Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been recently published in each speciality (perioperative medicine, cardiac imaging, cardiology, cardiothoracic surgery).
Cardiology
Summarised by Sarah Catchpoole
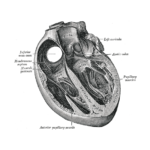
Transcatheter interventions for tricuspid valve disease of growing interest. This paper describes the 30 day results of the SCOUT trial, the first early feasibility study of a novel device (TriAlign®) for tricuspid regurgitation (TR). Device implantation was achieved without complications in all 15 enrolled patients across four centres, with an 80% device success rate at 30 days (3 patients experienced single-pledgelet annular detachment). The remaining patients were found to have significantly improved quality of life scores and echocardiographic parameters of TR. While further trials are needed, these early results demonstrate the procedure is feasible, safe, and improves clinical outcomes.
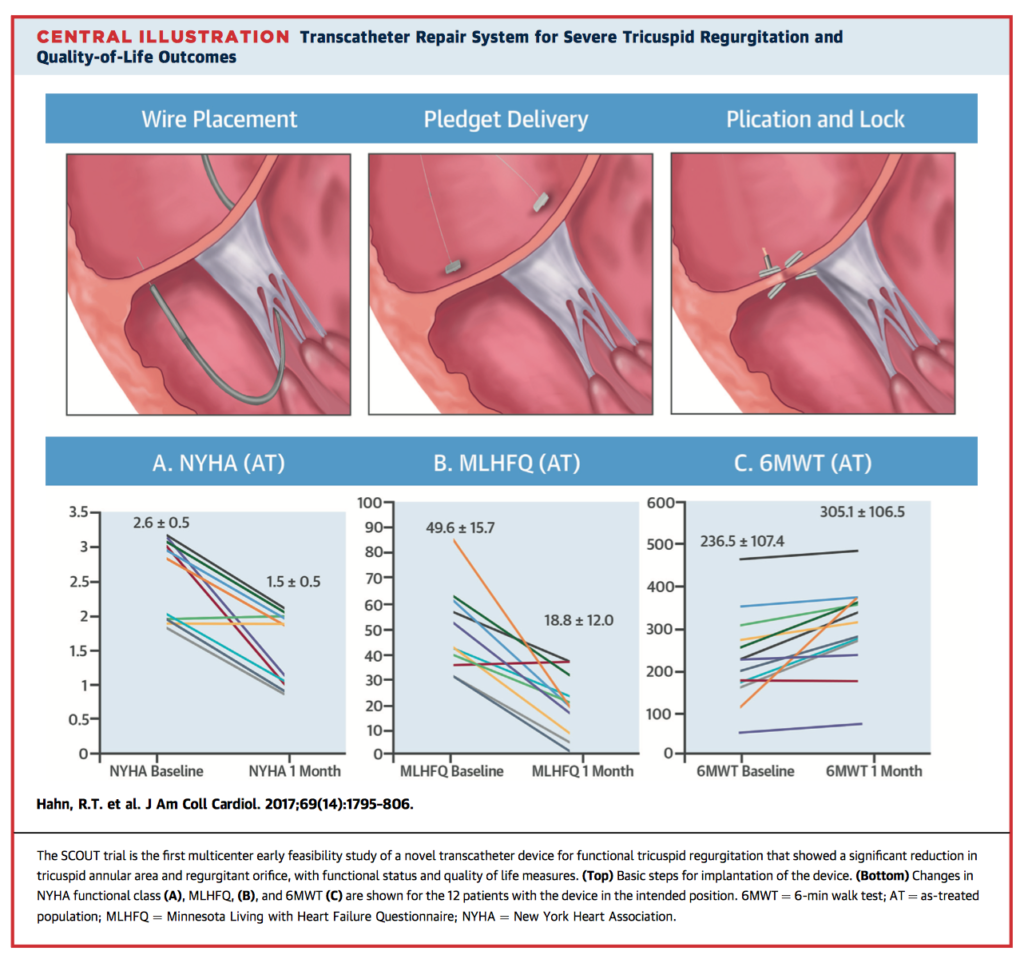
Anomalous coronary arteries arising at or above the inappropriate sinus of Valsalva have been associated with an increased risk of sudden death on autopsy and are increasingly recognised on imaging. This comprehensive review represents a significant contribution to an area where there is much uncertainty, summarising their classification, prevalence, risk stratification, and management. In addition, the authors have conducted two meta-analyses of the literature. To determine prevalence, data from 77 studies with more than one million patients revealed that anomalous right coronary artery is more common than anomalous left coronary artery (0.23% vs. 0.03% weighted prevalence, respectively). To examine outcomes, 20 eligible studies have been presented in narrative review.
