Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been recently published in each speciality (Cardiology, Cardiac Surgery, Cardiac Imaging, Perioperative Medicine).
Summarised by Sarah Catchpoole
The age of personal devices is felt by many to offer great promise for medicine and personal health. The Kardia Band (KB) is a novel technology that integrates with a wearable smart watch and allows recording of a rhythm strip (lead I) for 30 seconds. This study compared the KB and its interpretation algorithms to physician interpreted 12 lead ECG and rhythm strips for detection of atrial fibrillation (AF). From 100 enrolled patients with known AF, 169 simultaneous ECG and KB recordings were generated and reviewed in a blinded, prospective design. The KB alone had 93% sensitivity and 84% specificity compared to ECG (K=0.77) but also generated 57 non-interpretable recordings. On physician review, KB recordings had 99% sensitivity and 83% specificity (K=0.83) and the 57 non-interpretable recordings had 100% sensitivity and 80% specificity (K=0.74). The authors conclude the KB, when supported by physician interpretation, is a useful tool for detecting AF in a clinical setting.

Figure: Using the Kardia Band to record a lead I rhythm strip. Image taken from AliveCor website.
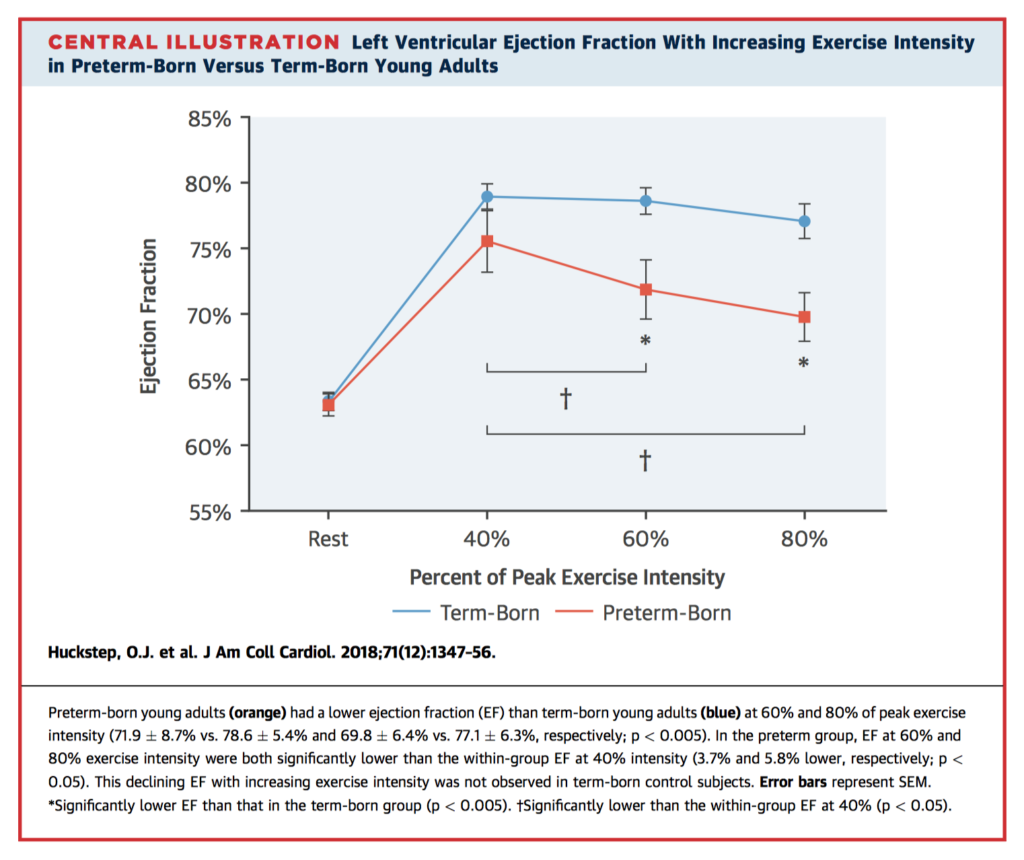
Recent large scale epidemiological studies have identified pre-term birth as a risk factor for heart failure in childhood and adolescence. In this observational case-control study, 101 young adults age 18-40 (54 term, 47 preterm of which 80% were born at 32-36 weeks) underwent comprehensive cardiovascular assessment including anthropometry, biochemistry, blood pressure monitoring, cardiopulmonary exercise testing, and full resting and stress echocardiography. Structurally, those born preterm had greater LV mass and lower LV volumes relative to body surface area, lower peak systolic longitudinal strain, and lower E-to-A ratio and velocity time integral. While LV ejection fraction (LVEF) was no different at rest, preterm born adults had significant declines in LVEF with increasing exercise intensity (Central Illustration), in addition to lower submaximal cardiac output reserve.
