Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been published recently in each speciality (cardiology, cardiothoracic surgery, cardiac imaging, perioperative medicine).
Cardiology
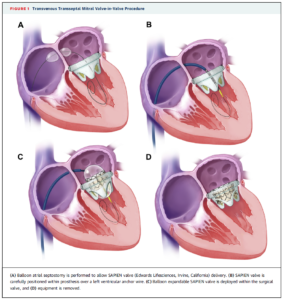
In the 10 years following mitral valve replacement or repair approximately 35% of patients require repeat surgery. This study examined the safety and feasibility of percutaneous, transfemoral, antegrade, transseptal mitral valve implantation in 48 patients. Patients selected had significant bioprosthetic mitral valve or annuloplasty ring dysfunction, or severe mitral stenosis due to mitral annular calcification (MAC) and comorbidities ruling out repeat sternotomy and valve replacement. The included patients had failed bioprosthesis (n=33), ring annuloplasty (n=9) or calcific mitral stenosis (n=6). All replacements were with Edwards SAPIEN prosthesis and immediate and mid-term outcomes were evaluated.
Despite the improved safety due to the less invasive nature of transcatheter mitral valve-in-valve procedures, challenges include the lack of direct visualization during valve positioning and the lack of direct fixation of the valve prosthesis. In this study, careful procedural planning was conducted including: i) size selection using manufacturers’ recommendations, CT and TEE derived measurements; ii) use of the valve-in-valve app to select valve size; iii) 3D CT of mitral annulus and leaflets to check for calcification in all 4 quadrants (for patients with calcific mitral stenosis); iv) consideration of ECMO support.
The procedure was successful in 88% of patients overall and in 94% of patients with failed bioprosthesis with an overall 30-day survival of 86%. Procedural complications included left ventricular perforation (6%), valve embolization (6%), emergency cardiac surgery (8%), major bleeding (8%), left ventricular pseudoaneurysm (2%) and death (6%).
“These findings should serve to advance the development of the transvenous transseptal approach for transcatheter mitral valve implantation,” the authors commented.
Accompanying editorial:
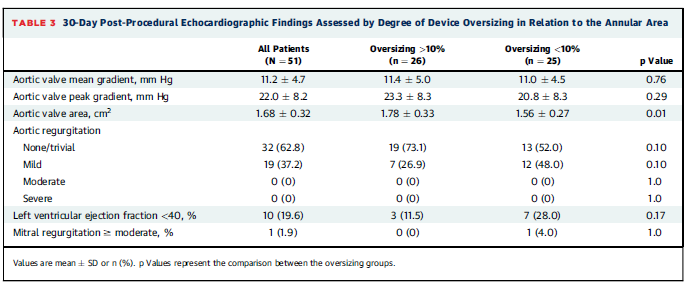
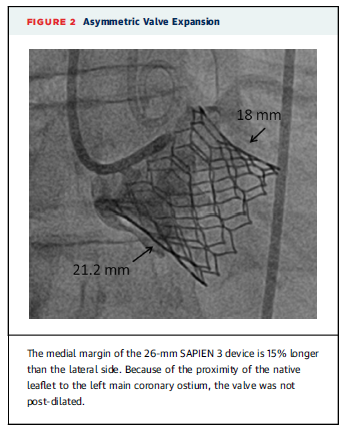
This study assessed the use of transcatheter aortic valve replacement (TAVR) with the Edwards SAPIEN 3 valve in 51 patients with bicuspid aortic valves and aortic stenosis. The mean age of patients was 76.2 years and the mean Society of Thoracic Surgeons Predicted Risk of Mortality score was 5.2. There were no intraprocedural deaths. The transthoracic echocardiographic evaluation at 30 days is shown in the table below. The researchers noted that on angiography the valve had tended to expand in an asymmetric manner in 38% of patients. The 30-day mortality was 3.9% and 12 patients (23.5%) required pacemaker implantation.