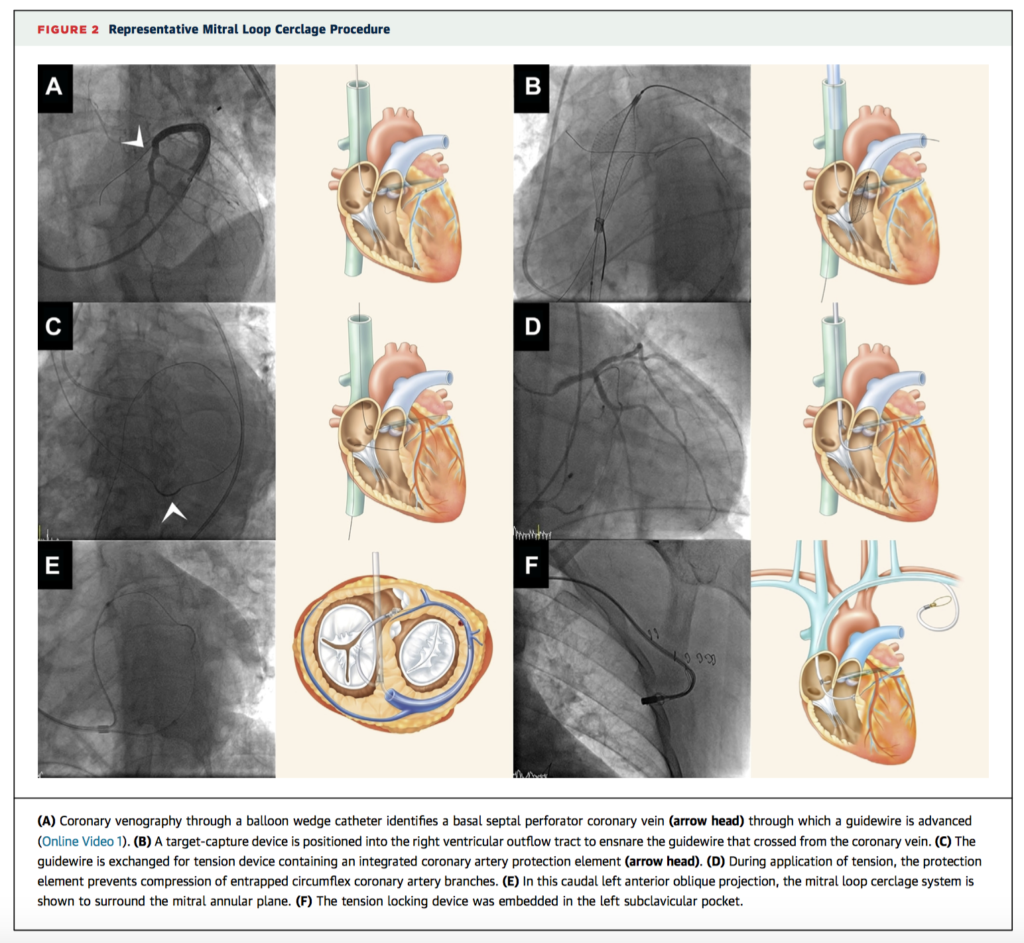
Secondary or functional mitral regurgitation (MR), where valve leaflets are normal but fail to coapt is common in the setting of left ventricular dysfunction and dilation. This first-in-human feasibility study shows promising results of a novel technique, transcather mitral loop cerclage annuloplasty. Of the five patients enrolled, device implantation was successful in four and aborted in one with atypical coronary venous anatomy. Post-procedural assessment and six month follow up revealed improved measures of MR, improved chamber dimensions, and a reversion to sinus rhythm from atrial fibrillation in two patients, suggesting structural and electrical remodelling. Complications included one myocardial infarction secondary to an entrapped marginal artery, one case of device migration, and one death due to refractory heart failure six weeks after implantation.
