Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been recently published in each speciality (Cardiology, Cardiac Surgery, Cardiac Imaging, Perioperative Medicine).
Cardiology
Summarised by Sarah Catchpoole
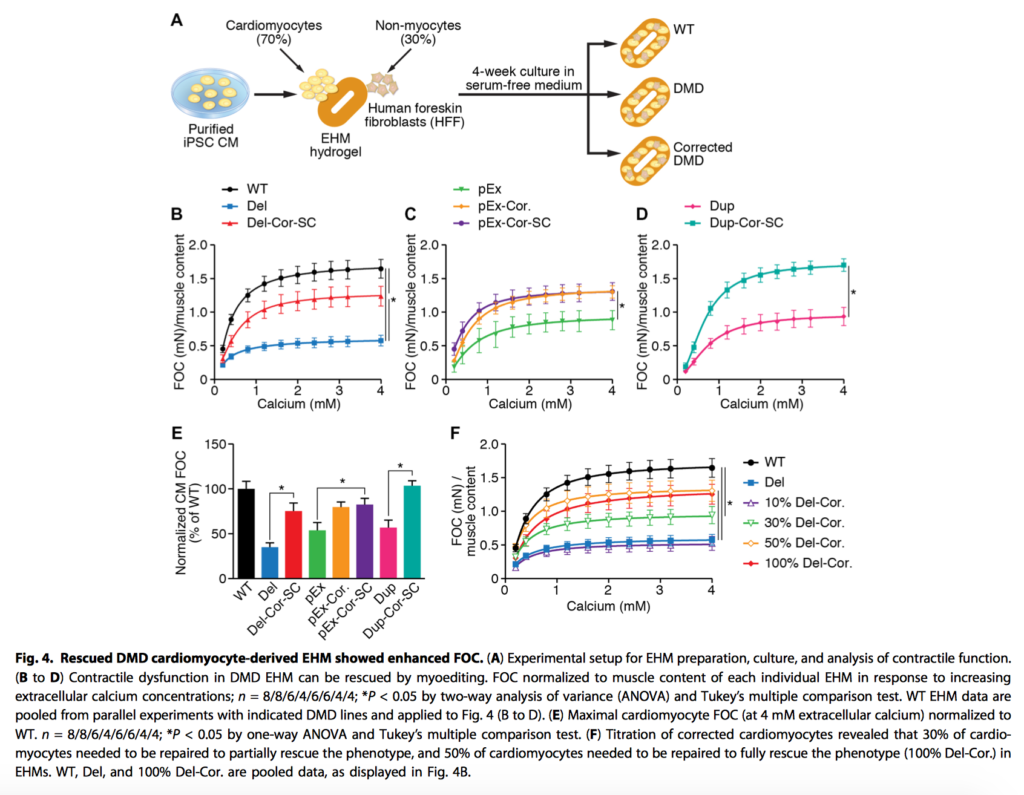
Duchenne muscular dystrophy (DMD) is an ultimately fatal degenerative muscular genetic disorder, with complications including dilated cardiomyopathy. CRISPR/Cas9 has been successfully applied to correct mutations to the dystrophin gene via a process the authors term myoediting. In contrast to previous genetic research in DMD, whereby large regions were deleted in order to correct dystrophin, the authors identified key RNA guide sites to allow the 12 most common DMD associated exons to be skipped. In human engineered heart muscle, the edited cardiomyocytes demonstrated restored dystrophin and contractile function. As these 12 exons are responsible for approximately 60% of DMD, the authors conclude the results are promising for future human trails.
Lund LH, et al. The year in cardiology 2017: heart failure. European Heart Journal. 2018 Jan 2.
This end of year research summary from the European Heart Journal highlights key clinical trials from autumn 2016-2017, and their implications in the clinical landscape of heart failure (HF). Findings and recommendations are arranged by categories; firstly regarding existing therapies by grade of HF, then covering acute heart failure, advanced heart failure, management of comorbidities, and lastly novel interventions. The authors note major challenges in HF at present are improved implementation of guideline directed care, and the need for effective interventions in HF with preserved ejection fraction and advanced HF.
