Written by Dr Tim Surman
Shortcuts
Scientific Session 1 – Current best practice in coronary revascularisation
Scientific Session 2 – Current best practice mitral interventions
Scientific session 3 – Current state of the art interventions for mitral valve
Scientific session 4 – Current best practice for TV repair and treatment of AF and LAA closure
Scientific Session 5 – Current state of the art in coronary revascularisation
Scientific Session 6 – Current best practices for valve intervention
Scientific Session 7 – Current state of the art surgery for LVOT and aortic root pathologies
Scientific Session 8 – Arch and endovascular procedures for the non-super-specialised teams
Masterclass 1 – TAVI and Endovascular Aortic interventions
Masterclass 2 – VSARR, Ross and Arch and HOCM
Scientific Session 1 – Current best practice in coronary revascularisation
Gaudino – Radial Artery or Right Internal Thoracic Artery for CABG?
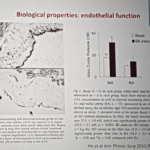
- Biological properties between RA and RITA are well known
- No clear superior choice between RITA or LITA
- Surgeon experience is the key
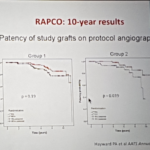
- Mid-trial results have shown equivalent survival and event-free survival and graft patency in both arms at median follow up of approximately 6 years
- Group 1 showed a 9% improved patency amongst the RA group over RITA
- Group 2 showed a 10% improved patency amongst the RA group over saphenous vein with
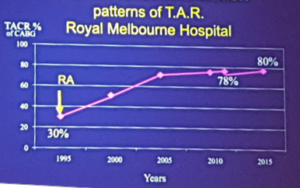
Tatoulis – Radial Artery or Right Internal Thoracic Artery for CABG?
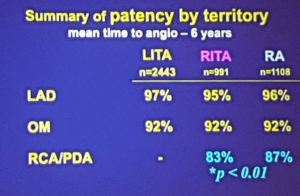
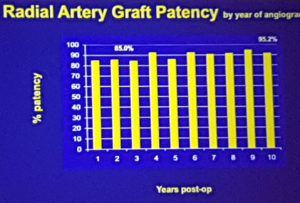
- LIMA is the superior graft conduit with 90%+ patency at 20 years
- RIMA is the second best skeletonised graft option limited by reach (A free RITA is an alternative)
- The LIMA and RIMA show identical patency’s in the same clinical situation
- RA and RITA are equivalent with RA being more versatile (open RA harvest is preferred)
- SVG is an option in older patients (preferably taken from the lower leg with decreased branches)
- Overall recommendations is total arterial revascularisation
Scientific Session 2 – Current best practice mitral interventions
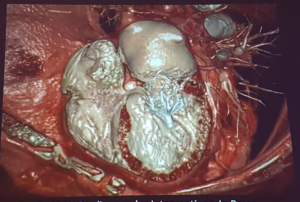
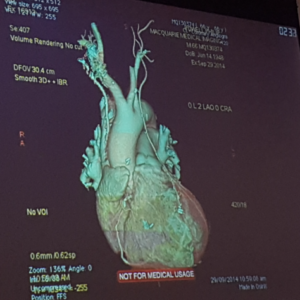
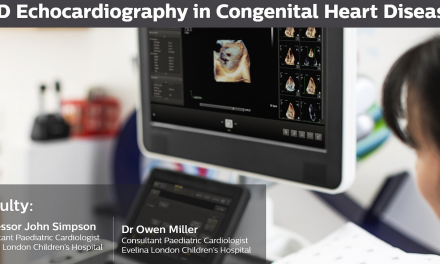