The 30 day results of the observational registry following 1947 patients from 10 countries who received third-generation SAPIEN 3 transcatheter aortic valves demonstrate good outcomes. Implantation success was high (98.3%), while conversion to surgery and need for cardiopulmonary bypass was rare (0.6% and 0.7%, respectively) and the overall rate of adverse events was low. 3.1% of patients had moderate or greater paravalvular regurgitation. Overall there were significant improvements in mean aortic valve gradient (P<0.0001), effective orifice area (P<0.0001) and a decrease in the proportion of patients with New York Heart Association Class III/IV symptoms (73.9% to 10.4% and 69.8% to 28.0%, both P<0.0001).
Cardiothoracic Surgery
Summarised by Andrew Haymet
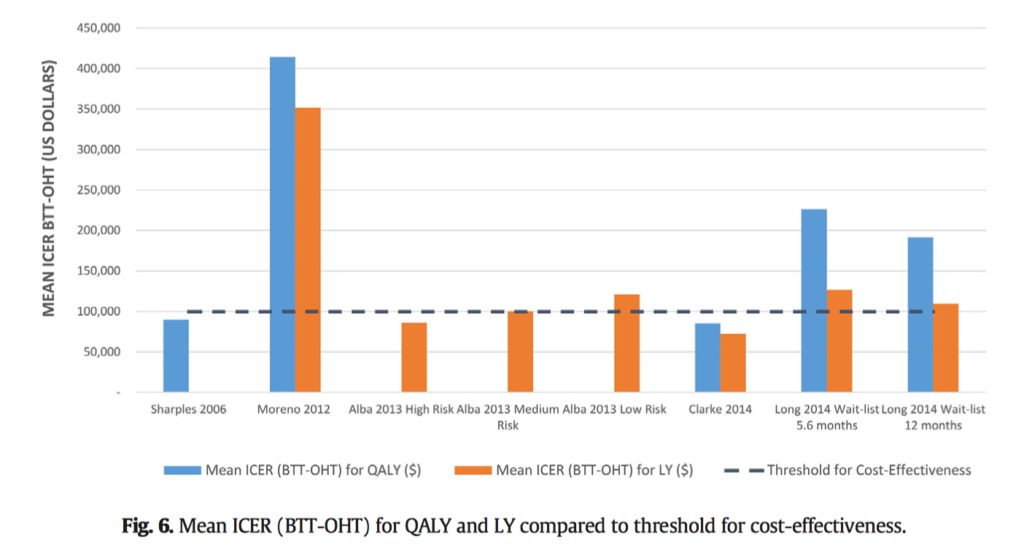
A systematic review of twenty studies was conducted to ascertain the clinical outcomes and cost-effectiveness of left ventricular assist devices (LVADs) used as a bridge to transplantation (BTT), compared to orthotopic heart transplantation (OHT) without a bridge. Meta analyses using summation of cost-effectiveness analyses were used to evaluate short and long-term post-transplantation outcomes. There was no difference in longterm post-transplantation survival (HR 1.24, 95% CI 1.00–1.54), acute rejection (HR 1.10, 95% CI 0.93–1.30), or chronic rejection and cardiac allograft vasculopathy (HR 0.99, 95% CI 0.73–1.36). The total cost of VAD BTT ranged from $316,078 to $1,025,500, and OHT ranged from $179,051to $802,200. The authors concluded that LVADs used as BTT did not alter post-transplantation long-term survival, rejection, and post-operative morbidity. LVAD BTT may be cost-effective, particularly in medium and high-risk patients with prolonged expected waiting times, those with renal dysfunction, or in young patients.
Veno-arterial (VA) extracorporeal membranous oxygenation may be employed to assist in managing life-threatening complications of transcatheter aortic valve replacement (TAVR). 46 patients underwent TAVR between December 2013 and February 2016, of whom 4 required emergency ECMO support and 3 received elective ECMO support. Indications for its emergent use were haemodynamic instability and cardiogenic shock, whilst its elective usage was indicated in severe pulmonary hypertension, impaired LV function, or both. There was no 30-day mortality, and no significant difference was found between the groups in 1-year survival at 83.3%. Although ECMO is support is rarely needed in TAVR, a thorough treatment strategy by the heart team is mandatory.