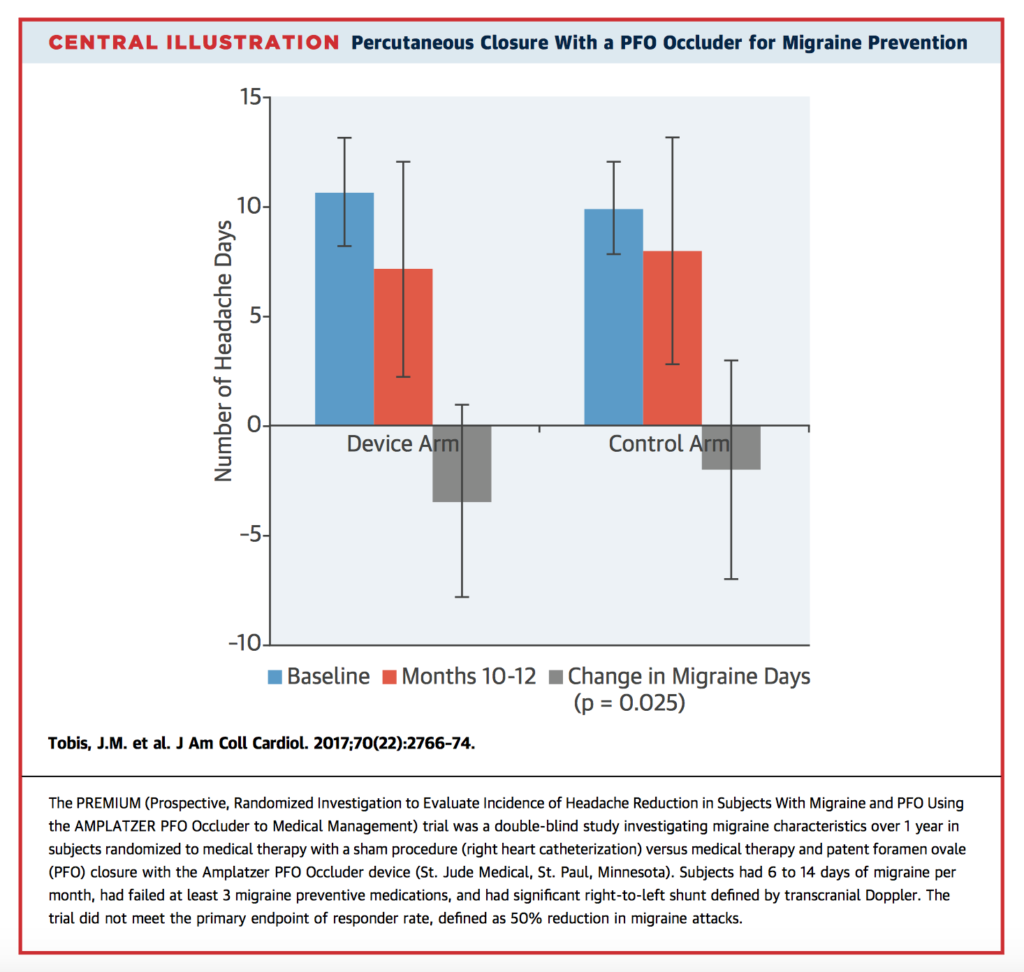
Migraine has previously been associated with patent foramen ovale (PFO) and other causes of right to left shunt. In this double-blind randomised trial, 230 patients with PFO and treatment-resistant migraine (failure of ≥3 preventative medications) received either PFO closure, or a sham procedure (right heart catheterisation). While the primary endpoint of responder rate (50% or greater reduction in migraine attacks compared with sham control) was not met, complete migraine remission at 1 year was observed in 10 of patients (8.5%) in the PFO closure group vs. 1 patient in the control group (p=0.01). Post-hoc analyses did reveal a significant difference in responder rate for patients who had migraine with aura (49% vs. 23%, p=0.015). Given migraine is a heterogenous disorder, the authors suggest that PFO closure merits further evaluation for this subgroup.