“The device success rate of 98% reported here is comparable to that reported with the same next-generation valve in patients with tricuspid aortic valves. Only 4 patients (7.6%) required post-implantation balloon dilation due to residual paravalvular regurgitation, a low rate compared with other recently reported bicuspid series where post-dilation was required in 18% to 30% of patients,” the researchers concluded.
In an accompanying editorial comment:
Dr Robert Guyton and Dr Muralidhar Padala comment that the outcomes of the study identify three red flags that will need attention: 1) higher mortality; 2) high rate of pacemaker requirement; and 3) high rate of asymmetrical deployment/incomplete stent expansion.
“As we consider extension of TAVR to lower risk patients, these 3 concerns—a higher mortality rate, a pacemaker rate of 10% to 25%, and incomplete stent expansion in 38% of patients—become magnified in importance,” wrote Dr Guyton & Dr Padala.
“A decrease in valve durability from 15 to 20 years down to 7 to 10 years becomes a major concern in those patients with longer life expectancy.”
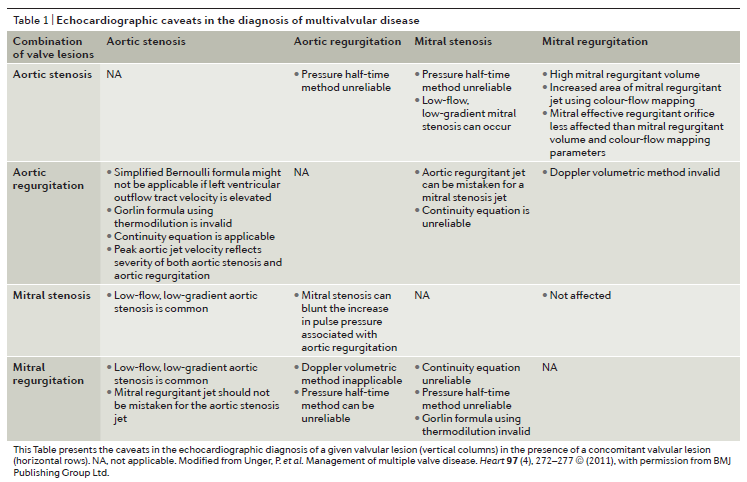
This comprehensive review addresses the management of multivalvular disease (MVD). Data from the EuroHeart survey estimated that 20.2% of all patients with valve disease and 14.6% of patients undergoing valvular surgery had MVD. Data from the Society of Thoracic Surgeons database (1993 – 2007) estimated that around 11% of valvular surgery patients were undergoing multi-valve replacement, with the largest group having both aortic and mitral valves replaced (57.8%), followed by mitral and tricuspid (31.0%) and aortic and tricuspid (3.3%). Triple-valve surgery was conducted in 7.9% of patients in this dataset.
The haemodynamic interactions between two or more valve lesions may alter the clinical expression of each singular lesion and the review authors point out that as diagnostic tools to evaluate stenosis or regurgitation have been validated in single-valve disease, they might not be valid for MVD. A useful table is presented in the review that outlines caveats in the echocardiographic diagnosis of MVD.