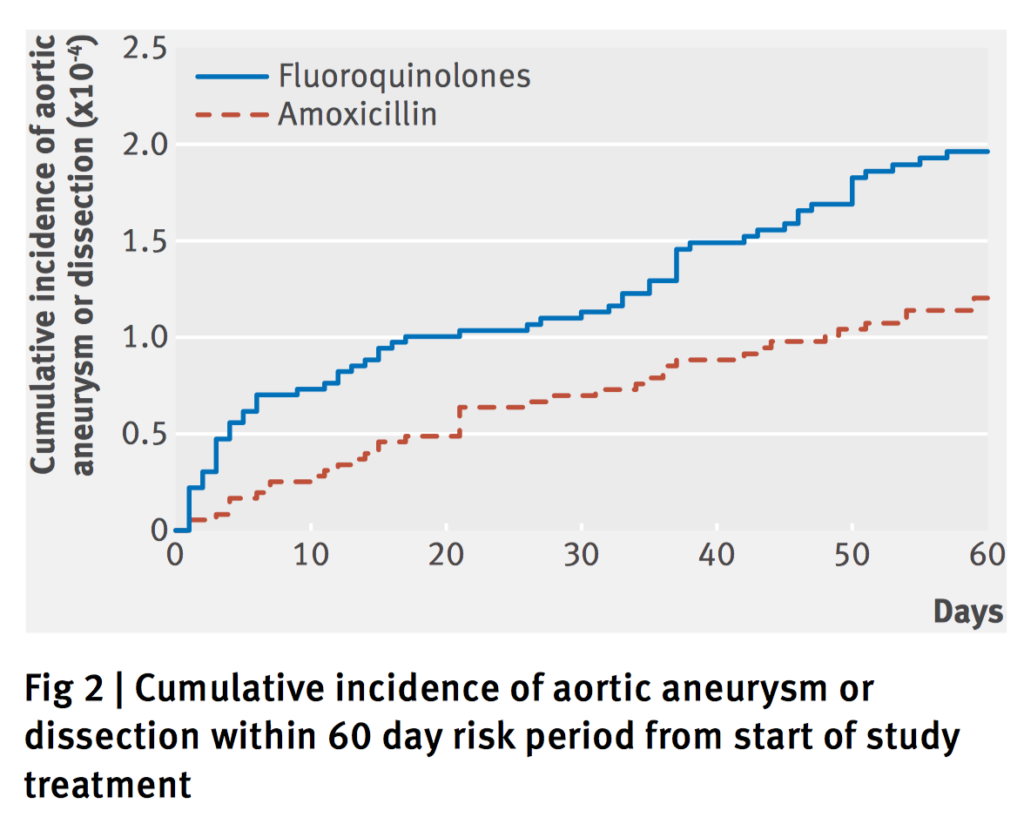
Fluoroquinolones are known to induce degradation of collagen by stimulating matrix metalloproteinases and have been associated with tendinopathy and Achilles tendon rupture. Two recent observational studies have also noted a potential two-fold increased risk of aortic aneurysm and dissection. In response, this nationwide, propensity score matched cohort study of adults >50 years was conducted using Swedish registry data from 2006-2013. Amoxicillin was the chosen comparison antibiotic as it is prescribed for similar indications and has no known association with aortic pathology. There were 2 333 219 treatment episodes of fluoroquinolone or amoxicillin use; after eligibility criteria application and 1:1 propensity matching, there were a total of 360 088 episodes per group. Within a 60 day risk period from commencement of treatment, fluoroquinolone use was associated with a 66% increased rate of aortic aneurysm or dissection (HR=1.66, 95% CI 1.12-2.46); the result appears largely driven by the increased rate of aortic aneurysms (HR=1.90 for aortic aneurysm, HR=0.93 for aortic dissection). While the overall absolute difference was 82 cases per 1 million treatment episodes, the authors stress the widespread use of fluoroquinolones.
