Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been recently published in each speciality (Cardiology, Cardiac Surgery, Cardiac Imaging, Perioperative Medicine).
Cardiology
Summarised by Sarah Catchpoole
TAVR is increasingly being performed in patients with bicuspid aortic valve stenosis. This propensity score-matched study compared outcomes between 561 patients with bicuspid AS and 4,546 patients with tricuspid AS. Compared with patients with tricuspid AS, patients with bicuspid AS had more frequent conversion to surgery (2.0% vs. 0.2%; p = 0.006) and a significantly lower device success rate (85.3% vs. 91.4%; p = 0.002). TAVR in bicuspid AS was associated with similar prognosis but lower device success rate compared to tricuspid AS.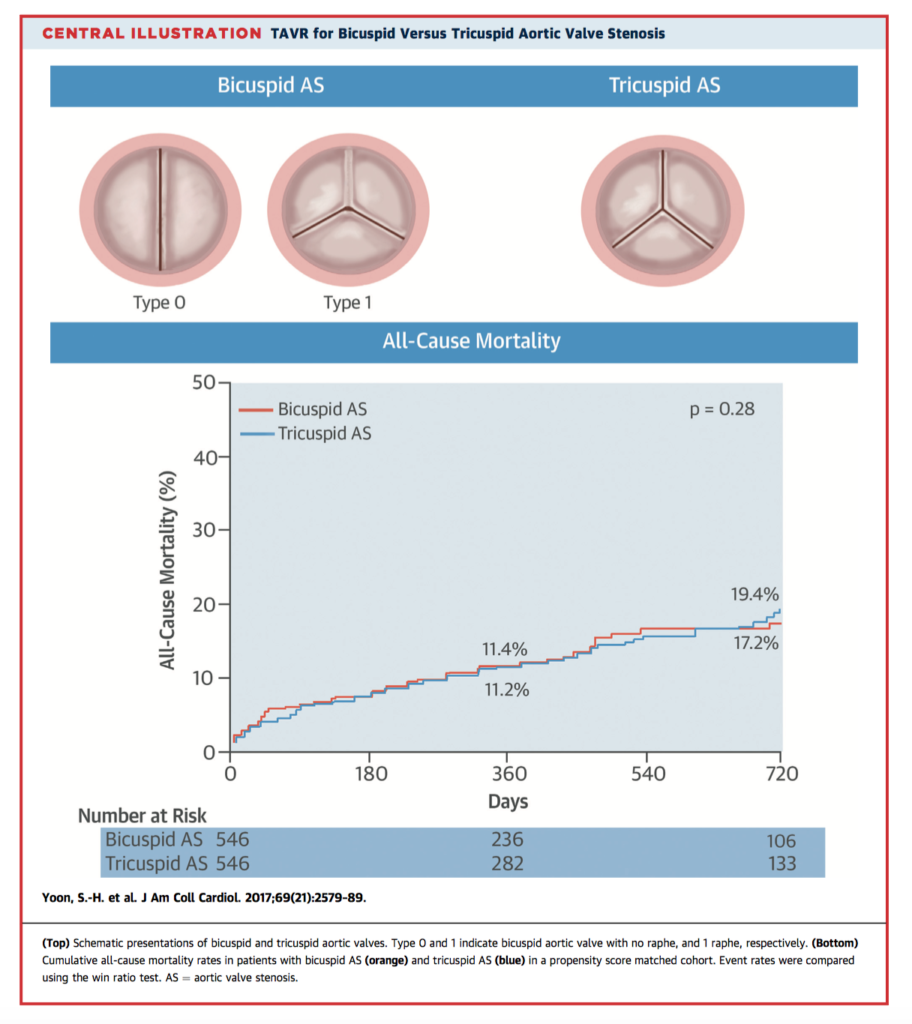