Cardiac Surgery
Summarised by Andrew Haymet
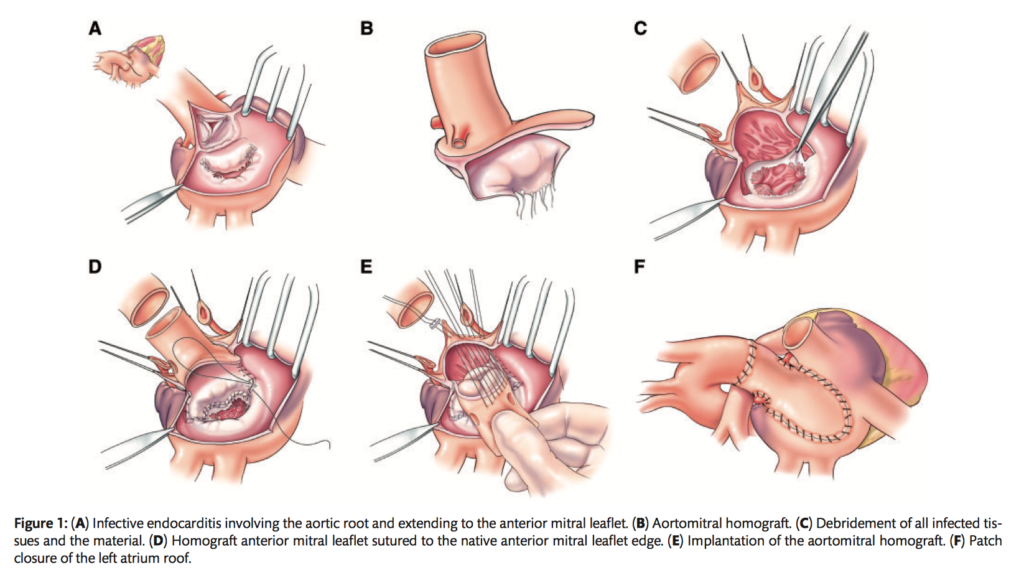
Surgical management of invasive double-valve infective endocarditis involving the intervalvular fibrosa (IVF) requires extensive, challenging debridement with complex reconstruction. Between 2010 and 2017, 37 patients with IE involving the IVF underwent the hemi-Commando procedure and aortic root replacement with reconstruction of IVF using an aortomitral allograft. Preoperatively, 70% (n = 26) of patients were admitted to the intensive care unit and 11% (n = 4) of patients were in septic shock. Hospital death occurred in 8% of patients due to multisystem organ failure (n=3). Intact IVF reconstruction was confirmed in all patients with no abnormal communication between the left heart chambers. One-year survival was 91%, while 3-year survival was 82%. Mid-term follow up revealed 1 death secondary to recurrent IE. The authors concluded that compared to double-valve replacement with IVF reconstruction, the early and midterm outcomes of the hemi-Commando procedure proved to be a feasible treatment option for IVF reconstruction.
