Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been recently published in each speciality (Cardiology, Cardiac Surgery, Cardiac Imaging, Perioperative Medicine).
Cardiology
Summarised by Sarah Catchpoole
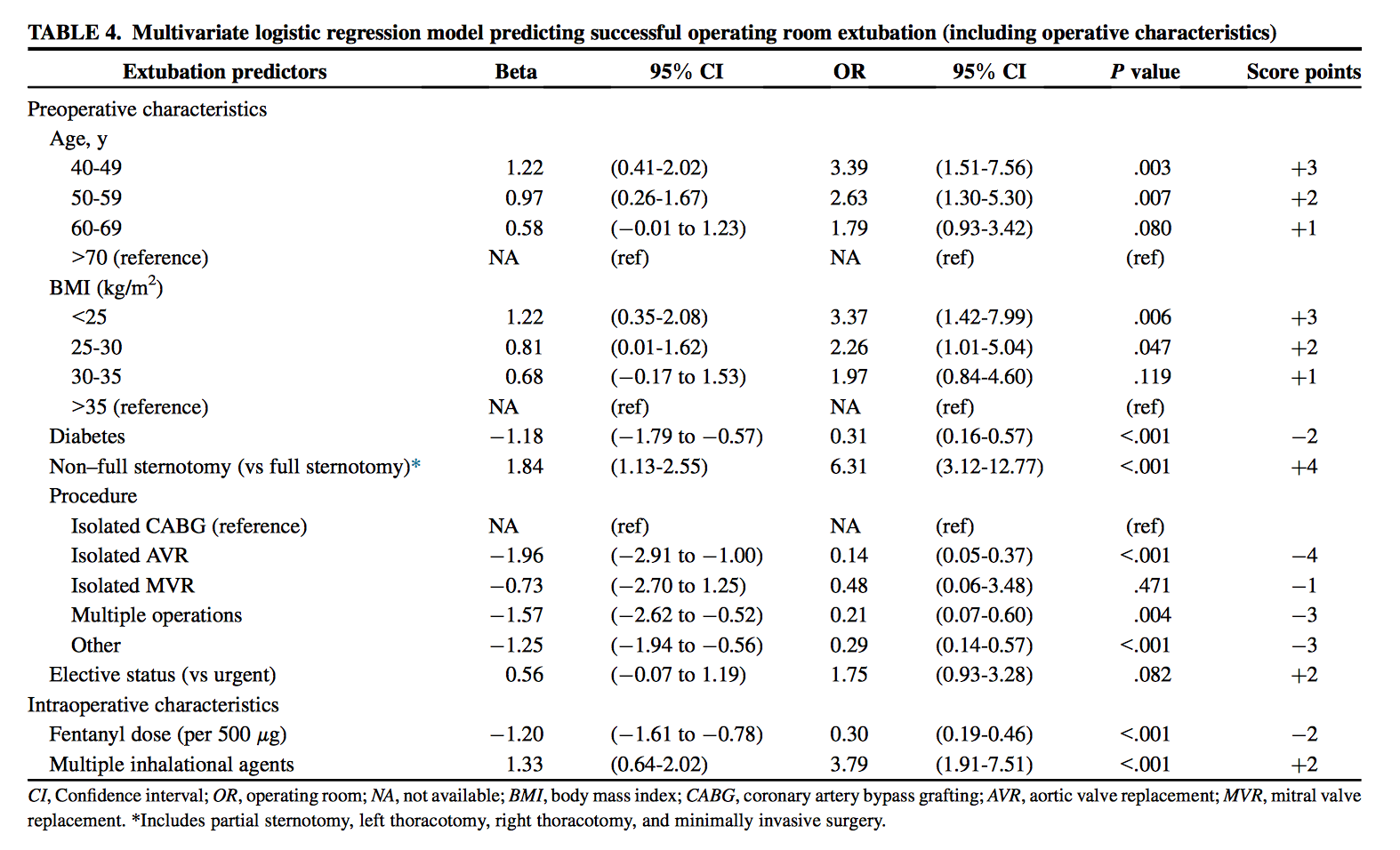
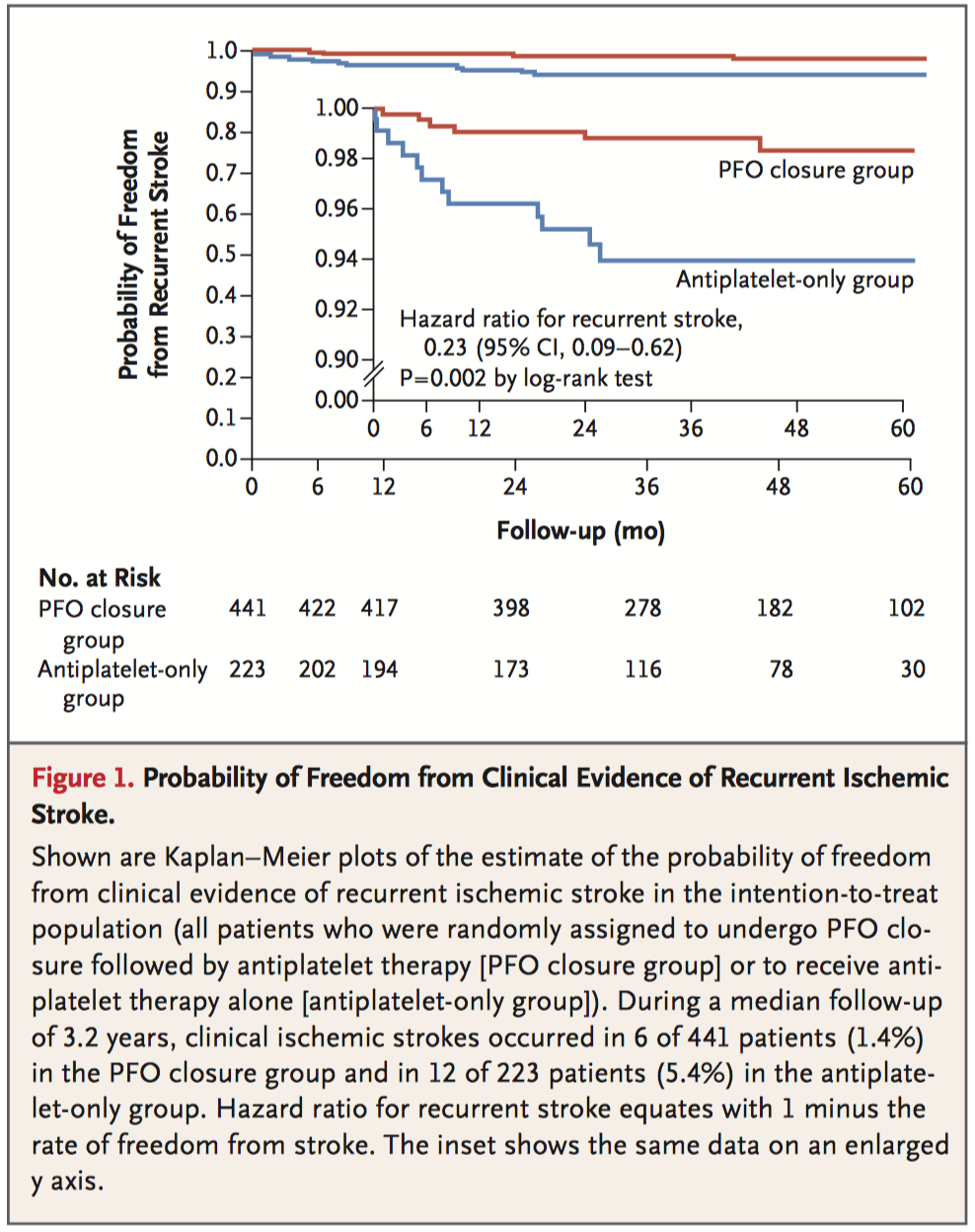
Part of a three article series and editorial on patent foramen ovale (PFO), this multi-national, blinded randomised controlled trial assigned patients to either PFO closure with antiplatet therapy (n=441) or to antiplatet therapy alone (n=223) and monitored clinical outcomes over a median follow-up of 3.2 years. Both clinical ischemic stroke and incidence of new brain infarctions on imaging were more common in the antiplatelet-only group (5.4% vs. 1.4%, respectively, P = 0.002; and 11.3% vs. 5.7%, respectively, P = 0.04). However, the