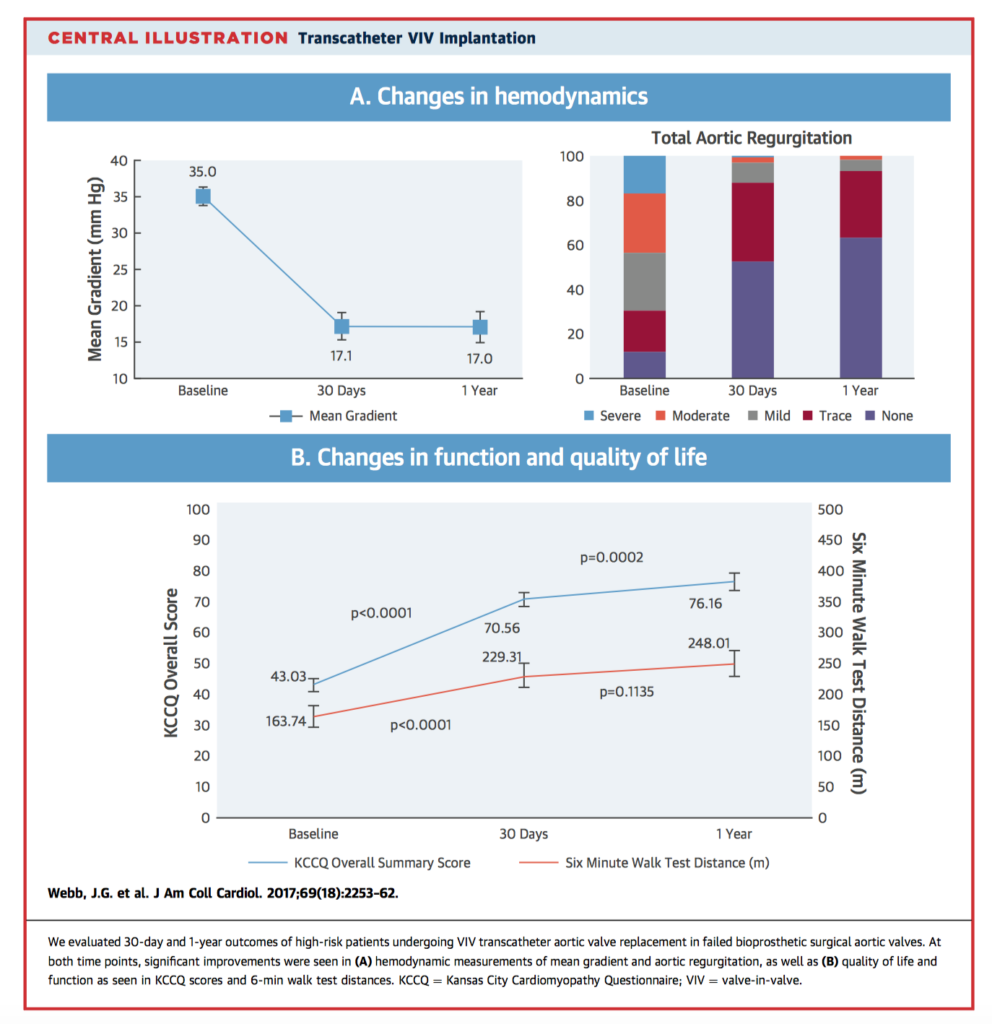
Early evidence suggests that valve-in-valve TAVR within failed bioprosthetic surgical aortic valves is a feasible therapeutic option with acceptable acute procedural results. 30-day and 1-year outcomes of a cohort of 365 high-risk patients undergoing VIV TAVR were studied. At 30 days, all-cause mortality was 2.7%, stroke was 2.7%, major vascular complication was 4.1%, conversion to surgery was 0.6%, coronary occlusion was 0.8%, and new pacemaker insertion was 1.9%. One-year all-cause mortality was 12.4%. The authors concluded that TAVR for bioprosthetic AVR failure is associated with relatively low mortality and complication rates, as well as sound functional and quality of life outcomes at 1 year.