Cardiothoracic Surgery – Summarised by Andrew Haymet
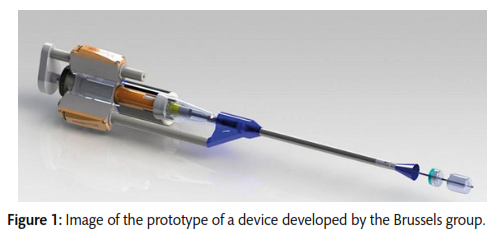
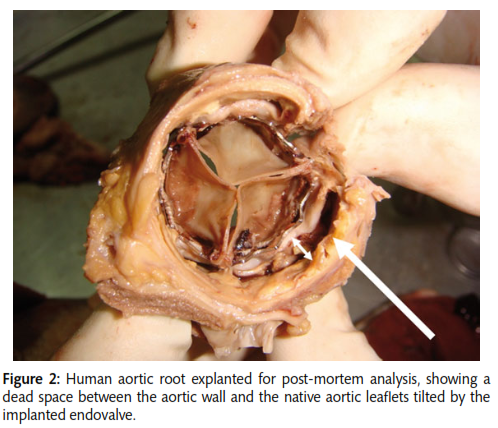
Transcatheter aortic valve implantation (TAVI) was introduced in 2002 as a rescue therapy for patients with severe aortic stenosis but ineligible for surgery. Complications of this technique have included stent deformation, paravalvular leakage, coronary ostial occlusion and embolization as a result of compression of the deployed TAVI stent against the calcified native aortic valve. This review of 21 papers between 2002 and 2015 describes numerous techniques of resecting the native aortic valve leaflets prior to TAVI to mitigate the risk of these complications. The resection techniques discussed included blade-based, laser and high-pressure water jet technologies. Blade-based devices seem to be suited to rapid endovascular resection performed within a few seconds, whilst resection using laser and water jet devices takes significantly longer and requires cardiopulmonary bypass or a ventricular-arterial shunt. A significant drawback of this technique is the miniaturization and motorization of a total procedure which includes both resection and implantation.
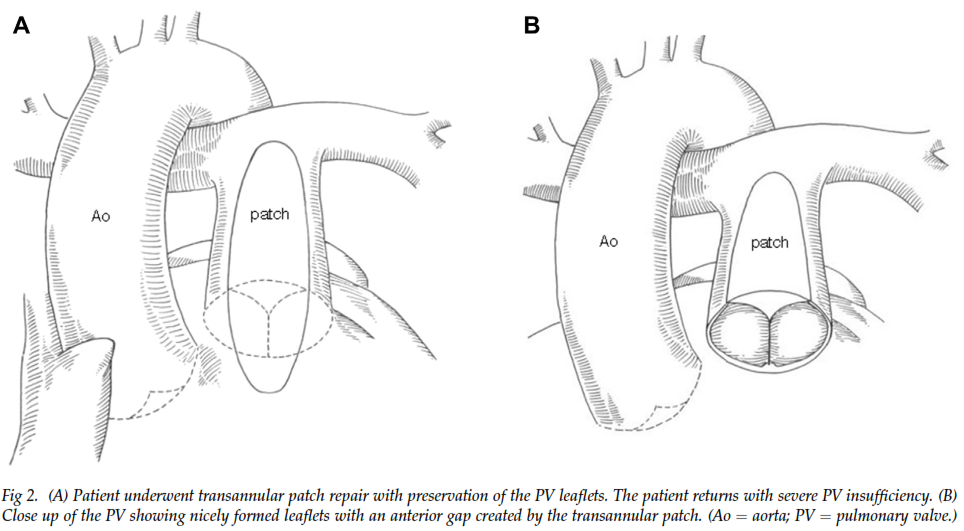
A retrospective review of 16 patients who underwent repair for acquired pulmonary valve (PV) insufficiency was conducted. Of these, 13 were born with Tetralogy of Fallot (TOF) and three had congenital critical pulmonary stenosis. After repair, all 13 patients with TOF showed marked reduction in PV insufficiency. All three patients with critical pulmonary stenosis showed a reduction in pulmonary insufficiency to a mild level, however two of these later relapsed. At early follow up, bicuspidization of the native PV in patients with TOF appeared to be efficacious, whilst those who underwent repair for torn leaflets exhibited deteriorating results over the longer term.