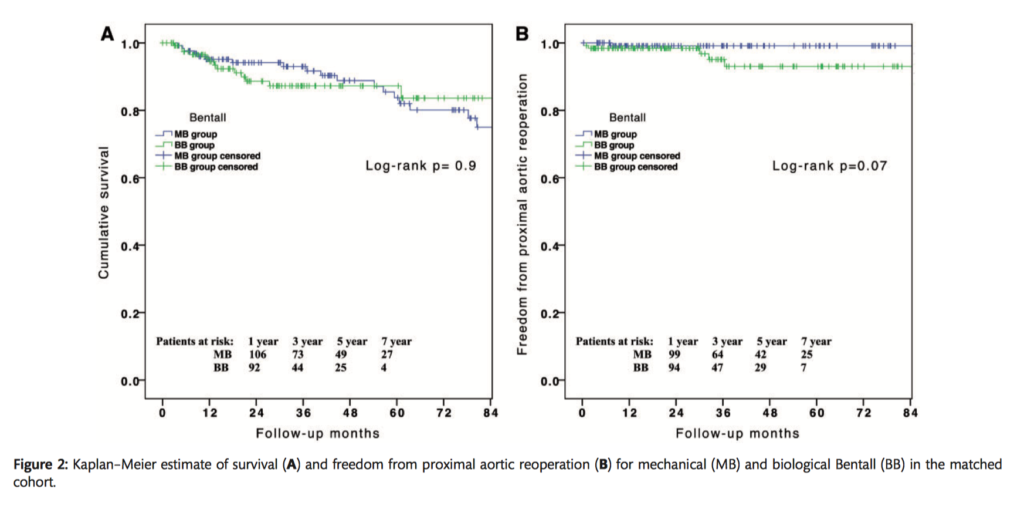
This propensity-matched analysis compared biological versus mechanical composite valve graft implantation for early mortality and morbidities and for late complications. 1112 consecutive patients underwent a complete aortic root replacement between 1978 and 2011. Hospital mortality was similar between the two groups (MB=7.2% and BB=5.8%, p=0.6). Propensity-adjusted Cox-regression analysis showed no relationship between prosthesis type and all-cause mortality at follow-up (HR 0.88, 95% CI 0.50-2.14, p=0.4). The authors concluded that the choice of a mechanical or biological graft appeared to have no influence on early to late midterm outcomes, including need for aortic reintervention.
Cardiac Imaging
Summarised by Sarah Catchpoole
The effect of transcatheter aortic valve replacement (TAVR) on diastolic function and whether there is any impact on clinical outcomes is unknown. In this single-centre retrospective cohort study, 90 patients underwent pre and post TAVR transthoracic echocardiogram and were followed up for one year. While diastolic parameters improved post-procedure, only pre-procedure diastolic dysfunction grade was associated with death at one year (hazard ratio, 1.163, P = 0.005) and combined death/cardiovascular hospitalisation (hazard ratio, 1.174; P = 0.018).
Gillam et al. Use of Imaging Endpoints in Clinical Trials. JACC Cardiovasc Imaging. 2017 Mar.
Data from cardiovascular imaging are fundamental not only for trials in medical, interventional and surgical cardiology, but in other fields where cardiovascular status impacts interventions and outcomes. It is therefore essential to ensure imaging measurements are reliable, valid and unbiased. This perspective article discusses the impact of imaging in the design of trials, standardisation and control of potential sources of bias, as well as the FDA guidance on imaging endpoints. The authors recommend best practice should include centralised, blinded image interpretation, standard operating procedures, and ongoing quality assessment and improvement.
Perioperative Medicine
Summarised by Andrew Haymet
Noninvasive ventilation (NIV) is commonly employed in the intensive care unit (ICU) to manage acute respiratory failure. This randomized, open-label trial aimed to demonstrate efficacy of NIV in improving oxygenation in patients who developed hypoxaemic respiratory failure after discharge from ICU. 64 patients were randomized to receive NIV or standard treatment. Continuous positive airway pressure use was associated with a statistically significant reduction in the number of patients with PaO2/FiO2<200 (4/33 (12%) vs 14/31 (45%), p=0.003). The authors concluded that administration of NIV on the main ward in patients with acute respiratory failure following cardiac surgery was associated with improved respiratory outcome.