Otto – Advanced Imaging, 3D-Printing and Simulation for Mitral Valve Interventions
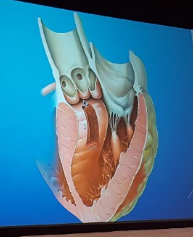
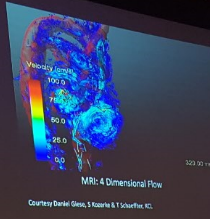
- Mitral valve can encroach on the LVOT
- New CT imaging can simulate flow
- Advanced imaging will soon enter clinical practice
Scalia – Imaging for Mitral Valve Interventions: Before the Procedure
- All views are from the surgeons view
- Lateral landmark is the LAA
- Medial landmark is the interatrial septum
- Carpentier’s classification is the basis for assessment
- 3D printing is used routinely preoperatively
- Assists in determining intrusion of the LVOT
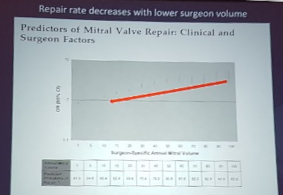
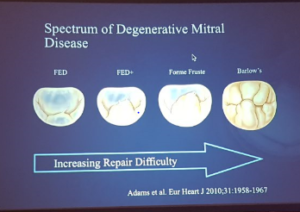
Anyanwu – What is Repairable Degenerative Valve Disease in 2018
- More important question is what is NOT reparable
- 3 factors
- Anatomical
- Surgical/institutional – high repair rate, high volume (very variable repair rate in new York)
- Mitral valve disease repair is a spectrum
- Lower repair rate with increasing difficulty
- Guides an appropriate mitral valve centre
- Patient factors
- Preoperative factors – often minimal
- Operative factors – most significant with complex repairs
- All non-calcified cusps are reparable
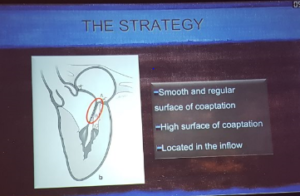
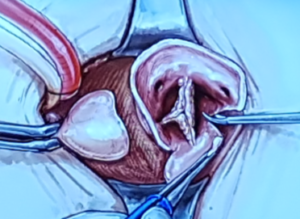
Perier – Isolated anterior or posterior leaflet repair
- The mitral valve is a complex apparatus
- To restore the valve we have to restore the area of coaptation
- Aiming for 100% repair rate can be achieved with MIMV approach and sternotomy
- “we should adapt to the mitral valve”
- We have to have systematic approach to repair
- Posterior leaflet repair
- If normal width – respect approach
- If increased width – resect approach (triangular resection)
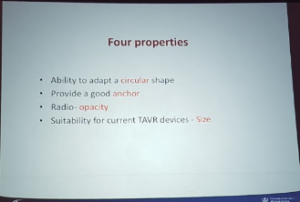
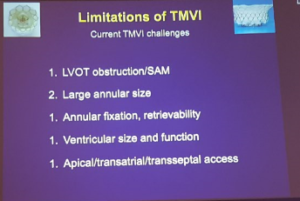
Bapat – Transcatheter mitral valve technology, current role
- There are 4 reasons for mitral transcatheter valve replacement
- There are 3 approaches – transeptal, transapical and transatrial
- Oversizing can prevent embolization or delayed embolization
- Four properties of the ring
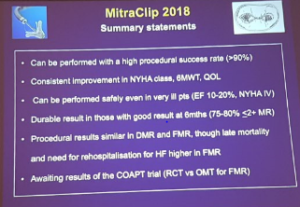
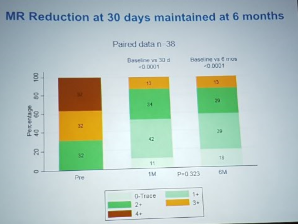
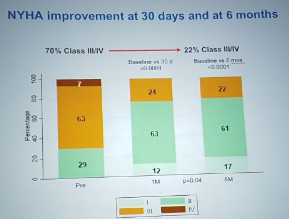
Muller – Transcatheter mitral interventions
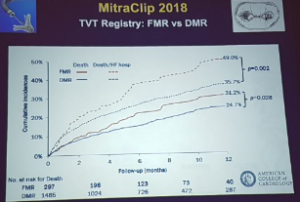
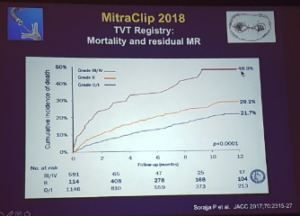