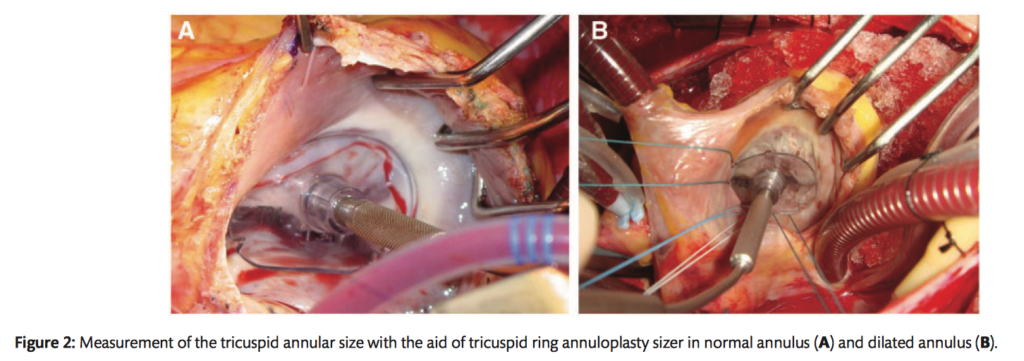
The benefits of concomitant tricuspid annuloplasty (TAP) for non-significant functional tricuspid regurgitation (TR) during mitral valve replacement (MVR) are controversial. Between 2004 and 2014, out of an enrolled 256 patients (56.4 +/- 12.1 years), 82 underwent concomitant TR annuloplasty (TAP group) and 174 patients did not undergo the procedure (nTAP group). The early clinical outcomes were similar between the 2 groups before and after propensity score matching with an early mortality rate of 3.5% (9 of 256). No significant differences in overall survival between the two groups were observed. However, freedom from significant TR aggravation and from TV related events was significantly higher in the TAP group (P=0.047 and P=0.043 respectively). The authors concluded that TV ring annuloplasty can be performed without complications and can be beneficial for patients with trivial or mild functional TR who are undergoing MVR.
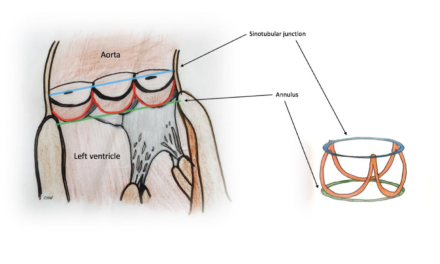
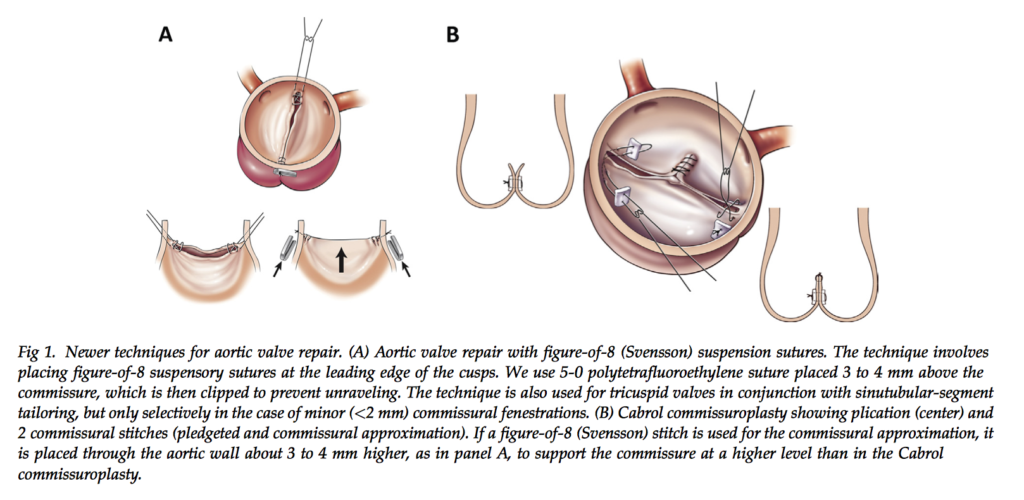
This study investigated the value of aortic valve repair rather than replacement in 1,124 patients between 2001 and 2011. Techniques involved commissural figure-of-8 suspension sutures (n = 63 [6.2%]), cusp repair with commissuroplasty (n = 481 [48%]), debridement (n = 174 [17%]), free-margin plication (n = 271 [27%]) or resection (n = 75) or both, or annulus repair with resuspension (n = 230 [23%]), root reimplantation (n [ 252 [25%]), or remodeling (n = 35 [3.5%]). Planned repair was aborted for replacement in 115 patients (10%). In-hospital outcomes for the remaining 1,009 patients included death (12 [1.2%]), stroke (13 [1.3%]), and reoperation for valve dysfunction (14 [1.4%]). Freedom from aortic valve reoperation at 1, 5, and 10 years was 97%, 93%, and 90%, respectively. Survival at 1, 5, and 10 years was 96%, 92%, and 83%. The authors concluded that valve repair, particularly commissural figure-of-8 suspension sutures and repair with annular support, is effective and durable for treating aortic valve dysfunction.