Summarised by Andrew Haymet
This study of 40 patients investigated coronary haemodynamics in response to transcatheter aortic valve implantation (TAVI). Primary endpoints were coronary flow reserve (CFR) and fractional flow reserve (FFR). CFR remained unchanged, and FFR was 0.90 +/- 0.08 before and 0.93 +/- 0.08 after TAVI (p=0.0021). The TAVI –induced increase in FFR was due to a decrease in hyperaemic mean aortic pressure (p=0.0099). The authors concluded that CFR appeared not to be acutely affected by LV afterload reduction among patients with severe AS in response to TAVI. However, it was found to improve FFR via lowering of mean aortic pressure.
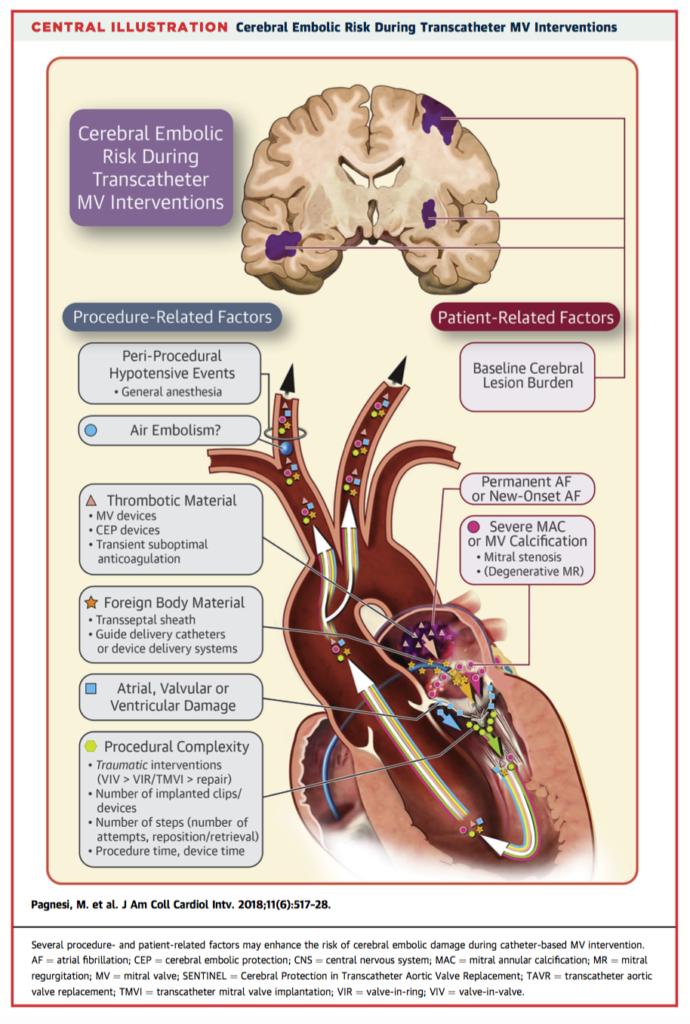
As new transcatheter mitral valve interventions continuously evolve, potential procedure-related adverse events demand careful investigation. The risk of cerebral embolic damage is ubiquitous in any left-sided structural heart intervention (and potentially linked to long term neurocognitive sequelae). Therefore, efforts to evaluate these aspects in the field of catheter-based MV procedures are justified. Early scientific evidence suggests that cerebral embolization during transcatheter MV interventions is common (rates of overt and covert cerebral injury up to 7% and 86% respectively) and remains poorly defined. The authors concluded that the paucity of available data prevents definitive conclusions on the incidence, mechanisms and implications of periprocedural neurological injury. Only future large, dedicated studies will determine whether this is a real clinical issue or an academic curiosity.