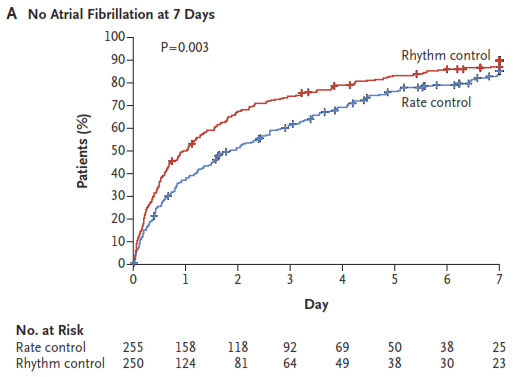
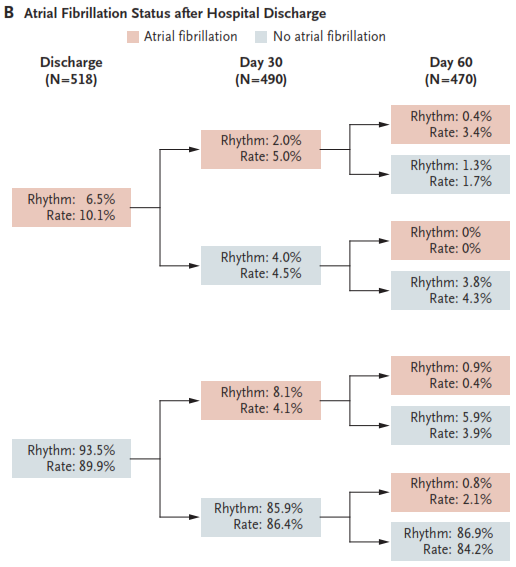
Atrial fibrillation (AF) after cardiac surgery is associated with increased mortality and confers substantial morbidity. In haemodynamically stable patients with postoperative AF, it remains unclear as to whether rate control or rhythm control should be the primary treatment strategy. In 2109 preoperatively enrolled patients, 695 developed postoperative AF and of these, 523 were randomized to either rate or rhythm control. The primary endpoint was total number of days in hospital 60 days after randomization. Both groups showed similar total numbers of days spent in hospital (median, 5.1 days and 5.0 days, respectively; P = 0.76). There were no significant differences in rates of death (p=0.64) or overall serious adverse events (P = 0.61). Neither treatment approach demonstrated a definitive clinical advantage over the other.
Cardiac Imaging
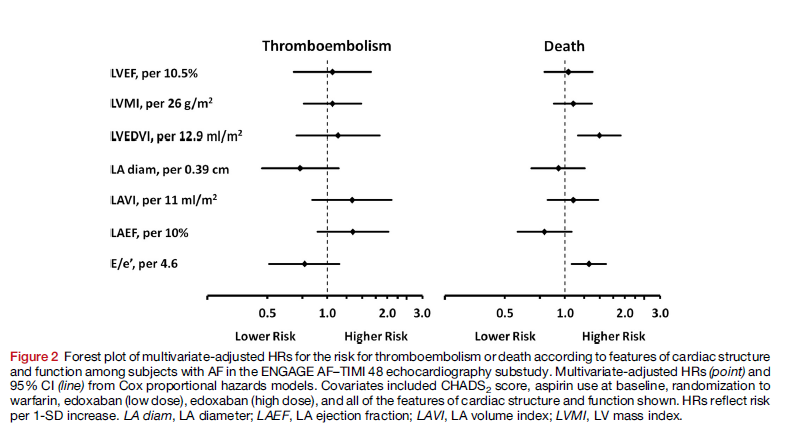
According to the results of a substudy of the ENGAGE atrial fibrillation (AF) thrombolysis in myocardial infarction trial, larger LV size and higher filling pressures were significantly associated with increased risk of death in a population of patients with AF at increased risk of thromboembolic events.
The AF-TIMI 48 trial compared the oral factor Xa inhibitor edoxaban with warfarin in 21,105 subjects for the prevention of ischaemic stroke, haemorrhagic stroke and systemic embolism in subjects with non-valvular AF and increased risk for thromboembolic events (CHADS2 score ≥ 2). In this prospective substudy 971 of these patients were evaluated for associations between cardiac structure and function and the risks for death and thromboembolism.
Over a median follow-up period of 2.5 years thromboembolism occurred in 4.9% and death occurred in 9.2% of subjects, with cardiovascular death accounting for the majority of deaths. In a statistical model that adjusted for CHADS2 score, it was found that none of the variables related to cardiac structure or function were associated with risk for thromboembolism. However, both larger LV end-diastolic volume index (LVEDVI) (HR 1.49; 95% CI, 1.16–1.91) and higher E/e´ (HR, 1.32; 95% CI, 1.08–1.61) were associated with increased risk of death.