Cardiac Imaging
Summarised by Sarah Catchpoole
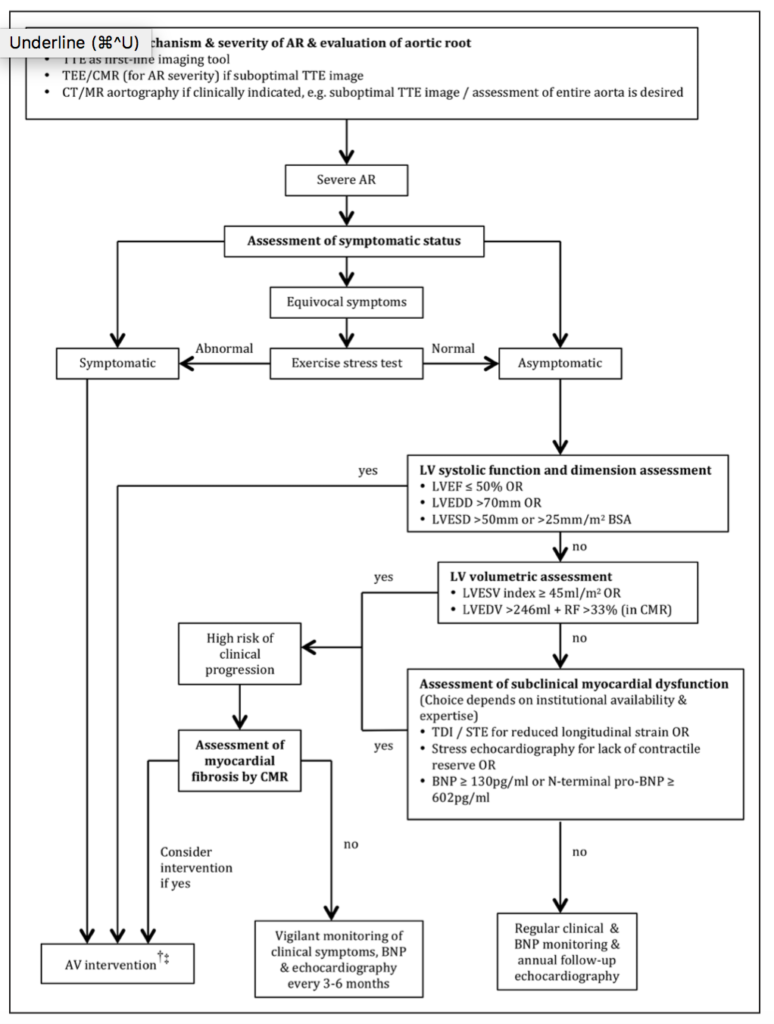
Effective and timely intervention in aortic regurgitation (AR) will become increasingly important as the population ages, with the prevalence and burden of AR set to rise. The natural history of AR is one of a prolonged compensated, asymptomatic period; however, recent data have shown irreversible myocardial damage occurs before development of current surgical indications. This in-depth review assesses the current methods for evaluating subclinical myocardial dysfunction in asymptomatic patients and accordingly, the optimal timing for any surgical intervention. Two clinical algorithms are proposed for (1) transthoracic echocardiography AR evaluation and stratification, and (2) clinical management including multimodal assessment, follow up intervals and referral to surgery.