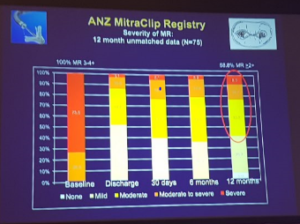
- Mitra clip – > 50,000 patients treated
- Results as 6/12 is the long term results
- Able to look at residual MR
- >50% still having residual MR at 10 years
- Combination therapies should be the approach
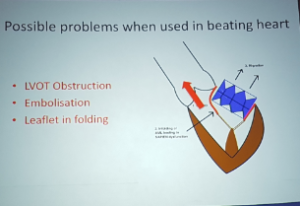
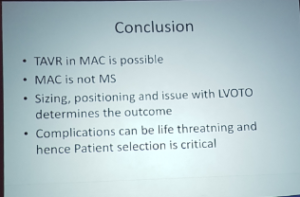
Bapat – Mitral valve annular calcification (MAC), Emerging transcatheter options
- Approaches transapical, transeptal
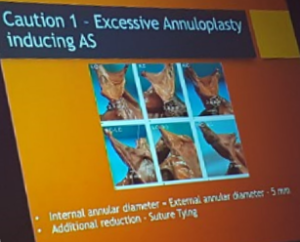
- Do not want to size and measure to include the calcification
- Less LVOT obstruction if AMI angle is obtuse
Anyanwu – Management of acute left ventricular failure after mitral valve surgery
- Failure to rescue = increased mortality
- Stop catecholamine’s
- Early recognition is important
- Resuscitate warm blood cardioplegia
- Treat the cause – often
- Poor myocardial protection
- Ischaemia
- No success then consider mechanical support early
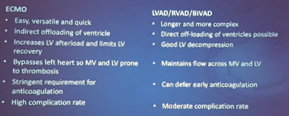
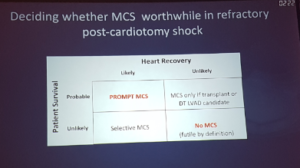
- Considerations for MCS: device choice
Scientific session 3 – Current state of the art interventions for mitral valve
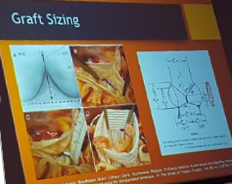
Anyanwu – Surgical tips to maximise your valve repair rate
- Take time with valve analysis!
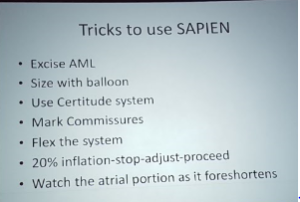
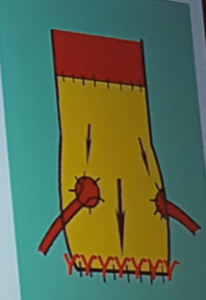
Bapat – MAC – emerging surgical options
- Teflon around the circumference of the sapian valve
- Cover the top 1/3 of Sapian
- Do not cover larger ring
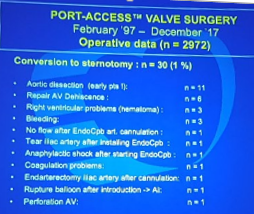
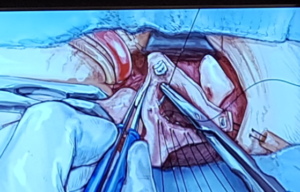
Casselman – Minimally invasive mitral valve surgery
- Intraclude device used for balloon in MIMVR
- Cryoprobe used for cryoablation
- SVC-IVC balloon catheter occlusion
- Bipolar pacemaker wire placed on diaphragm side of RV wall
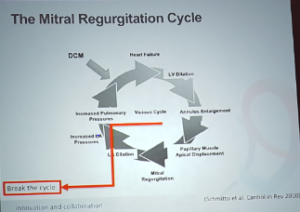
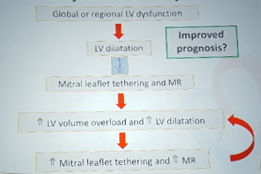
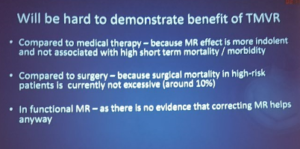
Walters – Functional MR
- 3+ 4+ MR – prognosis is worse than cancer
- The vicious cycle of MR
- The aim is to break the cycle
- The aim is a transcatheter solution via transapical approach
- Timing is important
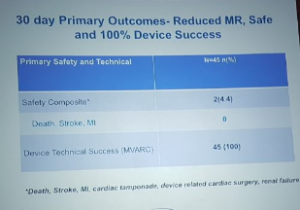
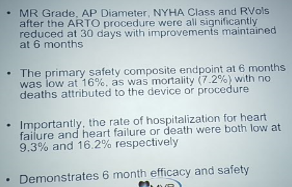
Redwood – The ARTO system for MR
- 7% mortality in low risk patients
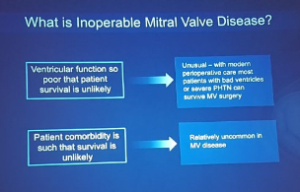
Anyanwu – TMVR – the next revolution?