PFO closure group did experience a number of device-related complications (n=6, 1.4%) and a higher incidence of atrial fibrillation or flutter (6.6% vs. 0.4%, P<0.001).
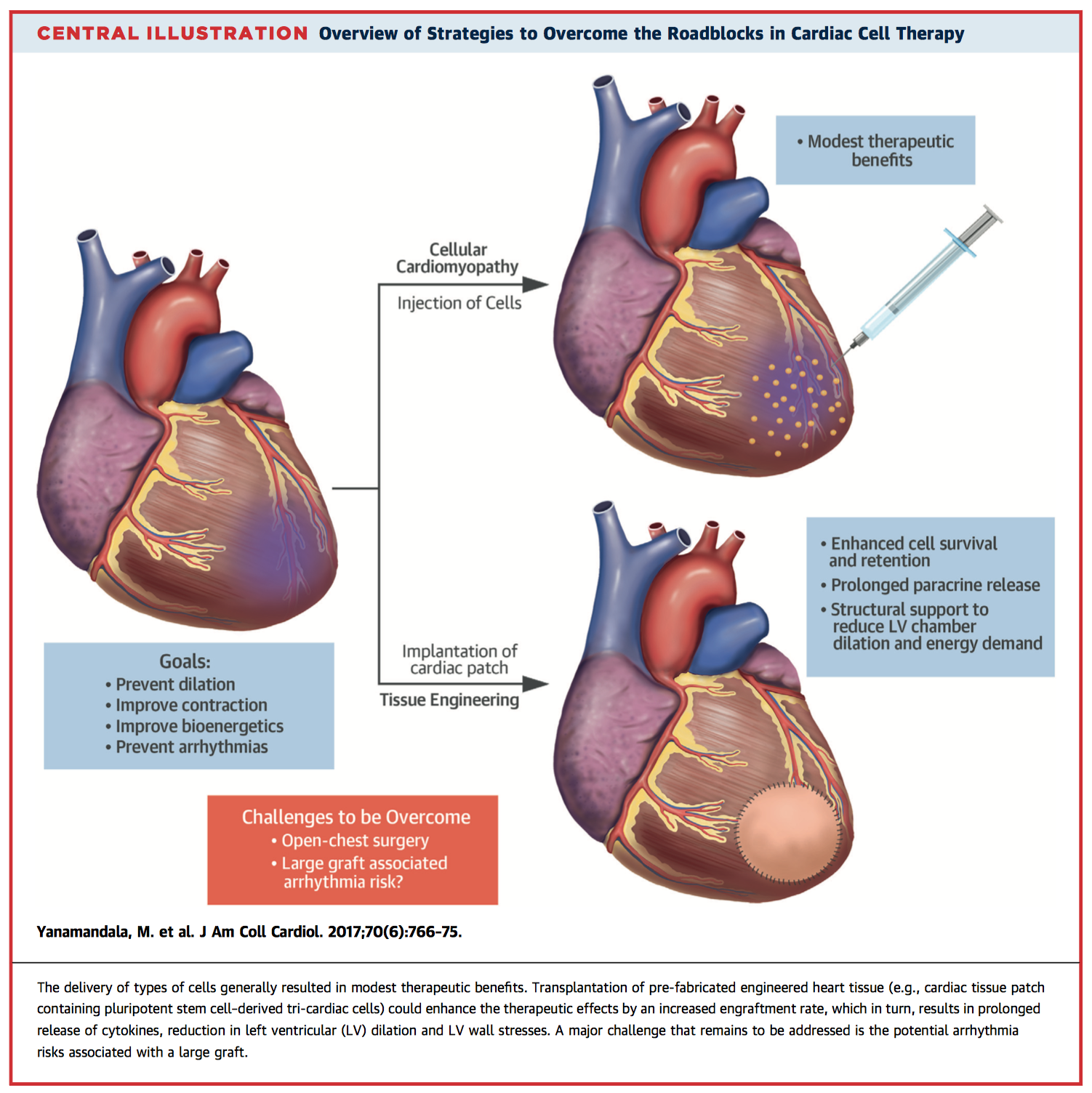
Cardiac cell therapies have shown promise in animal trials but progress in clinical trials has been modest. Current techniques include intramyocardial injection with various progenitor cells or transplantation of bioengineered tissue patches, however challenges remain including poor cell engraftment rates and increased arrythmogenic risk secondary to poor electrical integration. This article presents and dissects the current status, advances and potential directions in cardiac cell therapies, as discussed at the 2016 Progenitor Cell Biology Consortium and Cardiovascular Tissue Engineering Symposium.