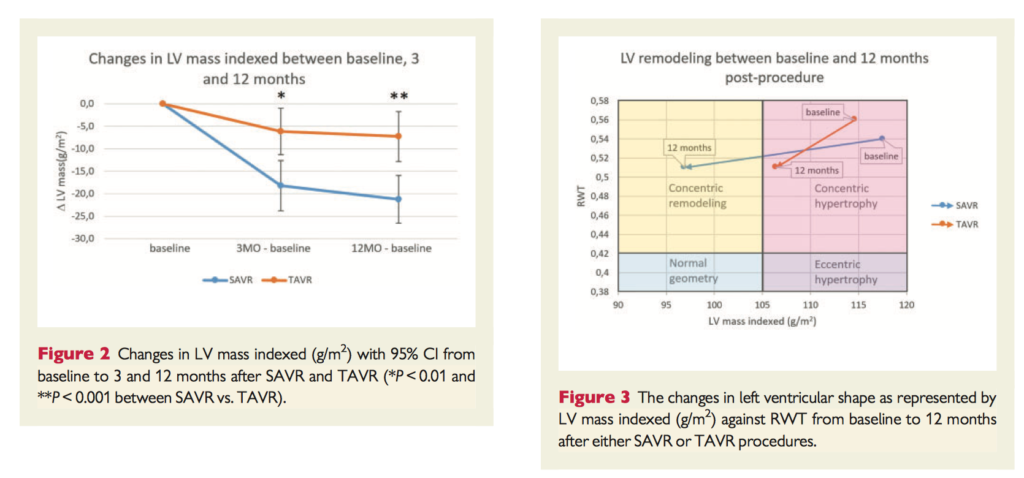
Transcatheter aortic valve replacement (TAVR) is becoming increasingly available for high and intermediate risk patients. Compared to surgical aortic valve replacement (SAVR), TAVR is associated with larger aortic valve area, increased paravalvular leakage, and increased rate of conduction abnormalities. To compare long-term haemodynamics, a subset of patients (n=232) from the NOTION trial were assessed using transthoracic echocardiography at baseline, 3 months and 12 months after valve replacement. SAVR recipients had improved left ventricular mass regression (17.5% vs. 7.2%, p<0.001) and improved end diastolic volume (15.4± 2.6ml decrease, vs. 10.2±2.5ml increase for TAVR recipients, p<0.0001). The difference in end diastolic volume was associated with the observed increase in pacemaker implantation and paravalvular leakage in the TAVR group (p<0.01); therefore, optimisation of long-term TAVR outcomes will need to address these disparities.
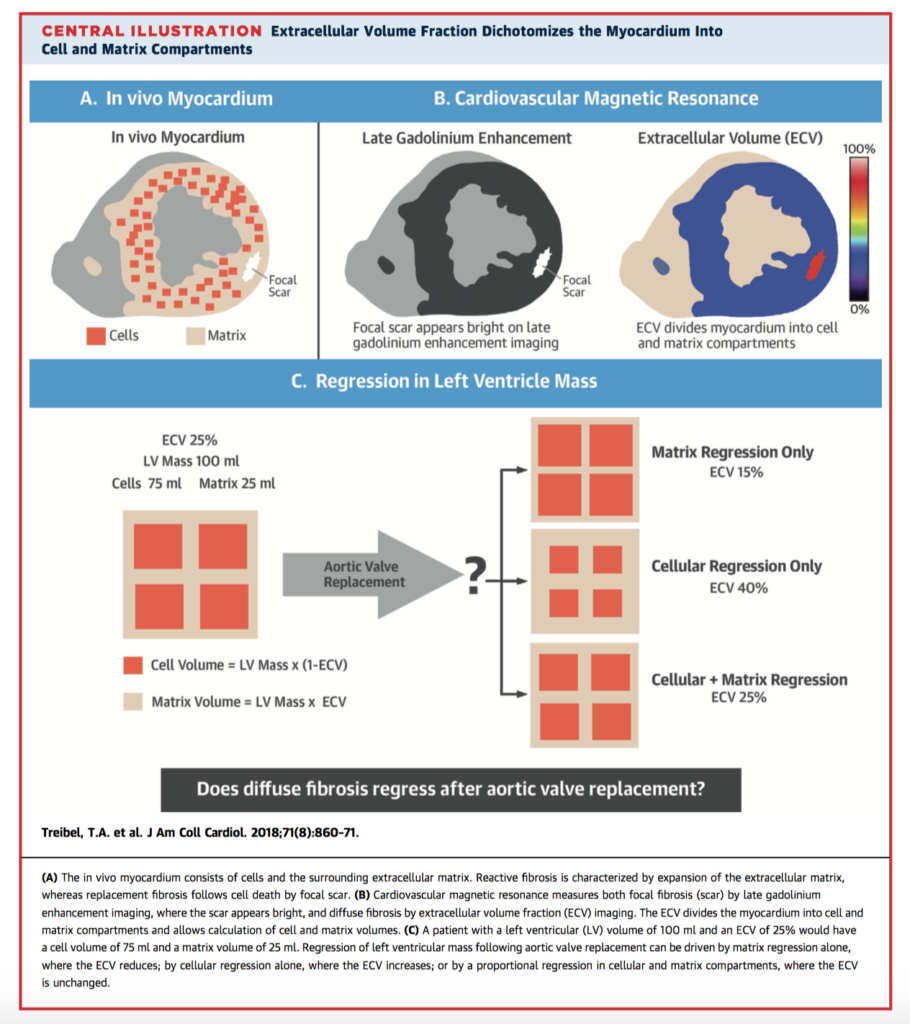
Can left ventricular (LV) hypertrophy caused by aortis stenosis (AS) resolve after aortic valve replacement (AVR)? In this prospective cohort study, 181 patients with severe symptomatic AS were assessed pre and at one year post AVR. In the 116 pace-maker free survivors evaluated, there was a 19% reduction in LV mass (p< 0.001), small increase in LV ejection fraction (71±16% to 74±12%, p<0.006), as well as improved NT-proBNP levels (50 ng/l to 38 ng/l, p < 0.001), 6 minute walk test, and New York Heart Association functional class. On cardiac magnetic resonance imaging, there was regression of diffuse fibrosis and myocardial cellular hypertrophy (increased extracellular volume fraction, 28.2±2.9% to 29.9±4.0%; p<0.001). However, there was no change in focal fibrosis, confirming cardiomyocyte loss is likely irreversible. The study also validates CMR to non-invasively assess improvements in cellular hypertrophy and diffuse fibrosis, which may represent a future therapeutic target.