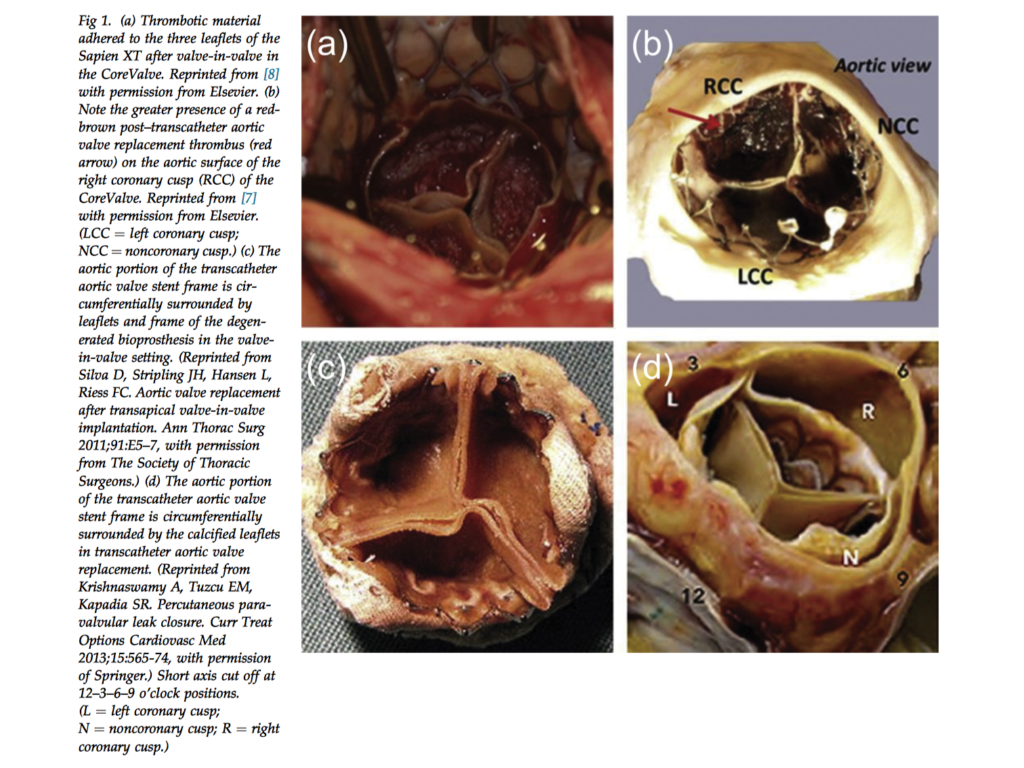
Valve leaflet thrombosis is an increasingly recognised complication of valve-in-valve (ViV) replacement. It is hypothesised that areas of flow disruption, as well as the foreign material of the prosthesis itself predisposes to thrombosis formation. In this computational study from the Denver University Cardiovascular Biomechanics Laboratory, 3D fluid-solid models of both surgical and transcatheter ViV replacement were developed using CT angiographic images from a standardised patient. Compared to the surgical model, the transcatheter model showed longer average blood in residence time (BRT), especially at the leaflet’s fixed boundary near the attachment of the valve frame. There was a similar pattern of BRT distribution for all three leaflets. In contrast, the surgical model demonstrated higher BRT particularly on the non-coronary leaflet.
Cardiac Surgery
Summarised by Andrew Haymet
Bioprosthetic valves, introduced commercially in the 1970’s, have become widely used compared with mechanical valves because they do not require anticoagulant treatment and they are associated with reduced rates of thrombotic complications. Their primary drawback is structural valve deterioration (SVD). This study of 54 papers collapsed 20 valve models into four types: Medtronic (Medtronic, Minneapolis, MN) and Edwards (Edwards Lifesciences, Irvine, CA) porcine, and Sorin (Sorin Group/LinaNova, London, UK) and Edwards pericardial. Sorin pericardial valves had significantly higher SVD risk with lower risk-adjusted mean time to failure. There were no significant differences in MTTF among the three other valves types.