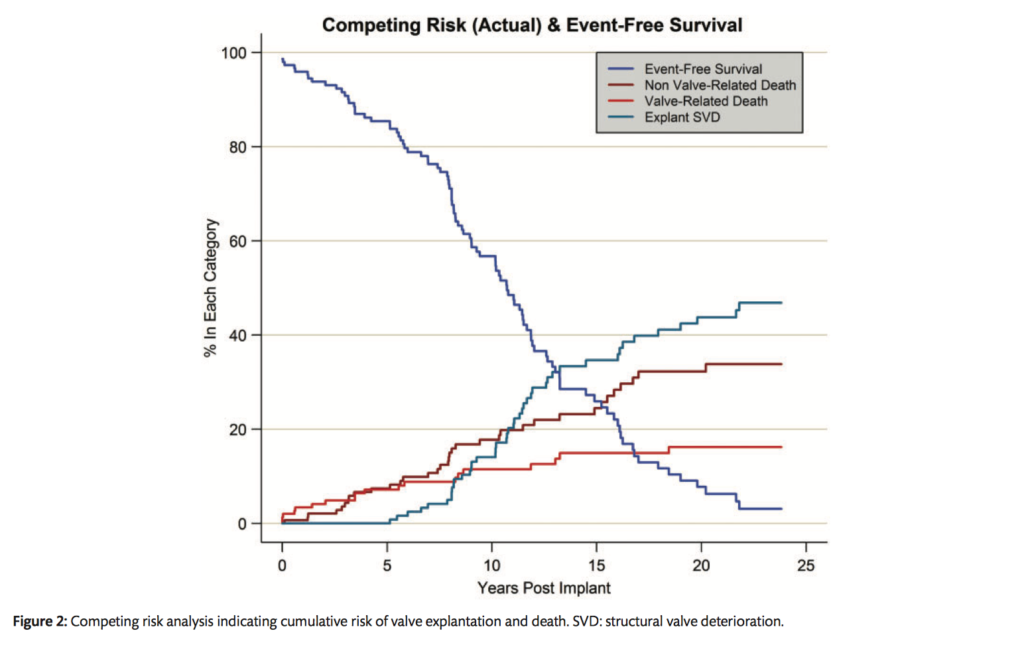
Bioprosthetic mitral valve replacement in young patients remains controversial because long term data are missing. This study evaluated the long term results of 148 Carpentier-Edwards PERIMOUNT mitral bioprostheses were implanted in 148 patients aged 65 years or younger between 1984 and 2010. The mean follow-up period was 8.6 ± 5.5 years, for a total of 1269 valve-years. Operative mortality rate was 2.0%. Fifty-one late deaths occurred (linearized rate 4.0% per valve-year). Actuarial survival rates averaged 70 ± 4%, 53 ± 6% and 31 ± 7% after 10, 15 and 20 years of follow-up, respectively. Actuarial freedom from structural valve deterioration (SVD) at 10, 15 and 20 years was 78 ± 5%, 47 ± 7% and 19 ± 7%, respectively. Reoperation was associated with no operative mortality. Expected valve durability was 14.2 years for this age group. In the selected patients aged 65 years or younger undergoing mitral valve replacement with a pericardial bioprosthesis, the expected valve durability was 14.2 years. Reoperation for SVD was associated with a low risk of mortality.
Summarised by Sarah Catchpoole
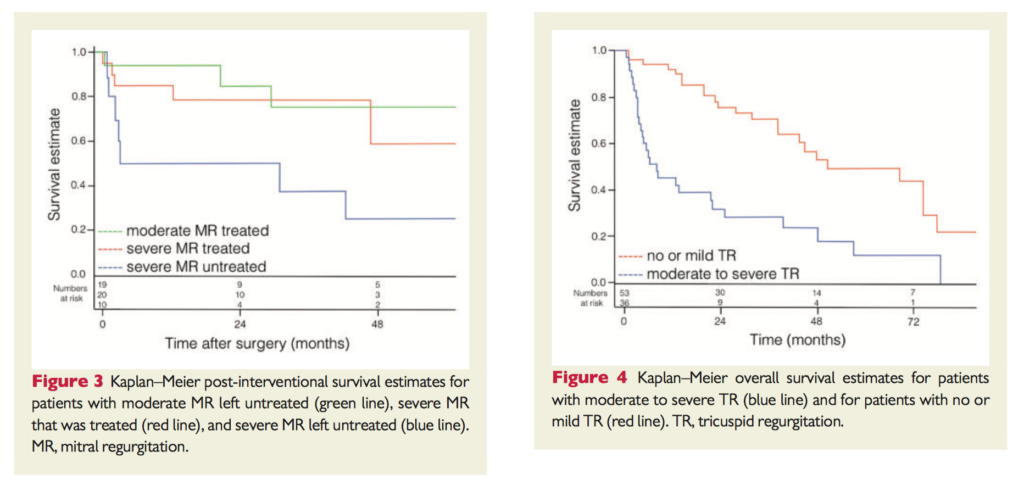
Multiple valve disease is increasingly common and is associated with poor outcomes after both surgical and transcatheter aortic valve replacement. In this prospective, observational study, 89 consecutive patients with severe AS and at least moderate mitral regurgitation (MR) were followed up for a median of 47.2 months. 35 patients were managed conservatively. Overall adjusted survival was higher in those who underwent a valve procedure of any kind within 4 months (hazard ratio=0.5, p=0.032). While concomitant mitral valve surgery (n=20) improved survival, this was non-significant. 36 patients also had concomitant moderate to severe tricuspid regurgitation (TR) – of those that underwent valve surgery, 7 of 14 (50%) were deceased within 3 months postoperatively, compared to only 1 of the 25 patients (3%) without TR. The authors conclude multiple valve disease, especially TR, indicates a high-risk population.