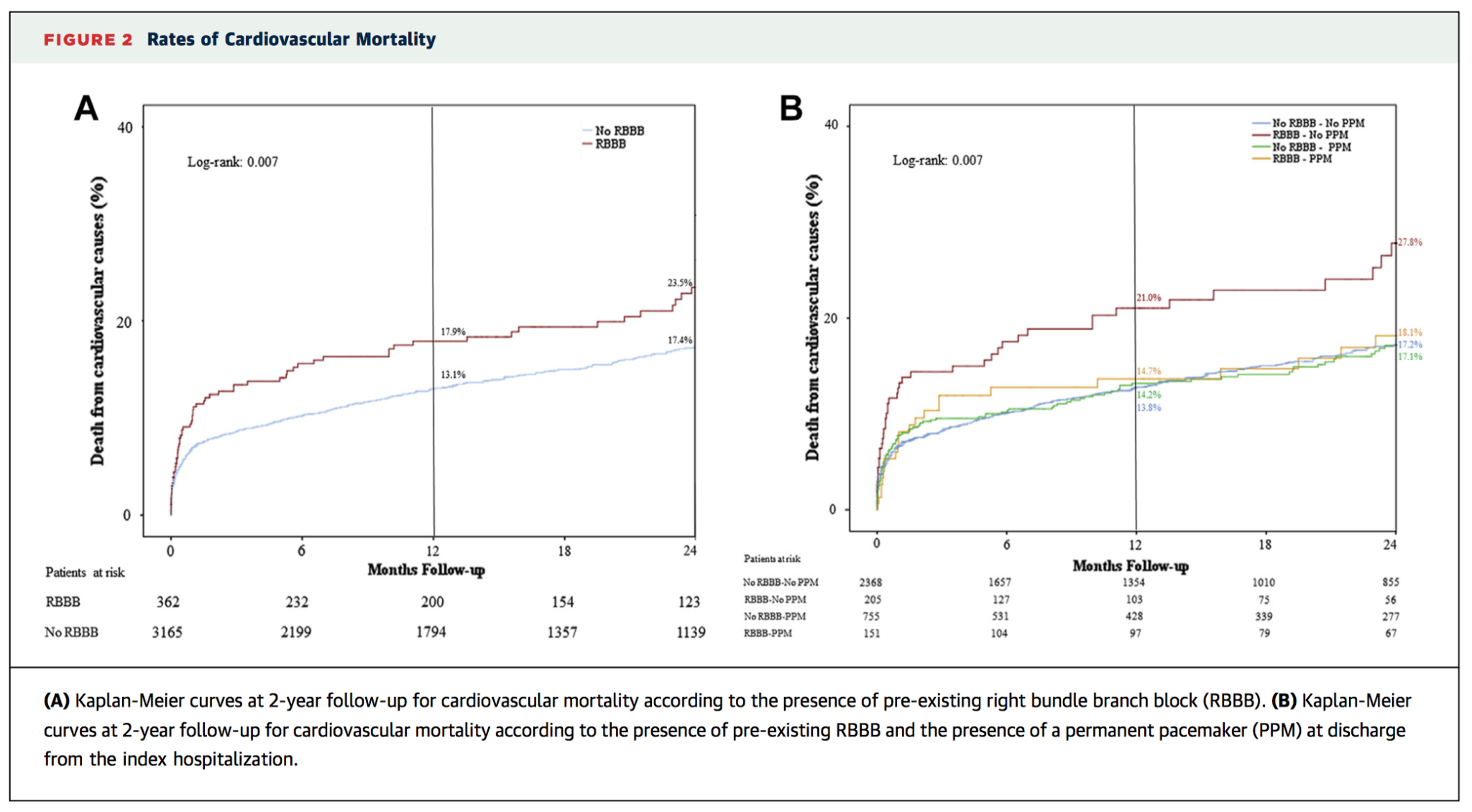
This multi-centre cohort study examined the prevalence and impact of pre-existing right bundle branch block (RBBB) in 3527 patients undergoing transcatheter aortic valve replacement (TAVR). The overall incidence of pre-existing RBBB was 10.3% (n=362). This was associated with worse short-term outcomes including higher rates of permanent pacemaker implantation (PPI) ( 40.1% vs. 13.5%; p < 0.001) and 30 day death (10.2% vs. 6.9%; p = 0.024). RBBB was also associated with worse mid-term outcomes (average follow-up 20±18 months) including cardiovascular mortality and all-cause mortality, but not sudden cardiac death (SCD). However, a sub-analysis revealed patients discharged without PPI insertion had especially high risk of SCD (hazard ratio 2.68, P = 0.023). The authors suggest future studies should examine early detection strategies and the potential role of prophylactic PPI.