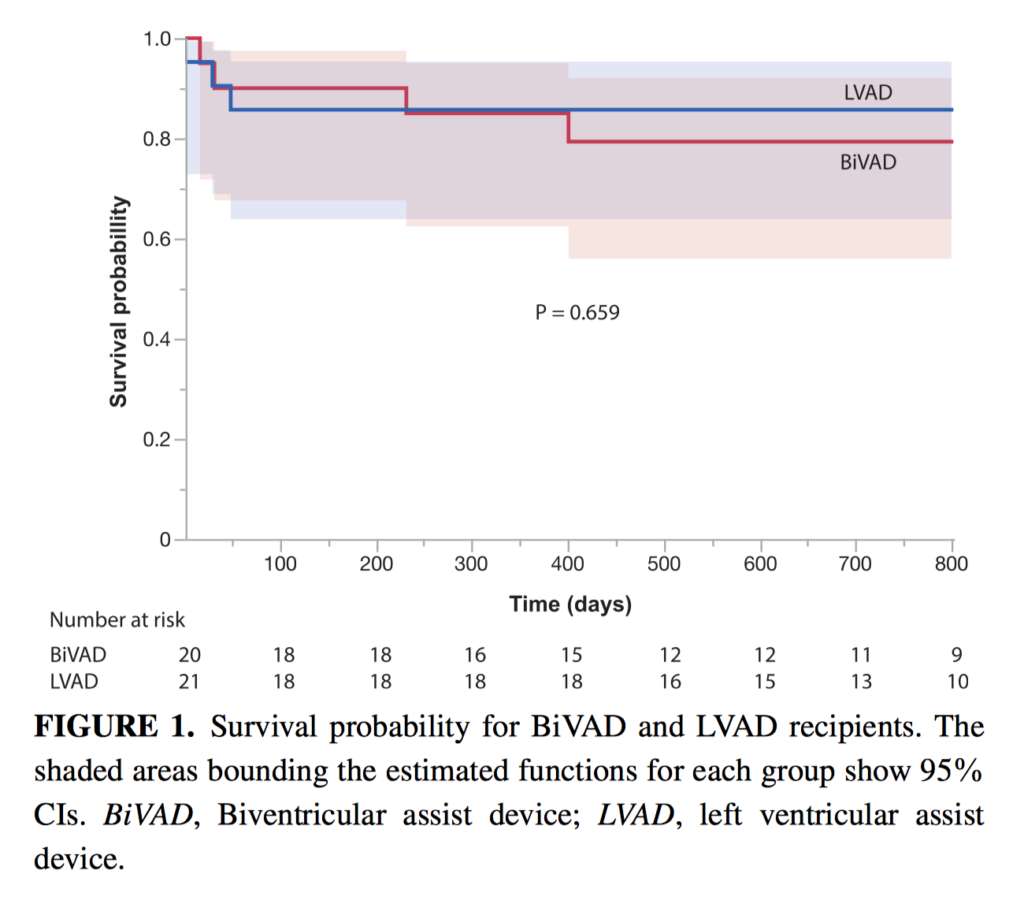
Right ventricular (RV) failure in patients treated using left ventricular assist devices is associated with poor outcomes. Between 2010 and 2014, 20 patients were assigned to receive biventricular assist devices and 21 patients to left ventricular assist devices as a bridge to heart transplantation, integrating estimated risk of postimplant RV failure. Survival on device to heart transplantation/weaning/destination for biventricular assist device and left ventricular assist device recipients was 90% versus 86% (not significant), with shorter heart transplantation waiting times for biventricular assist device recipients (median days, 154 vs 302, P <.001). The majority of both device recipients could be discharged home during transplant waiting time, and major stroke rates were comparable (55% versus 71% and 10% versus 10%, both non-significant). Aggressive use of a preplanned BiVAD as a bridge to transplantation for acutely ill patients with heart failure and for those with a high risk of post-implant RV failure appears to offer sound long-term outcomes.