This elegant in-depth analysis of the physiology of the stenotic aortic valve – at rest, under stress, and after transcatheter aortic valve replacement (TAVR) – offers new insights towards the observed dynamic behaviour of the aortic valve and limitations of anatomic measures such as aortic valve area. In 16 patients undergoing routine TAVR, graded dobutamine infusions pre and post implantation were performed with a set up as shown in Figure 1. Pre-implantation stenotic aortic valves did not behave like either a resistor or orifice, showing a flow-dependent geometry. Post-TAVR however, the aortic valve behaves like a pure linear resistor (See Figure 2). The authors suggest evaluation of ‘valvular fractional flow reserve’ as a potential indication for aortic valve intervention, especially in patients with mild symptoms at rest.
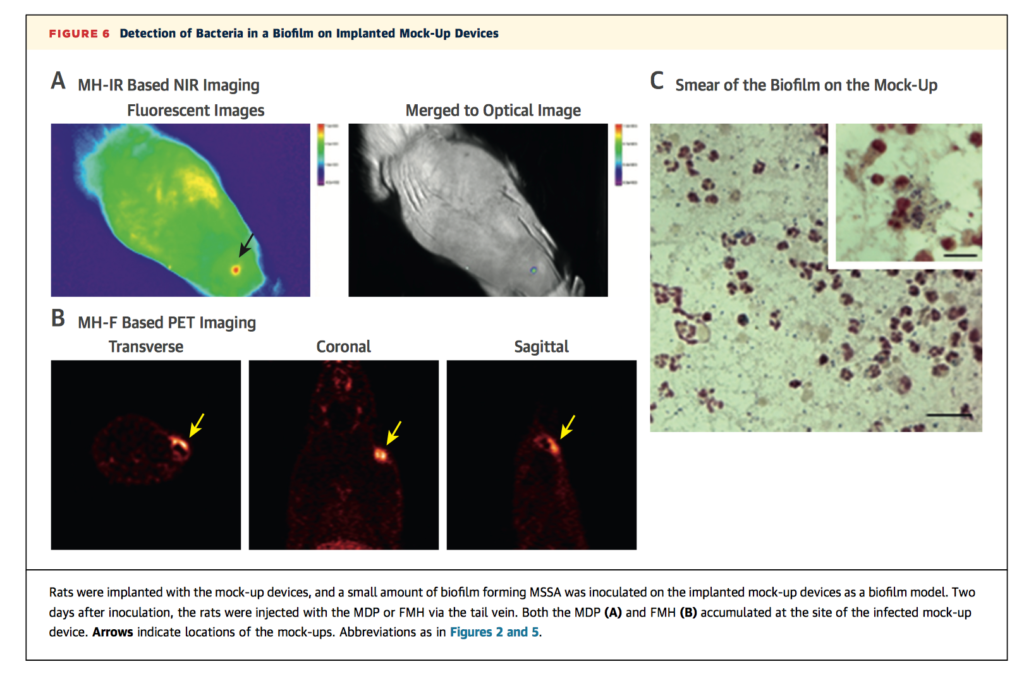
Implantable cardiovascular devices offer clear clinical benefit but carry a risk of device infection of approximately 0.5% for primary insertion, and higher rates for any revision or replacement. Earlier detection and treatment, especially in high-risk patients, could reduce extraction rates, morbidity, mortality, and costs. In a rat model, the authors assessed the sensitivity and specificity of maltohexaose-based imaging probes to detect infection compared to fluorodeoxyglucose (FDG). The probes exploit the high uptake of the bacterial specific maltodextrin transport system, are non-toxic, and are quickly cleared from non-infected tissue. Rats were implanted with subcutaneous stainless steel device mock ups and either left sterile (control) or injected post-operatively with staphylococcus areus (infection group) or oil of turpentine (inflammation group). Both the maltohexaose fluorescent dye probe and F18 fluoromaltohexaose PET imaging showed accumulation around devices in the infection group, but not in the inflammation or control groups. Consistent with its known poor specificity, FDG PET imaging was unable to distinguish between inflammation and infection. The authors conclude the maltahexoase-based probes are promising, and could also have potential in broader infectious diseases applications.