Cardiac Surgery
Summarised by Andrew Haymet
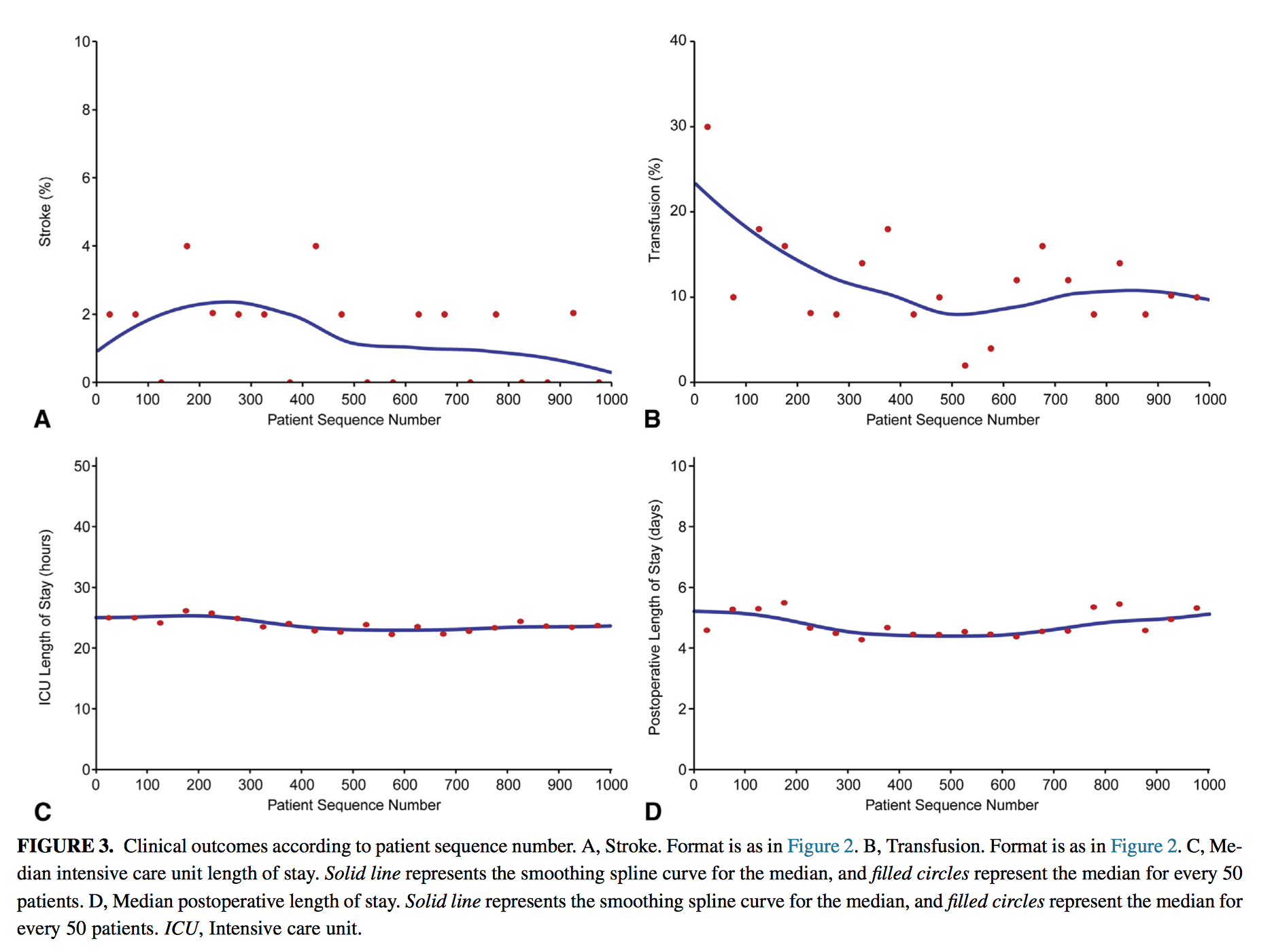
This study aimed to assess the technical improvement and clinical outcomes of the first 1000 cases of robotic primary mitral valve surgery performed in a tertiary care centre from January 2006 to November 2013. A total of 992 patients (99.5%) underwent mitral valve repair whilst 5 (0.5%) underwent valve replacement. Intraoperative post repair echocardiography showed that 989/992 (99.7%) left theatre with no or mild regurgitation. In-hospital mortality and stroke was 1 (0.1%) and 14 (1.4%) respectively. The authors concluded that robotically assisted mitral valve surgery provides successful, effective, and safe mitral valve repair, particularly in patients with leaflet prolapse.