Perioperative Medicine
Summarised by Andrew Haymet
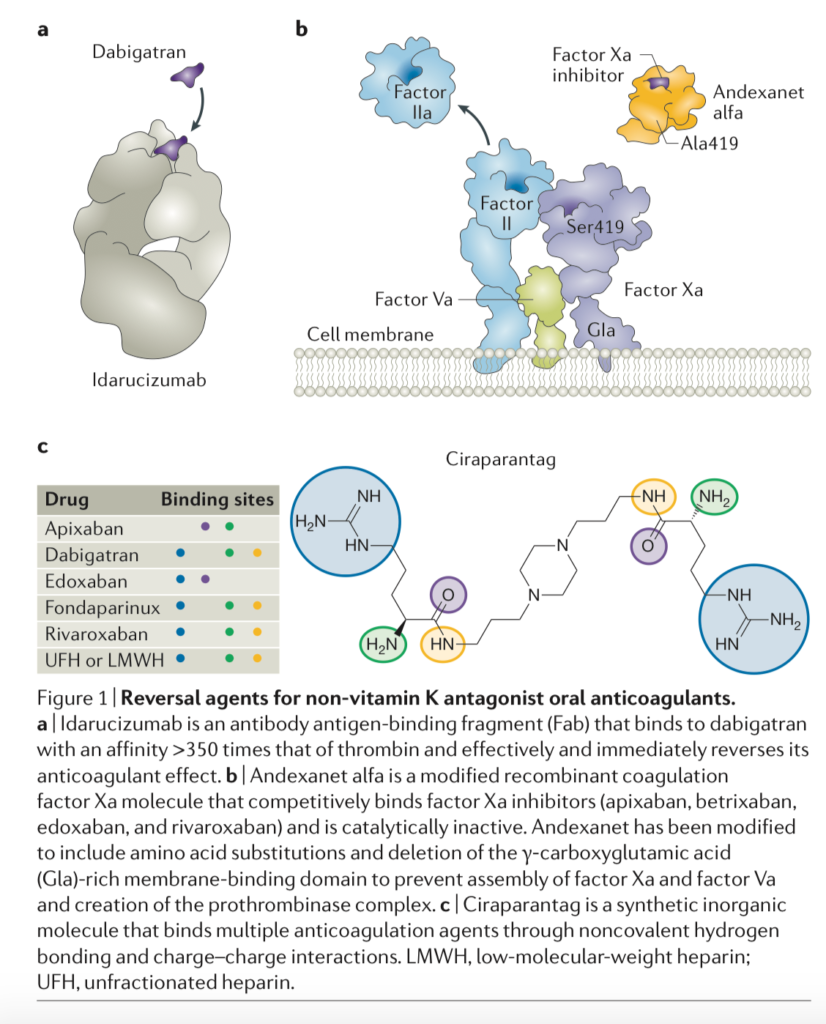
The non-vitamin K antagonist oral anticoagulants (NOACs) include dabigatran, which inhibits thrombin, and apixaban, betrixaban, edoxaban, and rivaroxaban, which inhibit coagulation factor Xa. Although clinical studies of NOACs were conducted without antidotes, patient outcomes with major bleeding when receiving NOACs were no worse than those in patients treated with a vitamin K antagonist. Three NOAC reversal agents are in various stages of development: idarucizumab, a specific reversal agent for dabigatran; andexanet alfa, which reverses factor Xa inhibitors; and ciraparantag, which is purported to reverse all NOACs. . Idarucizumab enables rapid and sustained reversal of dabigatran, and andexanet is poised to do the same for oral factor Xa inhibitors. Until andexanet is available, however, PCC might be of use. Specific reversal agents are expensive, and anticoagulant reversal places patients at risk of thrombosis. Therefore, reversal should be reserved for patients in need, and anticoagulation therapy should be restarted promptly after patients have stabilized.
This prospective clinical trial based at a tertiary level cardiac surgical intensive care unit aimed to study the effect of implementing an early extubation protocol in 459 patients following cardiac surgery. Primary outcomes were intensive care unit (ICU) and hospital length of stay. With implementation of the protocol, median ventilation times decreased from 7.4 