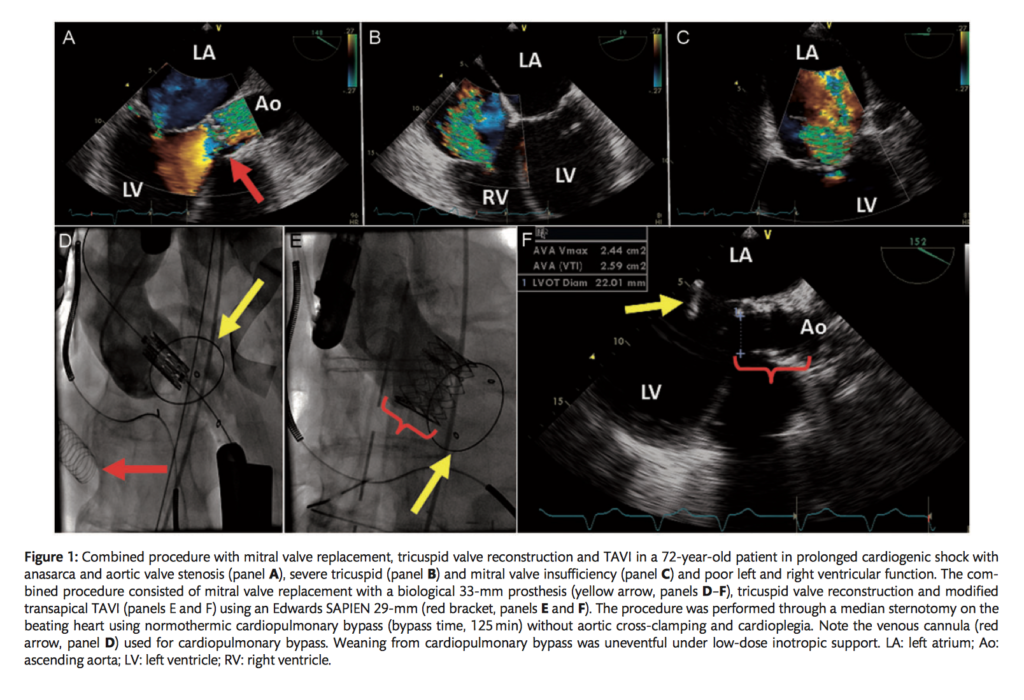
This retrospective, single centre observational cohort study of 120 patients investigated whether a beating heart mitral valve operation was of benefit in a heterogeneous, high risk group of patients requiring conventional mitral valve surgery. 58 patients (49%) had emergency or urgent procedures and 62 (51%) elective procedures. There were no conversions to conventional mitral valve procedures, and no intraoperative deaths. 30-day mortality rate for patients without cardiogenic shock was 7.5% (8 deaths among 106 patients). The authors concluded that patients deemed unsuitable for a conventional mitral valve operation had favourable outcomes if the procedure was performed on a beating heart.