Webcast of this AATS meeting presentation:
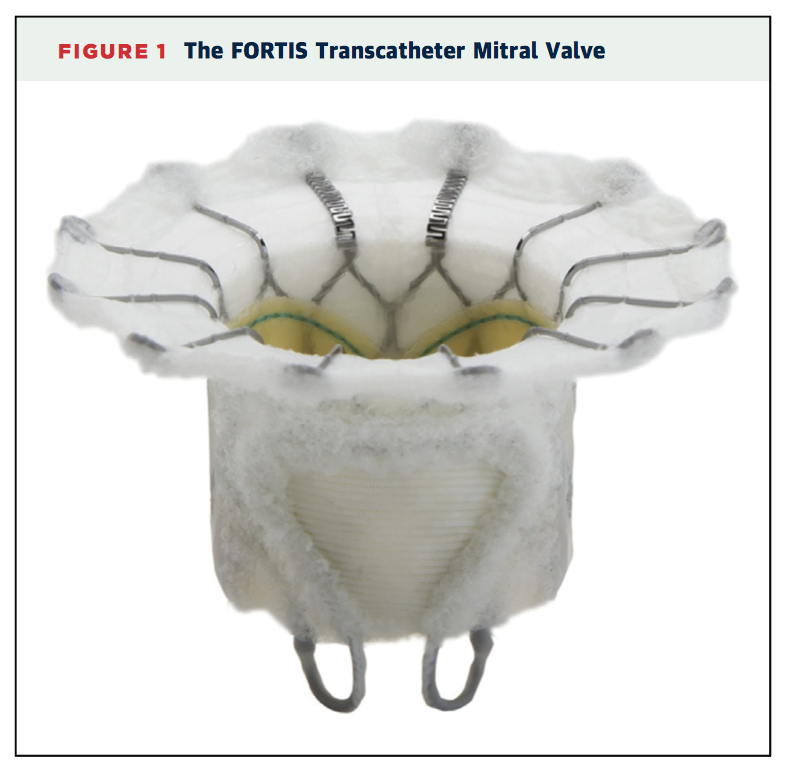
This multicentre registry of 13 patients reported the two year outcomes of transcatheter mitral valve replacement (TMVR) with the Fortis valve (Edwards Lifesciences, Irvine, California). Technical success was achieved in 10 patients (76.9%), and 5 patients (38.5%) died within 30 days postoperatively. At 30-day follow up, mean transmitral gradient was 3 +/- 1mmHg. There were no cases of moderate-severe residual mitral regurgitation or left ventricular outflow tract obstruction. Two further deaths occurred during follow-up as a result of end stage heart failure. At two year follow-up, all cause mortality was 54%. The authors concluded that TMVR was feasible with the FORTIS valve, with MR reduction maintained at two years and no late device-related adverse events.
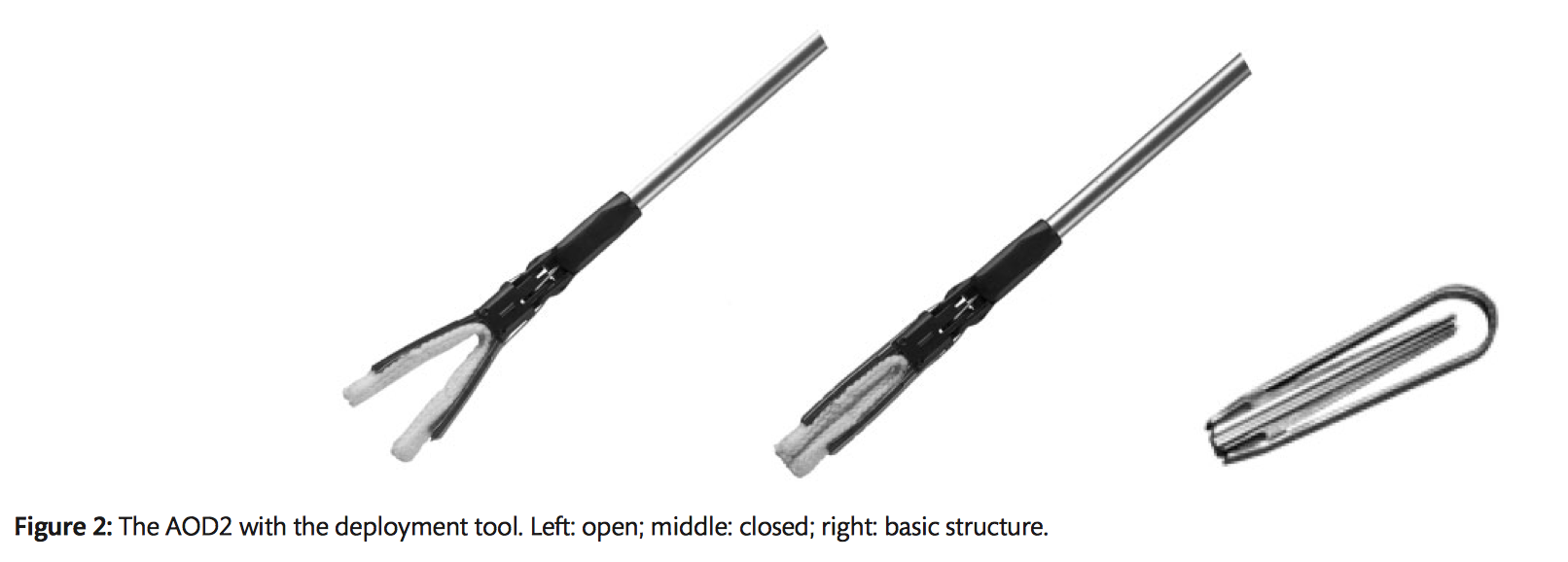
Exclusion of the left atrial appendage (LAA) has been proposed to reduce the risk of stroke in patients with atrial fibrillation. This study evaluated the feasibility and efficacy of the AtriClip PRO-V device (AOD2), currently in development, for LAA exclusion in a canine model. Six dogs were implanted via thoracotomy with the clinically available AtriClip device (AOD1) on the right atrial appendage and the AOD2 on the left. Ease of use of AOD1 and AOD2 was deemed comparable. All animals survived 90 days with no complications. The atrial appendages were successfully occluded without device migration. There was an acceptable biocompatibility response on histology of all AtriClip devices. The authors concluded that once approved for clinical application, the AOD2 could provide a new therapeutic option to lower the risks of stroke in patients with atrial fibrillation.
