Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been recently published in each speciality (Cardiology, Cardiac Surgery, Cardiac Imaging, Perioperative Medicine).
Summarised by Sarah Catchpoole
This large multinational genome-wide association study has identified new genetic loci and shed further light on the pathophysiology of aortic stenosis (AS). DNA was analysed from 2,457 Icelandic AS cases and 349,342 controls, as well as a further 4,850 AS cases and 451,731 controls from other national registries. The two new loci found were both also associated with bicuspid aortic valve, one with aortic root diameter, and one with coronary artery disease (CAD). In addition, a further 4 CAD variants were found to associate with AS, however causal analysis suggests this may be due to common pathways mediated by cholesterol metabolism. The authors conclude that the study further implicates structural cardiac abnormalities and shared physiology with atherosclerosis in the development of AS.
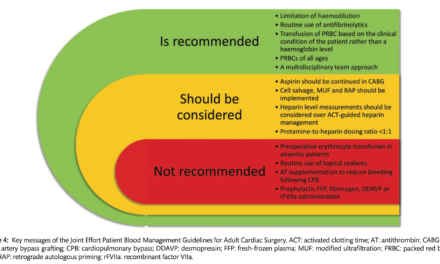
Geske JB, et al. Hypertrophic Cardiomyopathy: Clinical Update. JACC. Heart Failure 2018 April 5
Hypertrophic Cardiomyopathy (HOCM) is the most common genetic cardiomyopathy but is a heterogeneous condition requiring individualised, considered treatment. This new review provides an excellent summary and reference resource for clinicians working with HOCM patients. The pathophysiology, genetics and family screening, diagnosis, imaging and current therapeutic interventions are reviewed. Large sections are devoted to the risk of sudden cardiac death and management of symptoms. The author’s also propose a number of clinical algorithms to aid in risk stratification and decision making.
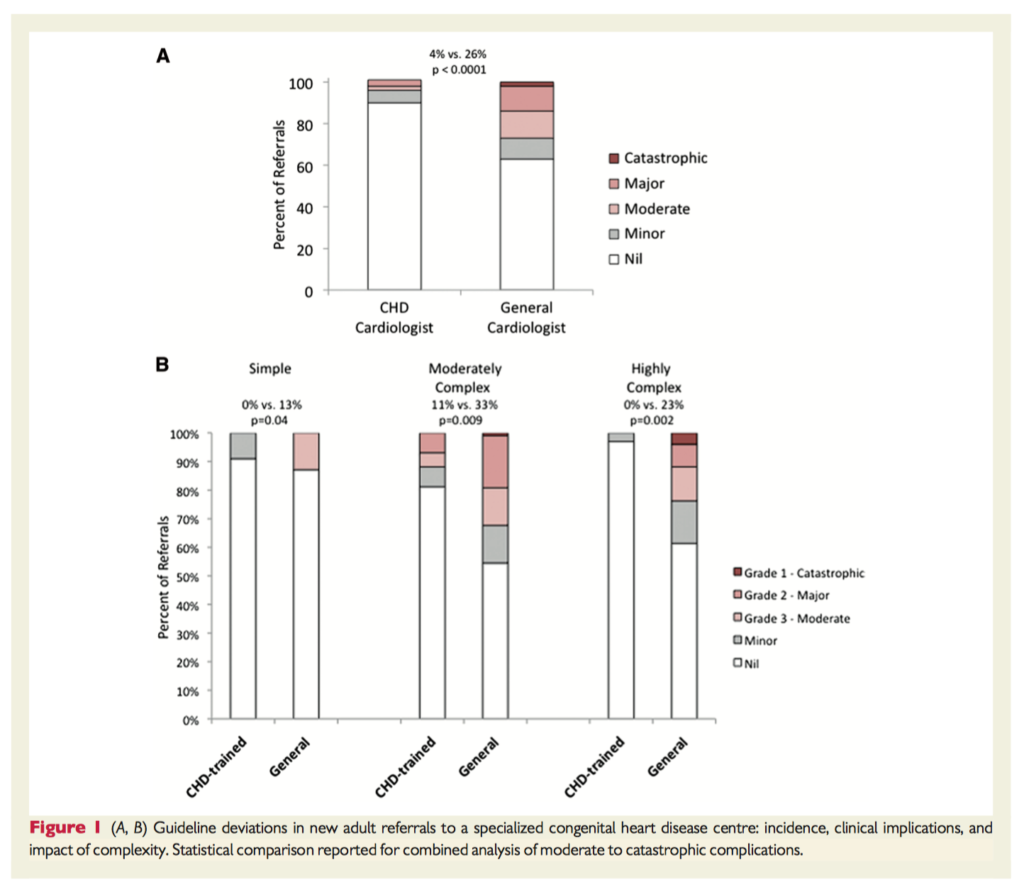
This is the first study to examine the benefit of tertiary specialist centre care in the rapidly expanding population of adults with congenital heart disease (ACHD). Over three years, consecutive new referrals to a tertiary ACHD centre were analysed. The majority were referred from general (43%) or ACHD specialist cardiologists (37%). Guideline deviations were more common in patients managed by general cardiologists (p<0.001, 37% non-adherence), and the rate of major complications was higher (n=18 for general cardiologists, vs. n=3 for ACHD specialists). Overall, all categories of ACHD patients (simple, moderate, complex) had an increased risk of adverse outcomes if not receiving specialist ACHD care.