The researchers concluded: “In a moderate- to high-risk population of subjects with AF enrolled in the echocardiographic substudy of ENGAGE AF–TIMI 48, we found that measures of cardiac structure and function were associated with increased risk for death, which was a more frequent event than thromboembolism, for which these measures were not predictive.”
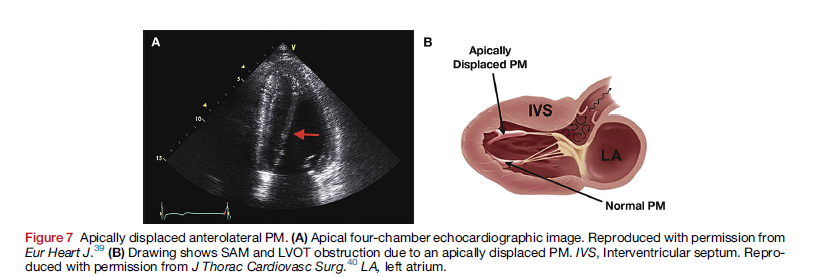
In this comprehensive overview of hypertrophic cardiomyopathy (HCM) the focus is on the abnormalities of the mitral apparatus (papillary muscles, leaflets, chords, and annulus) that may occur along with the characteristic ventricular hypertrophy. These abnormalities are important in the echocardiographic evaluation of patients with HCM.
Dr Silbiger outlines the normal anatomy and mechanics of the mitral apparatus and the mechanics of left ventricular outflow obstruction in HCM caused by systolic anterior motion of the mitral valve. Included in this review is a detailed discussion of echocardiographic evaluation of patients with HCM. Finally, differential diagnoses such as in athletes, cardiac amyloidosis and Anderson-Fabry disease are discussed.
In a particle image velocimetry and tissue doppler study of 36 participants the influence of left bundle branch block (LBBB) abnormalities on LV flow patterns was investigated. The patients all had normal ejection fractions; 20 had pacemakers, 6 had LBBB and the comparison group consisted of 10 healthy controls. Apical transverse motion (ATM) was measured to assess LV dyssynchrony and its impact on LV diastolic flow patterns.
In patients with pacemakers, both DDD and AAI modes were used when acquiring the data. When these patients were paced in DDD mode there was a significant decrease in ejection fraction compared to AAI mode. QRS was also significantly wider in DDD mode and the LBBB group compared to the AAI mode and controls.
The researchers observed that ATM was significantly higher in patients with LBBB abnormalities when compared to controls (mean 4.9 vs 1.0 mm; P < 0.001). They also noted that vortex energy dissipation was higher and the vortex duration time was shorter (28% vs 44%) in patients with LBBB.
The researchers concluded that:
“LV flow pattern analysis by echocardiographic particle image velocimetry reveals that conduction delay due to LBBB or pacemaker stimulation in the right ventricle (DDD) disturbs the transfer of kinetic energy during the cardiac cycle and causes less efficient LV function.”
Perioperative Medicine
This study of 45 individuals undergoing cardiopulmonary bypass provides evidence that norepinephrine use is not associated with significant changes in cerebral oxygen saturation.
Norepinephrine is a vasopressor used during cardiopulmonary bypass with the intention of increasing cerebral perfusion pressure through increasing systemic mean arterial pressure, which recommendations suggest should be kept at >70mmHg. Cerebral oximetery is used to monitor cerebral tissue oxygen saturation and reduced levels have been associated with poor outcomes including major organ dysfunction. Although norepinephrine is used to maintain mean arterial pressure, there are concerns it may induce cerebral vasoconstriction and contribute to cerebral hypoxia.
This study included patients undergoing cardiopulmonary bypass and aortic valve replacement who had norepinephrine administered to achieve a mean arterial pressure of approximately 80 mmHg. In a multivariate analysis no association between norepinephrine dose and cerebral tissue oxygen saturation was observed.