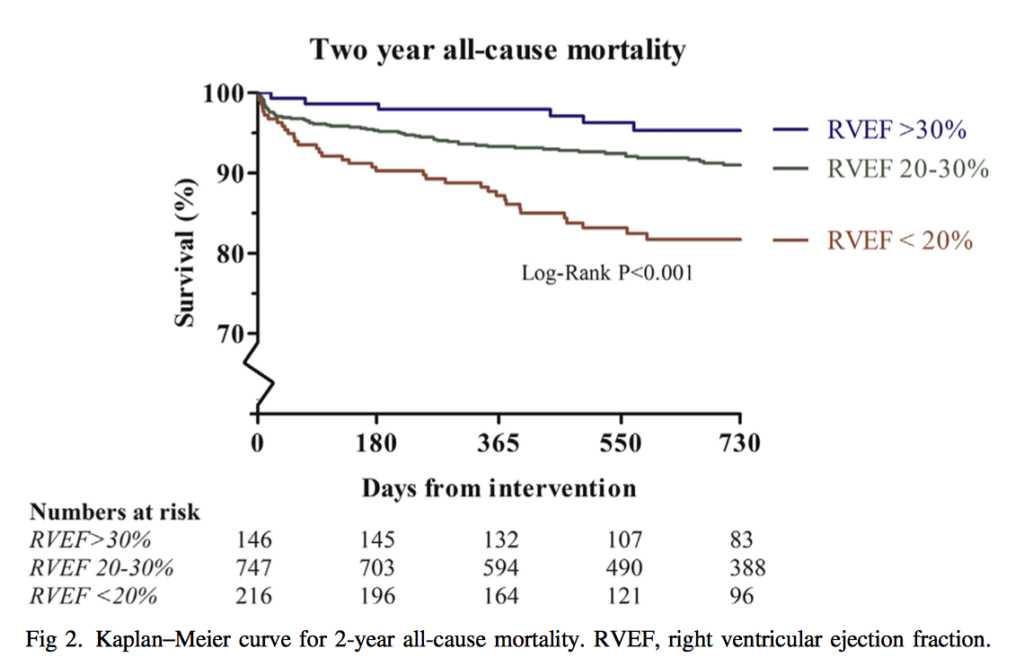
This retrospective analysis of 1,109 patients aimed to establish the all-cause mortality of right ventricular dysfunction after cardiac surgery over a four-year period in a tertiary teaching hospital. Primary outcome was 2-year all-cause mortality. Right ventricular ejection fraction was categorized into 3 subgroups: <20%, 20-30%, and >30%. In a multivariate analysis, RVEF as a continuous variable was associated independently with the primary outcome (odds ratio 0.95 confidence interval 0.91-0.99, p = 0.011.) Odds ratios for RVEF <20% were 1.88 (confidence interval 1.18-3.00, p = 0.008). The authors concluded that, in a heterogenic cardiac surgery population, RV function was associated independently with 2-year all cause mortality. Given this strong association, further research is warranted to further ascertain the aetiology of RV dysfunction in cardiac surgery.
Prolonged cardiopulmonary bypass (CPB) is associated with haemolysis, resulting in increased plasma oxyhaemoglobin and vascular nitric oxide depletion. The authors hypothesized in a prospective cohort study of 50 patients that haemolysis associated with CPB would reduce nitric oxide bioavailability, resulting in high pulmonary and systemic vascular resistance. These resistances were then hypothesized to normalize after CPB with clearance of plasma oxyhaemoglobin. Plasma hemoglobin and plasma nitric oxide consumption were measured before surgery and after CPB. Pulmonary and systemic vascular resistances, and plasma haemoglobin and nitric oxide consumption, were highest at 15 minutes after CPB and then decreased over time. The reduction in plasma nitric oxide consumption at 4 hours after CPB was an independent predictor of the concomitant reductions in pulmonary and systemic vascular resistances.