Cardiac Imaging
Summarised by Sarah Catchpoole
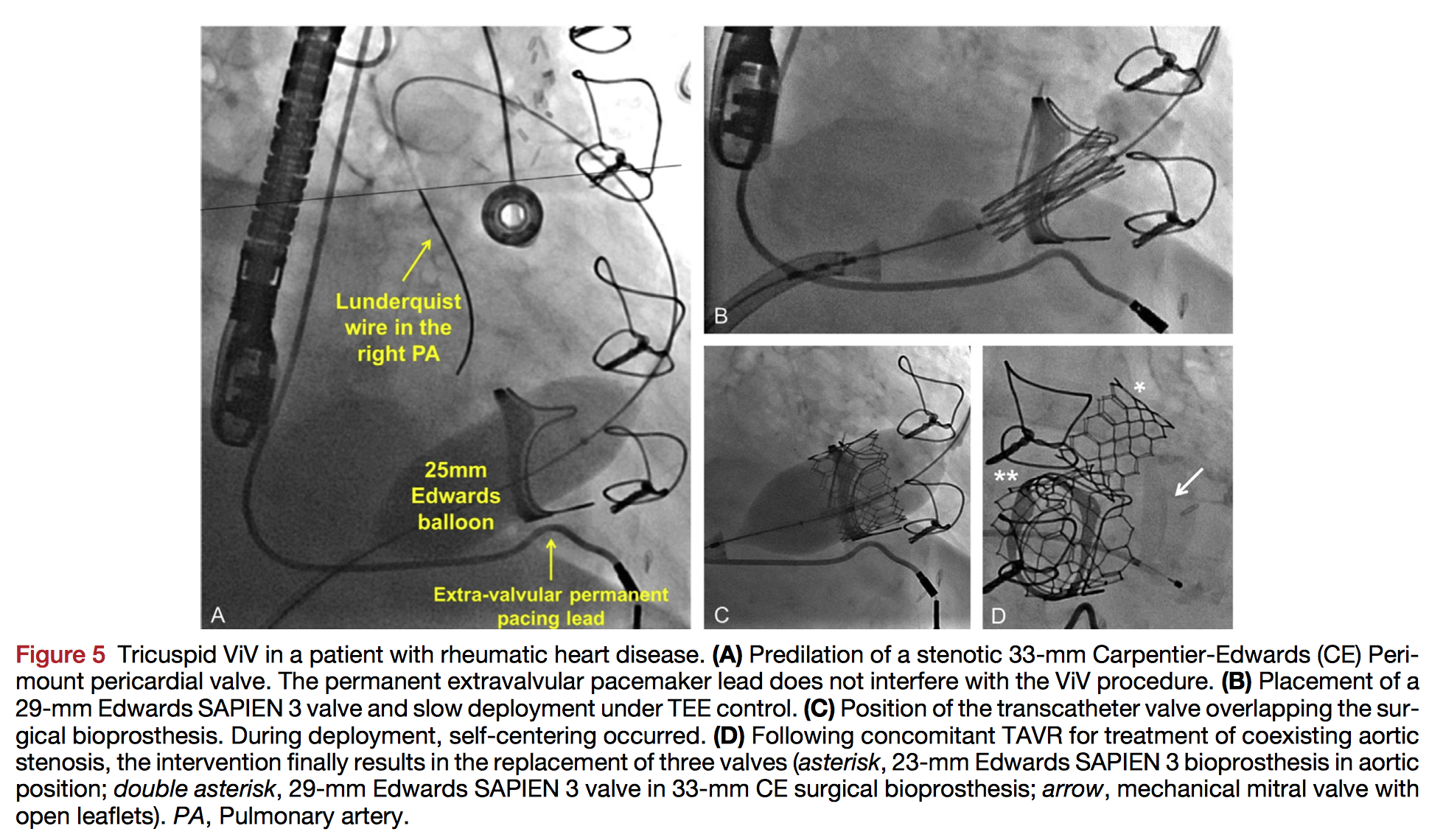
The high-risk associated with repeat surgical tricuspid valve replacement has led to growing interest in the transcatheter tricuspid valve-in-valve approach for a failing prosthesis. This comprehensive review highlights the role of echocardiographic assessment in the initial assessment of tricuspid prosthetic dysfunction and as a guide for peri-procedural intervention. Finally, while normal ranges for post-procedural follow-up are yet to be established, the article provides expert recommendations derived from clinical case-report experience and the tricuspid VIVID registry.
The aortic valve (AV) is being increasingly appreciated as a 3D dynamic structure which we must understand with greater precision to optimise AV repair. This retrospective clinical feasibility study examined what dynamic assessment is possible with commercially available software (Siemens eSie valve) in patients with normal aortic valves undergoing 3D transoesophageal echocardiography as part of other cardiac surgery. Multiple parameters including sizes for the annulus, sinus of Valsalva, sinotubular junction, aortic leaflet height, and leaflet coaptation were found to change significantly during the cardiac cycle (p < 0.001, for all). The authors conclude dynamic imaging is feasible and may improve intra-operative decision making.