Summarised by Andrew Haymet
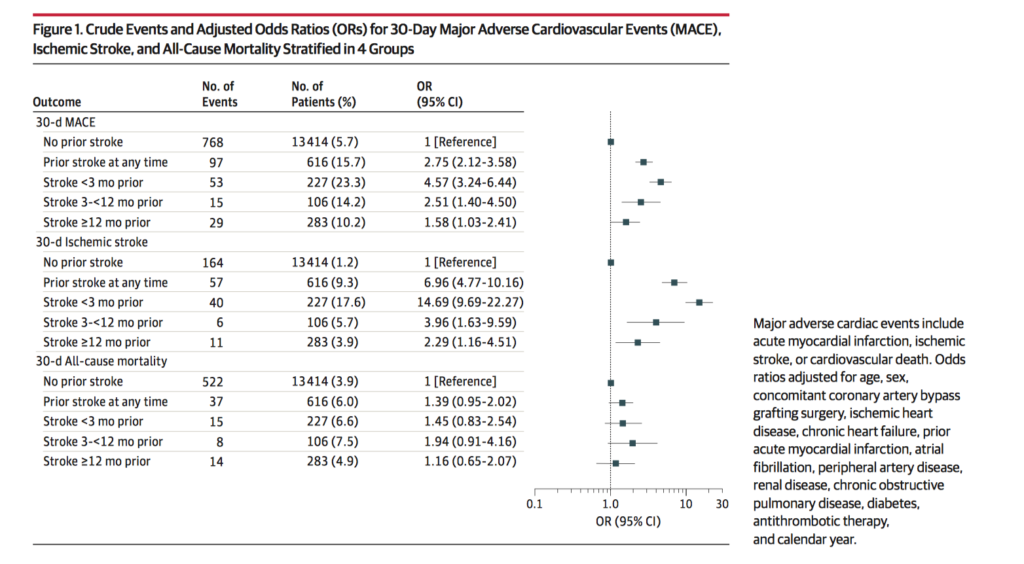
This cohort study included 14,030 patients from Danish administrative registries with AS who underwent SAVR between 1996 and 2014. 616 of these patients with prior stroke underwent surgery, and 13,414 without prior stroke underwent surgery. The absolute risk of ischaemic stroke was significantly increased in patients with stroke less than 3 months prior to surgery compared with patients with no prior stroke (18.4% vs 1.2%; OR 14.69; 95%CI 9.69-22.27). The authors concluded that previous stroke is a major risk factor of recurrent ischaemic stroke and MACE in patients undergoing SAVR, especially if the difference between previous stroke and surgery is less than 3 months.