Cardiac Imaging
Summarised by Sarah Catchpoole
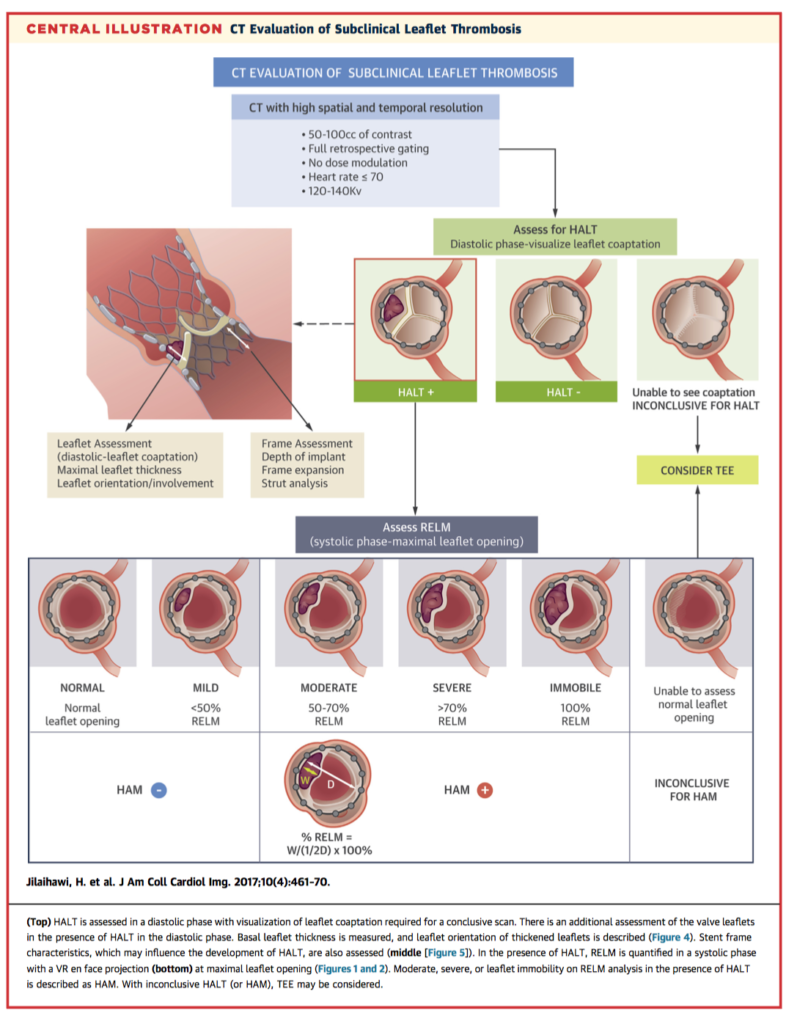
Subclinical leaflet thrombosis has been noted after all forms of aortic bioprostheses and is typically diagnosed by transoesophageal echocardiography. In this paper, the authors describe an alternative systematic CT methodology, previously validated and used in the Portico Trial. CT assessment has the advantages of being less invasive and less operator dependent. The author’s suggest this standardised approach could be used across clinical trials, as the significance of leaflet thrombosis and risk-benefit of treatment with anticoagulation is yet to be established. The protocol covers image acquisition, assessment for hypoattenuation associated with bioprosthetic leaflets (HALT), assessment for reduction of leaflet motion (RELM), and considerations specific to the type of bioprosthesis.
Correct device sizing is essential for the success of transcatheter closure of atrial septal defect (ASD). While balloon sizing is the gold standard, it is time-consuming and carries an increased risk of intraprocedural complications. In this prospective study, the authors sought to validate a new sizing formula that uses 3D transoesophageal echocardiography (TOE) in 248 consecutive patients with secundum ASD. The first tier received 3D TOE sizing with intraprocedural verification using traditional balloon sizing (n = 53), while the second tier received 3D TOE sizing alone (n = 195). In the first tier; estimated device size correlated well with stretched balloon diameter and final device size (P < 0.001, for all). Procedural success rate was 100% in the first tier and 99% in the second tier. Two patients experienced device embolization and were subsequently found to have unfavourable procedural anatomy. The authors conclude 3D TOE sizing is a feasible and safe alternative in appropriate candidates.
