary end point consisted of death or renal replacement therapy through day 30, or perioperative myocardial infarction or use of mechanical support through day 5. This occurred in 105 of 428 patients (24.5%) assigned to receive levosimendan and in 103 of 421 (24.5%) assigned to receive placebo (adjusted odds ratio, 1.00; 99% confidence interval [CI], 0.66 to 1.54; P = 0.98). Compared to placebo, prophylactic levosimendan did not result in a lower rate of a composite end point of death, renal replacement therapy, perioperative myocardial infarction or use of mechanical circulatory support among patients with reduced LVEF undergoing cardiac surgery with CPB.