- There are key differences between AVR and MVR surgeries
- Mitral valves all look different
- MVR is not a disease of the elderly therefore testing is not easy
- MV replacement is the treatment of choice
- SAM – anterior leaflet pushed in obstructing the LVOT
Scientific session 4 – Current best practice for TV repair and treatment of AF and LAA closure
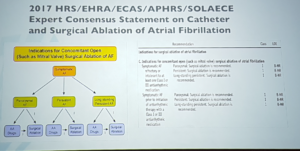
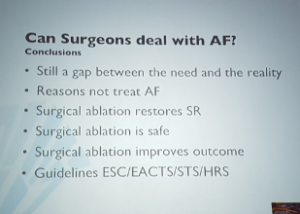
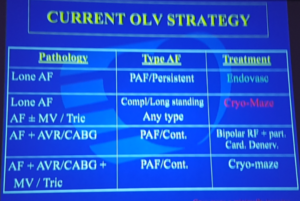
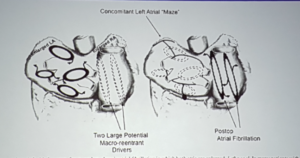
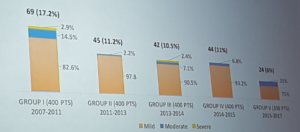
Rega – Concomitant AF ablation during open heart surgery. Can surgeons deal with AF
Casselman – Minimally invasive COX maze procedure
- Varies in cycle length in primary AF
- Secondary AF right atrium is not treated usually
- Mechanism – cells freeze, cells explode, cell death occurs
- Necrosis is greatest at the probe tip
- Free the entire RAA
- Conclusions
- Minimally invasive COX maze IV procedure is feasible
- Consistent overlapping lines are crucial
- Beware of the RA
- SSS approximately 15%
- EFO is complementary
Scalia – The LAA – is it really closed?
- LAA is viewed in 4-imaging plane
- 1 in 7 developed LAA thrombus (NEJM and klein zapi 2001)
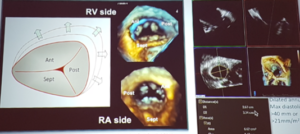
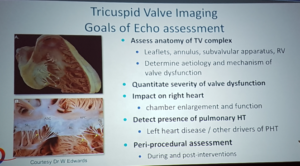
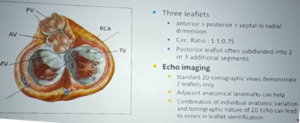
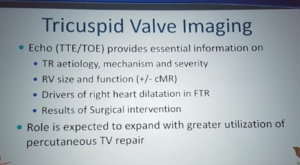
Burstow – Tricuspid valve imaging
- 3D imaging has improved leaflet identification
- Surgical correction follows Carpentier
- Tenting distance >8mm associated with severe functional TR
- Use of RA free wall strain <20% = reduced RV systolic function
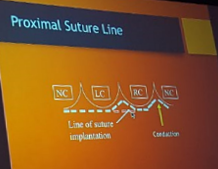
Perrier – Tricuspid valve repair
- Summary
- Treat tricuspid regurgitations
- Prevent the onset of post-operative TR
- Avoid persistence/recurrence of TR after ring implantation
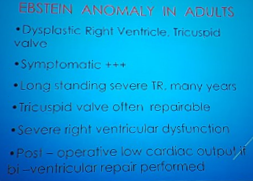
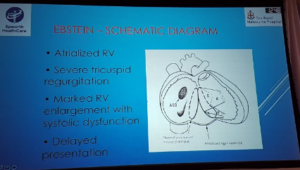
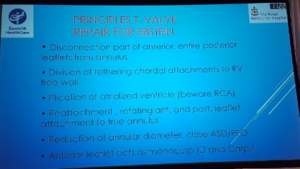
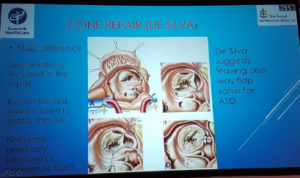
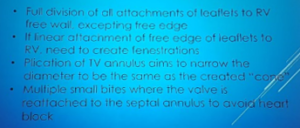
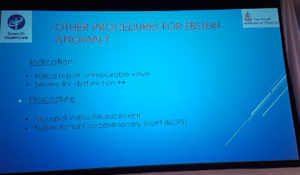
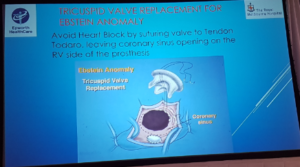
Skillington – The cone procedure and TV repair for Ebstein’s anomaly
- Previously not repair because of risk to conduction system