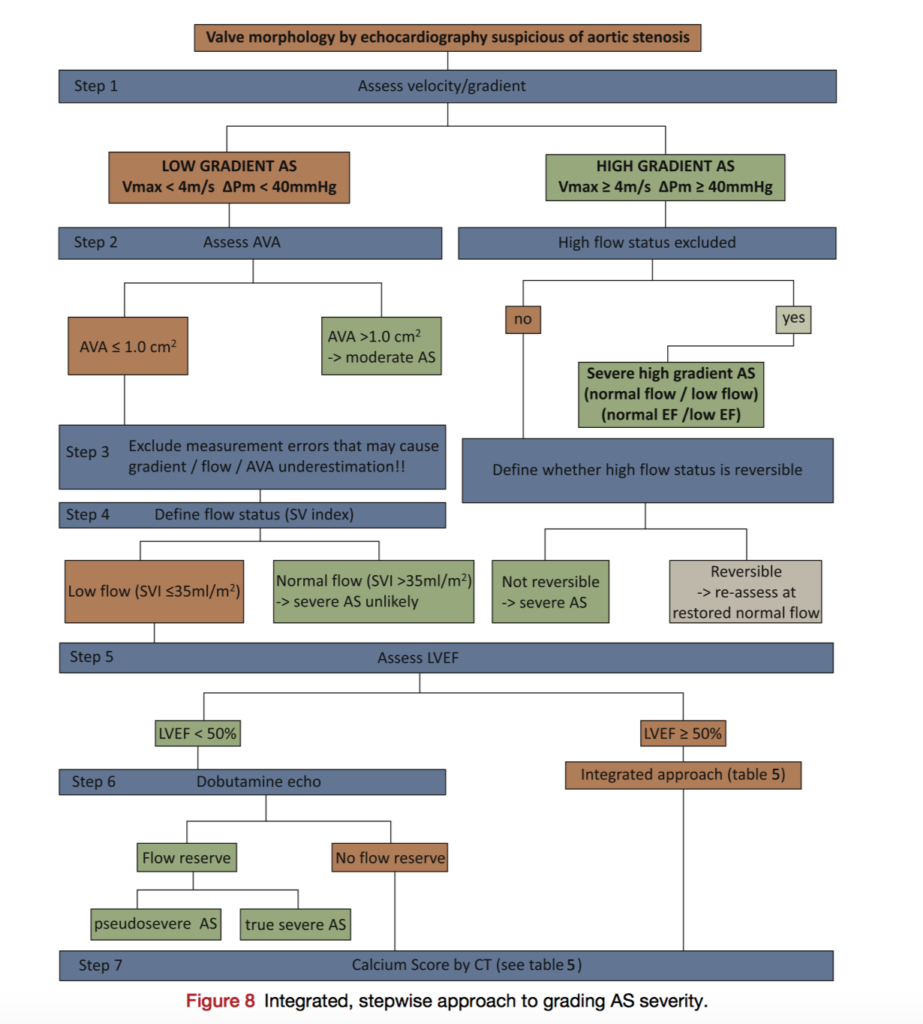
Contemporary research in aortic stenosis (AS) has made significant progress especially in the challenging clinical entity of low flow, low gradient AS. This focused updated guideline from the European Association of Cardiovascular Imaging and the American Society of Echocardiography will be essential for maintaining consistency across centres. Highlights of the update include assessment of low flow, low gradient AS with both reduced and preserved ejection fraction, optimisation of left ventricular outflow tract assessment, and a new classification of AS according to flow, gradient and ejection fraction.