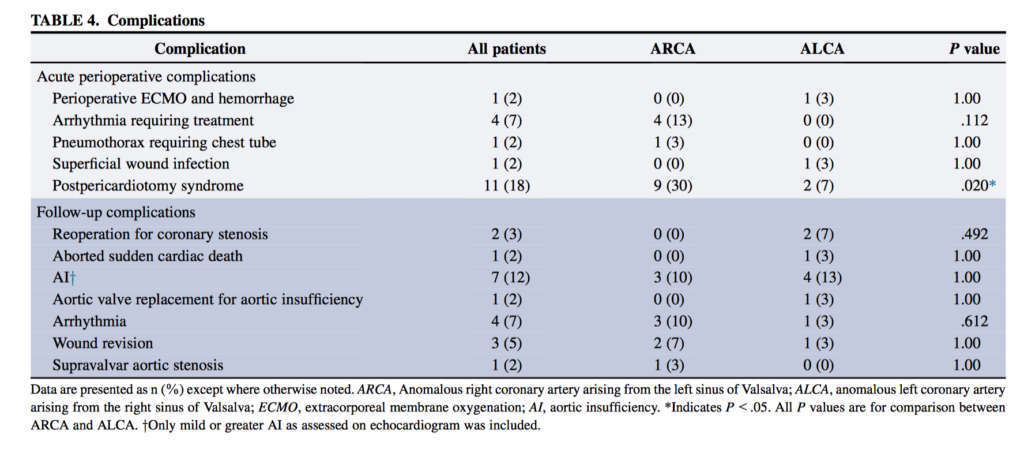
Anomalous aortic origin of a coronary artery (AAOCA) from the opposite sinus of Valsalva is a rare cardiac anomaly associated with sudden cardiac death (SCD). 60 patients underwent AAOCA repair between 2001 and 2016. Half of the patients had an anomalous left coronary artery arising from the right sinus of Valsalva and half had an anomalous right. Median age at surgery was 15.4 years. Follow-up data were available for 54 patients (90%) over a median of 1.6 years. Of 53 patients with symptoms at presentation, 34 (64%) had complete resolution postoperatively. Postoperative mild or greater aortic insufficiency was present in 8 patients (17%) and moderate supravalvar aortic stenosis in 1 (2%). The authors concluded that repair of AAOCA can be performed safely. Restenosis and sudden cardiac death can occur, and long term surveillance is critical.
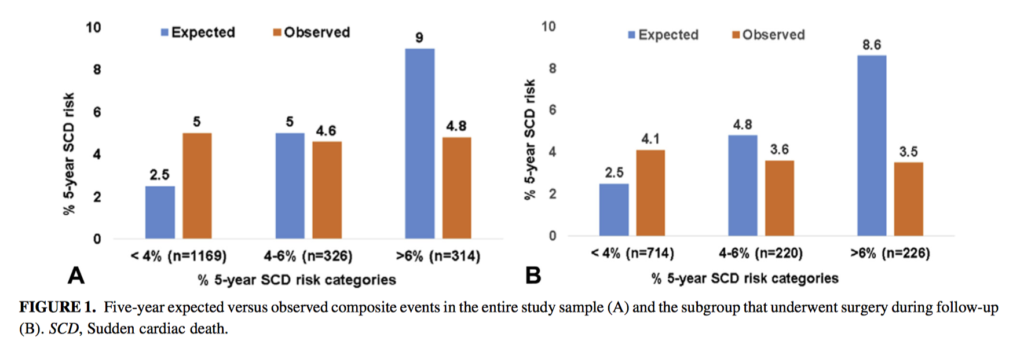
This study of 1,809 patients with obstructive HCM aimed to determine the prognostic utility of the European Society of Cardiology SCD risk score, and to evaluate whether additional factors can modulate SCD risk. Surgical myectomy was performed in 1,160 patients (64%). At a mean of 8.8± 4 years, 169 patients had a composite event (154 SCDs). On multivariable competing-risk analysis, myectomy (subdistribution HR 0.69; 95% CI 0.47-0.83) was associated with lower risk of longer-term composite events, whereas ESC SCD risk score was not (sHR 1.31; 95% CI 0.75-2.25). The authors concluded that in patients with HCM, the observed primary events were similar across the 3 ESC SCD risk categories, with myectomy mitigating SCD risk. In patients with obstructive HCM, SCD risk may need to be refined for patients following myectomy.