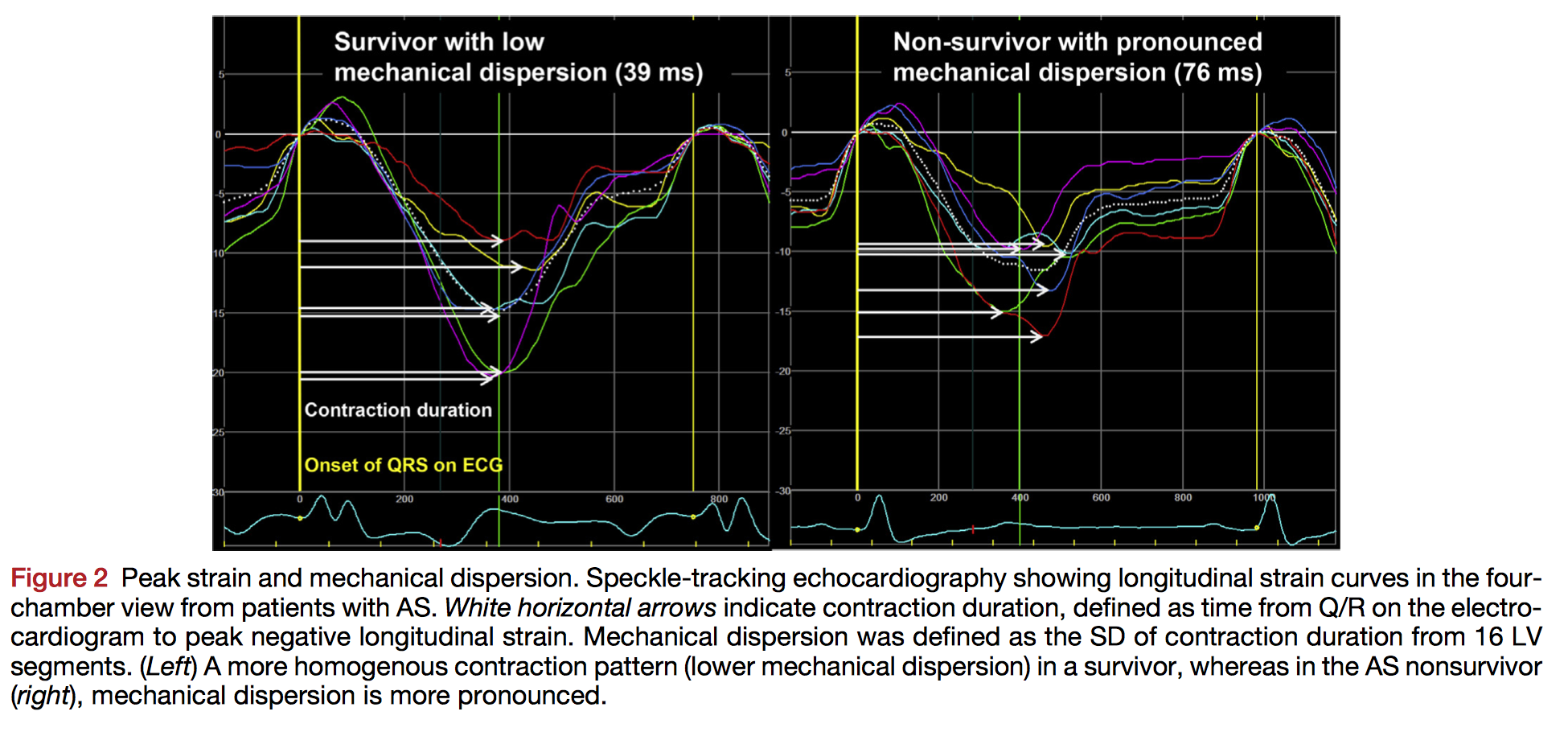
Early detection of decompensation in aortic stenosis (AS) can guide clinical decision making regarding optimal timing of valve replacement. In this prospective cohort of 162 patients with AS, the authors examined the prognostic value of global longitudinal strain (GLS) and mechanical dispersion (standard deviation of time from Q/R on the electrocardiogram to peak strain in 16 left ventricular segments) over a period of 37±13 months. Poorer GLS and mechanical dispersion were both associated with lower overall survival. However, only mechanical dispersion provided incremental prognostic utility in addition to GLS, left ventricular ejection fraction, and correlates of flow and gradient. The authors suggest mechanical dispersion is a useful prognostic marker and may represent a measure of myocardial fibrosis.
Perioperative Medicine
Summarised by Andrew Haymet
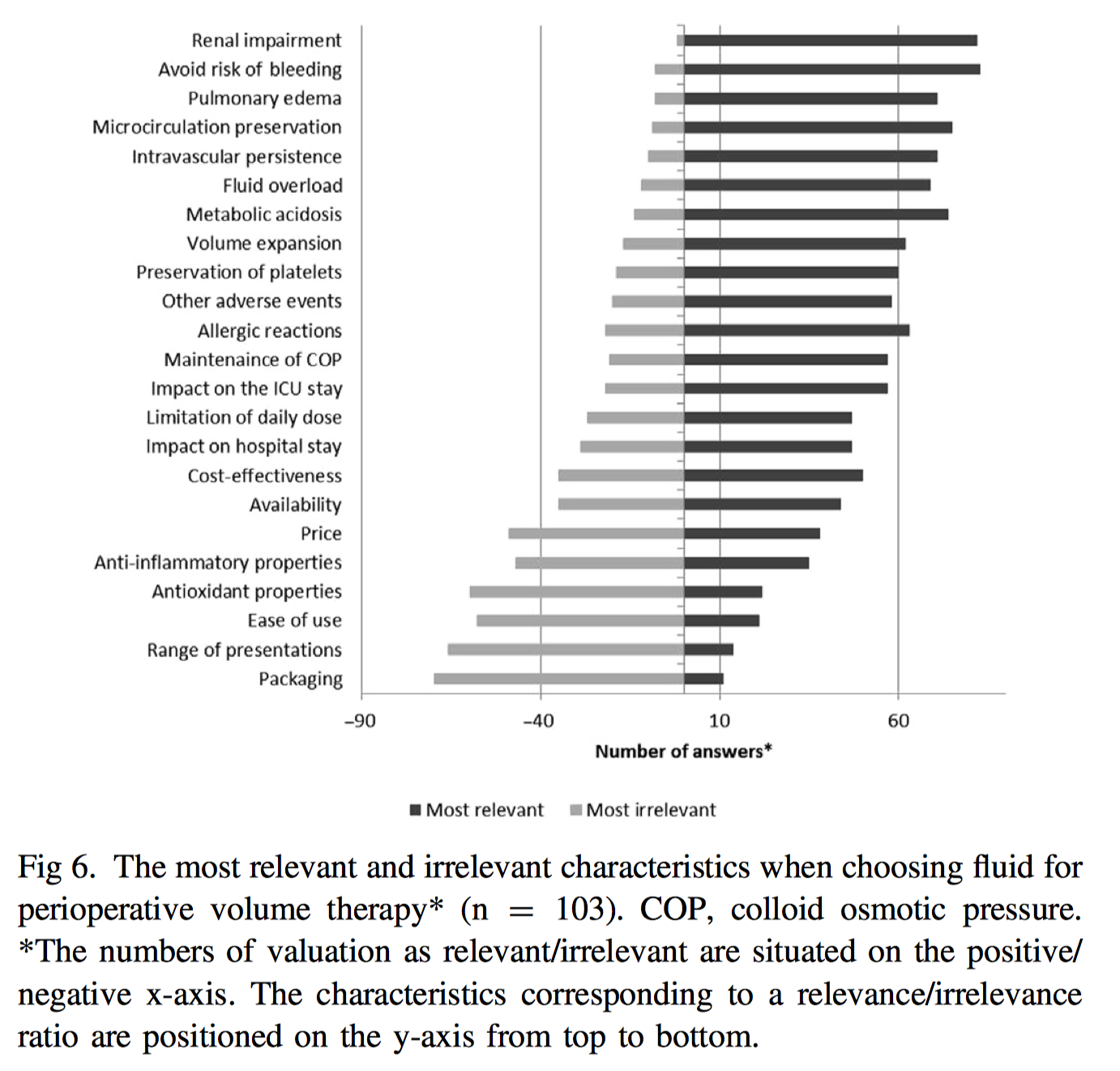
This study surveyed 106 respondents primarily from teaching hospitals across 18 European countries to evaluate current perioperative fluid management in cardiac surgery patients. Perfusionists were responsible for cardiopulmonary bypass (CPB) priming solutions, whilst anaesthetists were responsible for intraoperative and postoperative fluid management. For CPB bypass priming, balanced crystalloids were used in 51.5% of centres, and 36% using a combination of crystalloid with either synthetic colloid or albumin. Intraoperatively, balanced crystalloids were used by 74% of centres. No colloids were used by 32% of respondents. 73% of respondents, also involved in ICU management, did not change their fluid regimen in the ICU compared with intraoperatively. The authors concluded that perioperative fluid management may have evolved across the last few years in European centres, with balanced crystalloids appearing to be the preferred solutions, followed by synthetic colloids (mainly gelatins), and albumin.