Perioperative Medicine
Summarised by Andrew Haymet
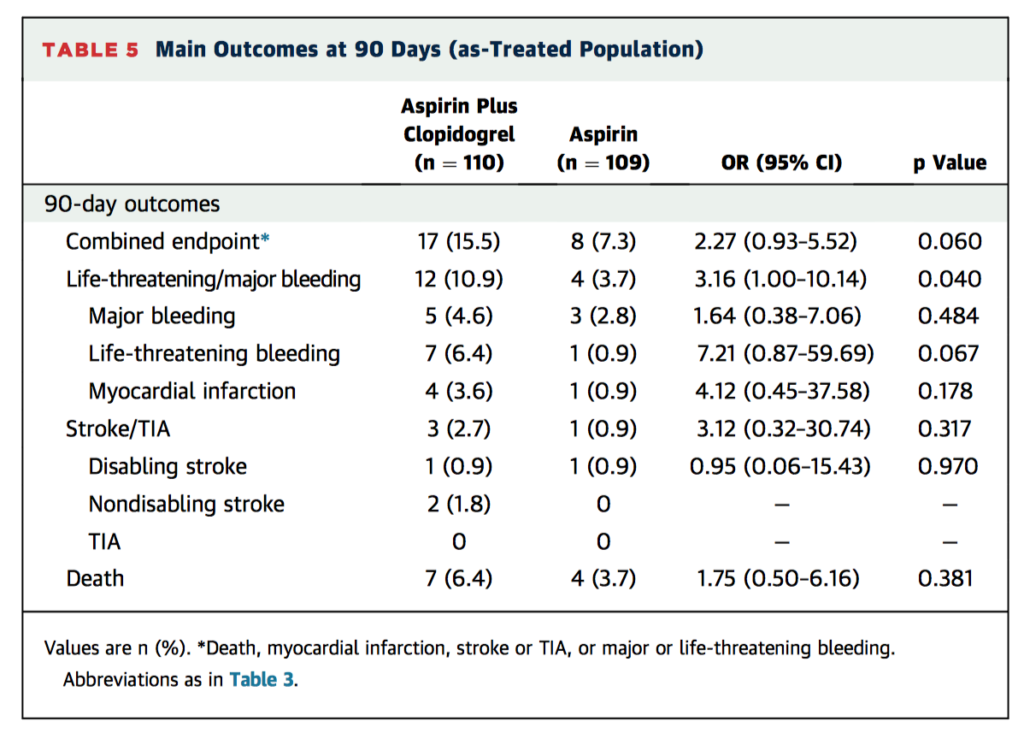
This randomized controlled trial of 222 patients compared the efficacy of aspirin plus clopidogrel (DAPT) versus aspirin (SAPT) alone as antithrombotic treatment following transcatheter aortic valve replacement (TAVR) for the prevention of ischaemic events, bleeding and death. There were no differences between groups in the occurrence of death (DAPT, 6.3%; SAPT, 3.6%; p = 0.37), MI (DAPT, 3.6%; SAT, 0.9%; p = 0.18), or stroke or transient ischemic attack (DAPT, 2.7%; SAPT, 0.9%; p = 0.31) at 3 months. DAPT was associated with a higher rate of major or life-threatening bleeding events (10.8% vs. 3.6% in the SAPT group, p = 0.038). There were no differences between groups in valve haemodynamic status post-TAVR. This small study concluded that SAPT decreased the risk for major or life-threatening events without increasing risk of MI or stroke.
This multi-institutional study of 21,821 patients receiving mitral valve repair or replacement between 1999-2011 aimed to demonstrate the role of perioperative stroke as an independent risk factor for in-hospital morbidity and mortality. In-hospital mortality was 5.5% and morbidity was 63.30% (p<0.05). The rate of perioperative stroke was 3.89% after isolated mitral valve surgery (p<0.05). Perioperative strokes were found to be the strongest risk factor for postoperative mortality (odds ratio 2.34, 95% confidence interval 1.83-2.98) and morbidity (odds ratio 4.53, 95% confidence interval 3.34-6.15). The trends in the last 10 years suggest decreasing mortality, but increasing morbidity. Preoperative risk stratification and intraoperative identification for impending strokes appear warranted.
The use of cardiopulmonary bypass (CPB) is associated with acute kidney injury. Proposed pathophysiology has included inflammation, micro-embolization and hypoperfusion. This prospective study evaluated the systemic and renal effects of increased pump flow during CPB in ten patients receiving cardiac surgery >60 minutes in duration. Filtration fraction was measured using 51Cr-EDTA infusion clearance, and as a primary outcome, renal oxygen extraction was measured [(arterial – renal vein O2 content)/arterial O2 content]. Increasing pump flow index from 2.4 to 3.0 l min-1 m-2, increased DO2I by 30 %. This was accompanied by 20% decrease in renal oxygen extraction. Filtration fraction was maintained, suggesting that GFR increased in proportion to the increase in renal perfusion. The authors concluded that impaired renal oxygenation seen during CPB may be counteracted by increasing pump flow rates above conventionally maintained levels.