Summarised by Sarah Catchpoole
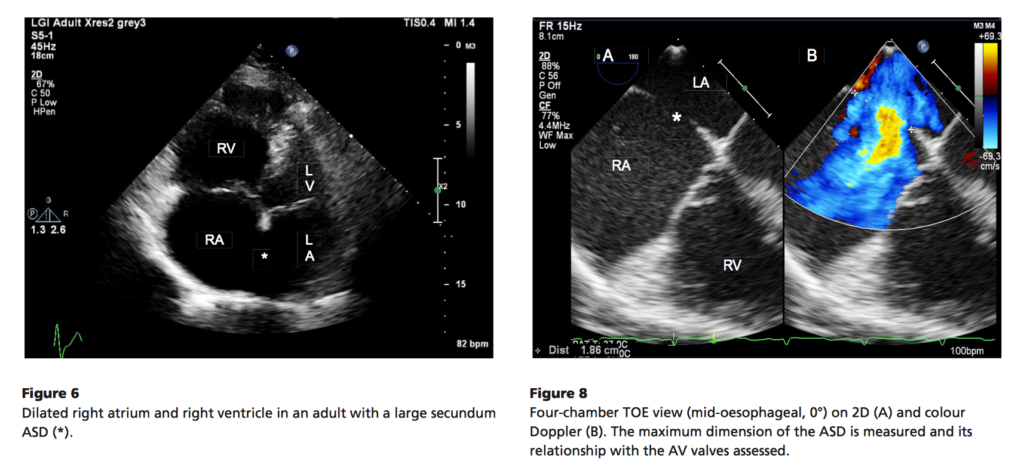
This open-access review of right to left shunts provides a visually rich teaching, reference, and revision resource for students and clinicians. The procedure for echocardiographic assessment and features of shunt pathologies including patent ductus arteriosus, atrial septal defects, ventricular septal defects, and atrioventricular septal defects are reviewed. A number of free online videos supplement the article well, and all images are available for free download as power point slides on the journal website. Part of a new educational series, another review on assessment of congenital left-sided heart obstruction has also recently been published.
Friedberg MK. Imaging Right-Left Ventricular Interactions. JACC: Cardiovascular Imaging. 2018 May.
While the heart is often conceptualised in discrete anatomical or functional units, it nevertheless functions as one dynamic structure. This review by Friedberg examines the current literature on the assessment and clinical implications of ventricular-ventricular interactions. He begins by reviewing physiological studies demonstrating left ventricular (LV) and right ventricular interactions (RV); for example, the role of the septum, and the impact of LV contraction on RV pressures. The bulk of the review is devoted to echocardiographic assessment of such interactions. Table 1 (below) summarises useful echocardiographic parameters, and their known prognostic implications.

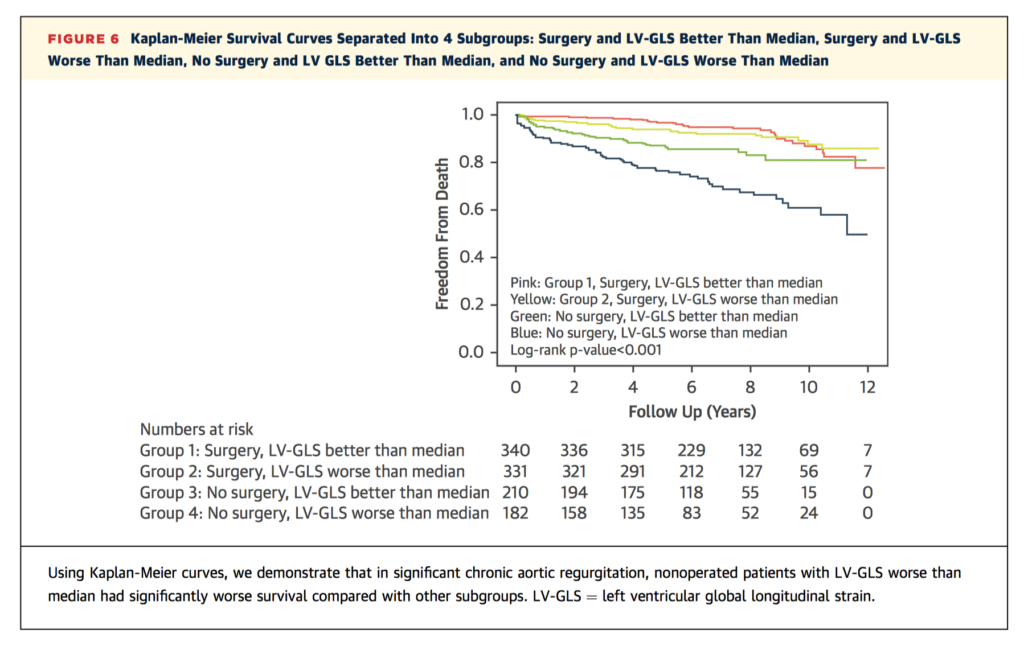
Optimal timing for AVR in severe aortic regurgitation (AR) with preserved left ventricular ejection fraction (LVEF) remains a difficult decision. This study sought to examine whether left ventricular global longitudinal strain (LV-GLS) can provide additional prognostic utility to aid risk stratification and clinical decision making. In an observational cohort, 1,063 asymptomatic patients were followed up for a median of 6.8 ± 3.0 years. Overall mortality was 14%, which was predicted by LV-GLS (HR 1.11), Society of Thoracic Surgeon’s Score (HR 1.51), and right ventricular systolic pressure (HR1.33), and improved with aortic valve surgery (HR 0.35). Sequential addition of LV-GLS and aortic valve surgery improved the C-statistic for longer term mortality from 0.61 to 0.77 (95% CI 0.63-0.90, p<0.001).