Transcatheter aortic valve replacement (TAVR) confers unavoidable haemodynamic perturbances which may contribute to adverse neurological outcomes associated with the procedure. This paper monitored cerebral oximetry in 31 patients undergoing transfemoral TAVR to detect intraoperative hypoperfusion insults. Serial neurologic, cognitive, and cerebral MRI assessments were used to quantify perioperative neurologic injury. Cerebral oximetry reacted rapidly to rapid ventricular pacing, with significant cerebral desaturation relative to baseline of greater than 12% and 20% in 12 of 31 (68%) and 9 of 31 (29%) patients respectively. Postoperative cognitive dysfunction was evident in 3 of 31 (10%) patients and new MRI-defined ischaemic lesions were seen in 17 of 28 (61%) patients. No patient experienced clinically apparent stroke. The authors concluded that whilst cerebral oximetry reacted promptly to rapid ventricular pacing, with significant desaturation and hyperaemia a common occurrence, this did not appear to be associated with objective neurologic injury postoperatively.
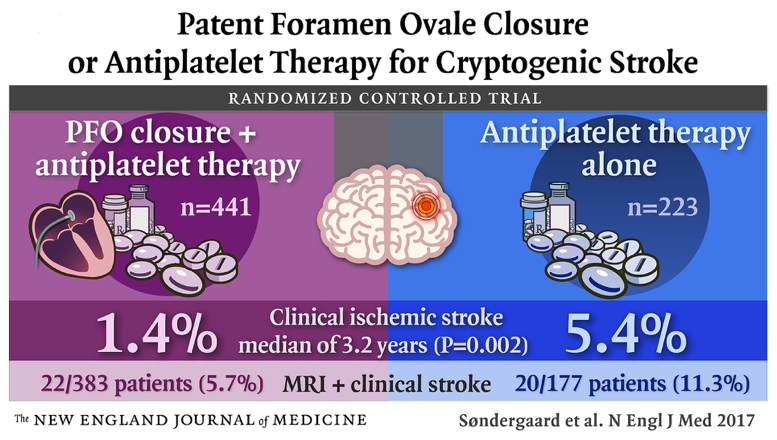
This retrospective cohort study of 1518 patients undergoing cardiac surgery aimed to identify perioperative factors associated with successful immediate extubation in the operating room after adult cardiac surgery. All patients underwent a standardized fast-track cardiac anaesthetic protocol. A predictive score of successful extubation was constructed from the multivariable logistic regression results of 800 patients, and further tested with a validation set of 398 patients. Factors independently associated with higher probability of successful operating room extubation were younger age, lower body mass index, absence of chronic lung disease and diabetes, elective surgery, and lower doses of intraoperative fentanyl. Patient scores less than 0 had a minimal probability of successful operating room extubation, whilst scores greater than 5 were highly predictive of a successful extubation.