Summarised by Andrew Haymet
Cerebral injury is an important complication following cardiac surgery with the use of cardiopulmonary bypass. It is unclear whether higher versus lower blood pressures during CPB reduces cerebral infarction in these patients. This patient- and assessor-blinded randomized trial allocated 197 patients to a higher (70–80 mmHg) or lower (40–50 mmHg) target for mean arterial pressure by the titration of noradrenaline during cardiopulmonary bypass. Overall, DWI revealed new cerebral lesions in 52.8% of patients in the low-target group versus 55.7% in the high-target group (p = 0.76). The primary outcome of volume of new cerebral lesions was comparable between groups, 25 mm outcome of volume of new cerebral lesions was comparable between groups, 25 mm3 interquartile range [IQR], 0-118; range 0-25261) in the low-target group vs 29 mm3 (IQR 0-143; range 0-22116) in the high-target group (median difference estimate, 0 (95% confidence interval [95% CI] -25 – 0.028); P=0.99). No significant difference was observed in frequency of severe adverse events. The authors concluded that targeting a higher versus lower MAP during CPB did not seem to affect the volume or numbers of new cerebral infarcts.
Acute kidney injury (AKI) occurs frequently after cardiac surgery. This study of 90 patients undergoing mitral valve surgery investigated whether levosimendan administration could reduce AKI incidence in a high-risk cardiac surgical population. Patients were randomly assigned to receive levosimendan (0.025-0.2 μg/kg/min) or placebo in addition to standard inotropic treatment. Postoperative AKI occurred in 14 (30%) patients in the levosimendan group versus 23 (52%) in the placebo group (absolute difference –21.8; 95% confidence interval –41.7 to –1.97; p = 0.035). The incidence of major complications also was lower (18 [39%]) in the levosimendan group versus that in the placebo group (29 [66%]) (absolute difference –26.8 [–46.7 to –6.90]; p = 0.011). The authors concluded that levosimendan may improve renal outcome in cardiac surgery patients with chronic kidney disease undergoing mitral valve surgery who develop perioperative myocardial dysfunction. Results of this exploratory analysis should be investigated in future properly designed randomized controlled trials.
Prolonged intubation following cardiac surgery is associated with significant morbidity. A fast-track extubation protocol primarily driven by bedside providers was instituted for all postoperative cardiac surgery patients to facilitate safe and expeditious extubation. A retrospective review of 1581 cardiac surgery patients over an 8 year period was performed. Prior to 2011, non-protocolized standard perioperative management was utilized (n=807). From 2011 onwards, a fast-track extubation (FTE) protocol was instituted (n=774). Prior to instituting the FTE protocol, the rate of early extubation (<6 hours) was 43.7%, and increased to 64.1% during the FTE-era (P<0.001). Median time to extubation was also found to be significantly decreased (295 [IQR: 288] min vs. 385 [IQR: 362] min; P=0.041). There was no statistically significant difference in reintubation rates or 30-day mortality. The institution of a bedside provider-directed FTE pathway reduced overall intubation times and increased the rate of early extubation, without an increase in reintubation or mortality.