Summarised by Andrew Haymet
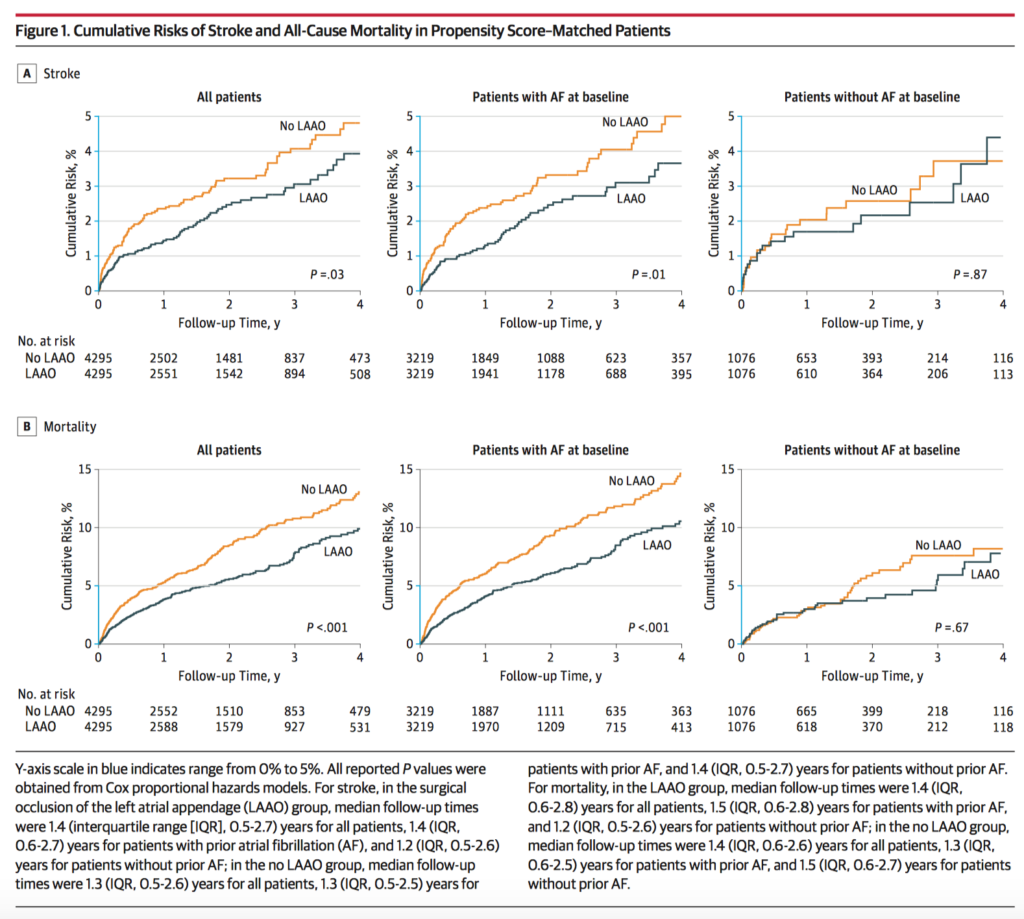
Surgical occlusion of the left atrial appendage (LAAO) can be performed concurrently during cardiac surgery. However there are limited data on the association of LAAO with long-term risk of stroke, and some evidence suggests that this procedure may be associated with subsequent development of atrial fibrillation (AF). 75,782 patients underwent coronary artery bypass graft (CABG) or valve surgery between 2009 and 2017. In the 8590 propensity score–matched patients, LAAO was associated with a reduced risk of stroke (1.14 vs 1.59 events per 100 person-years; HR 0.73l 95%CI 0.56-0.96) and mortality (3.01 vs 4.30 events per 100 person-years; HR 0.71; 95%CI 0.60-0.84). The authors concluded that concurrent surgical LAAO compared to none, was associated with reduced risk of subsequent stroke and mortality.