hours (interquartile range = 6.72 hours) to 5.73 hours (IQR = 5.51 hours, p = 0.0001). However, median ICU length of stay in patients who achieved extubation within 6 hours increased to 49.45 hours (IQR = 44.4) from 40.3 (IQR = 25.6) (p = 0.0017). The authors concluded that decreasing intubation times to <6 hours in postoperative cardiac surgery patients was possible with a multidisciplinary rapid weaning protocol, however patients extubated within 6 hours had longer ICU stays and no difference to hospital length of stay with this intervention.
This single center, retrospective analysis of 81 patients aimed to analyze the results of open heart surgery and bleeding complications after administration of novel oral anticoagulants (NOAC). Of the 81 patients operated on between June 2014 and June 2016, 37 had Rivaroxaban (45.7%), 35 Apixaban (43.2%), and 9 Dabigatran (11.1%). Surgery was performed at a median of 4 [IQR 3, 6] days after NOAC withdrawal. Thirty-day-mortality was 3.7%. Reduced renal function was predictive for length of intensive care unit (ICU) stay and administration of red blood cells (p<0.0001 and p=0.0291, respectively). The NOAC withdrawal interval significantly influenced postoperative drainage volume (p=0.0056). Five patients needed re-thoracotomy because of relevant bleeding (6.2%), 4 after Apixaban (11.4%) and 1 after Rivaroxaban therapy (2.7%). ICU stay was 2.0 days after NOAC withdrawal of 10 days, compared to 4.2 days without termination. The authors concluded that a long NOAC withdrawal period was essential for safe open heart surgery, particularly in patients with impaired renal function. Despite official recommendations, patients should not, where possible, be considered for elective cardiac surgery within 10 days of NOAC cessation.