The authors commented that: “The lower confidence interval (CI) boundary corresponded to a <0.2% reduction in rSO2 with each 0.1 mg/kg/min NE-increment, which the authors did not believe to be relevant clinically.”
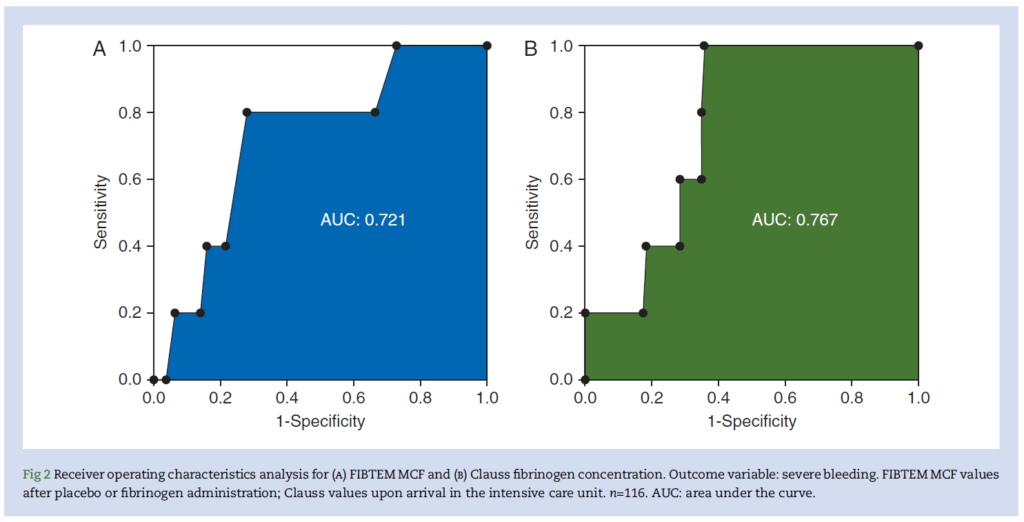
According to a subanalysis of 116 patients from the randomised controlled trial, Zero-Plasma (ZEPLAST), around a 2g dose of fibrinogen concentrate may be sufficient to prevent and treat postoperative bleeding following cardiac surgery.
In this study target fibrinogen values were assessed to determine optimal corresponding fibrinogen supplement dose. Fibrin-based thromboelastometry (FIBTEM) maximum clot firmness (MCF) and Clauss fibrinogen concentration after fibrinogen supplementation or placebo were the tests evaluated for their ability to predict postoperative severe bleeding.
The researchers noted a good correlation between the two tests. For a Clauss fibrinogen concentration of 287mg/dl there was a negative predictive value for severe bleeding of 100%. Similarly, for an FIBTEN MCF of 14 mm the negative predictive value for severe bleeding was 98%.
The researchers concluded that:
“Our evidence for lower target values for FIBTEM MCF suggests that the therapeutic dose of fibrinogen concentrate should probably be much lower than that reported previously, although further studies are required for confirmation.”
This case report discusses two cases of the rarely occurring pseudoaneurysm of the ascending aorta. Risk factors include previous cardiac surgery with poor surgical suture technique, pre-existing aortic wall disease, and perioperative infection.
The first case was a 2-year-old who had surgery for closure of a ventricular septal defect (VSD) one year before presenting to hospital with edema of the feet, facial puffiness, hoarseness and shortness of breath. ECHO revealed a PAA with fistulous communication to the right atrium (RA) (see figure below).
The second case was a 17-year-old who had surgery for closure of a VSD and aortic valve replacement for aortic regurgitation with a 25 St. Jude non-rotatable valve one year prior to presenting to hospital with pulsatile swelling of the chest that was increasing, episodes of chest pain, edema of the feet and raised liver enzymes suggestive of right heart failure.
The implications for anaesthetic management are also discussed in this case report.
Figure legend: Transthoracic echocardiography with colour flow Doppler showing neck of pseudoaneurysm of ascending aorta (PAA) and PAA-right atrium fistula.