Extracorporeal Membrane Oxygenation (ECMO) is used in cases of severe respiratory and/or circulatory failure over periods of several days to several weeks. Its components require closely monitored anticoagulation empirically supported by activated clotting time (ACT). This study of 109 patients receiving venovenous or venoarterial ECMO aimed to compared the measurement of heparin activity with ACT and the direct measurement of heparin activity (anti-Xa). Spearman analysis found no correlation between anti-Xa and ACT (r < 0.4) from day 1 and worsened over time. Kappa analysis showed no agreement between the respective target ranges of ACT and anti-Xa. The authors concluded that concomitant measurement of ACT and anti-Xa activity is irrelevant in ECMO patients. Anti-Xa activity appears to be a more suitable assay for anticoagulation monitoring since ACT is poorly correlated with heparin dosage.
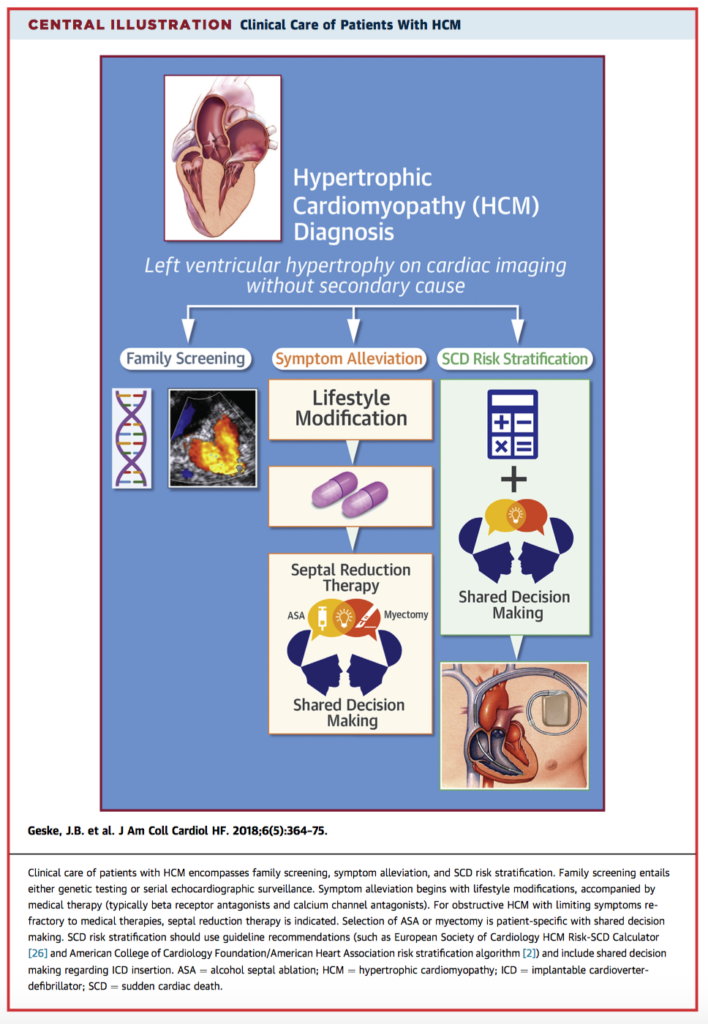
This retrospective study of 4,869 consecutive patients aimed to derive and validate a clinical risk index that can predict readmission to the intensive care unit (ICU) following cardiac surgery. A total of 156 patients (3.2%) were readmitted to the ICU during their index surgical admission. Nine independent variables were associated with readmission, including urgency of surgery, diabetes, chronic kidney disease stage 3 to 5, aortic valve surgery, European System for Cardiac Operative Risk Evaluation, postoperative anaemia, hypertension, preoperative neurological disease, and the Intensive Care National Audit and Research Centre score. Mortality (18% v 3.2%, p<0.0001) was shown to be significantly higher in readmitted patients. The median duration of ICU stay (7 [4-17] v 1 [1-2] days, p<0.0001) and hospital stay (20 [12-33] v 7 [5-10] days, p<0.0001) were significantly longer in patients who were readmitted to ICU as well. The authors derived and validated a risk index incorporating 9 routinely collected variables to predict readmission following cardiac surgery.