- Small bites taken to avoid damage to conduction system
- BCPS Bi-directional Cavo-pulmonary shunt is a useful adjunct for no failure post op
- Cone repair = best chance of perfect result
- https://www.ctsnet.org/article/cone-reconstruction-tricuspid-valve-repair-ebstein-anomaly
- TVR = good long term results
- Closure of ASD and BCPS if required
- TVR does not address the RV function
Bapat – Transcatheter tricuspid valve repair options
- TR grading of severe class = Severe – Massive – Torrential
- Tricuspid repair study – improvements in the severity of TR
- Hater double orifice repair https://www.ncbi.nlm.nih.gov/pubmed/22945241
- Triclinic repair http://4techtricuspid.com/4tech-tricinch-transcatheter-tricuspid-valve-repair-ttvr-system/
- Mitraclip for TR
- Sapian XT caval implant
- Decreases preload
Scientific Session 5 – Current state of the art in coronary revascularisation
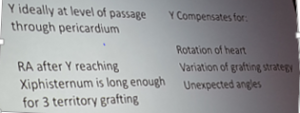
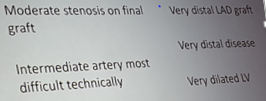
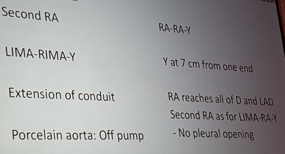
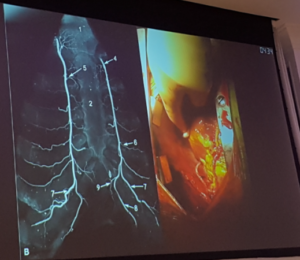
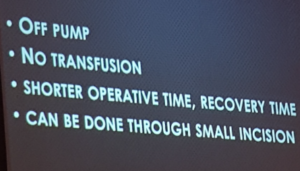
Ramponi – Dual inflow, total arterial, anaortic, off pump coronary artery bypass grafting: How to do it
- LIMA, RIMA, Radial = neurological protection
- LAA excision = neurological protection
- Strategy at institution is dual antiplatelets for 3/12 and milrinone till day 1
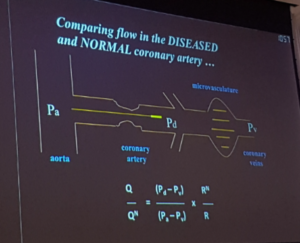
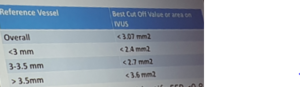
Redwood – Defining coronary anatomy and physiology: IVUS and FFR
- IVUS – reduces death, reduces thrombosis
- Evidence
- Single vessel disease – DEFER study
- Double vessel disease – FAME study
- Single vessel disease with FFR >0.75 (no ischaemia) does not need PCI and can be safely treated with medical therapy alone
- FFR > 0.75 (no ischaemia) can be used to select ARTERIES that do not need PCI and can be safely treated with medical therapy alone in single and multi-vessel disease
- FFR < 0.75 (+ ischaemia) can be used to select PATIENTS who would benefit from PCI rather than medical therapy alone
Gaudino – CABG versus PCI in multi-vessel disease
- Single graft = no benefit
- Multiple grafts = significant benefit (>1.7 grafts)
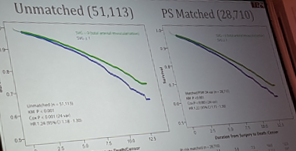
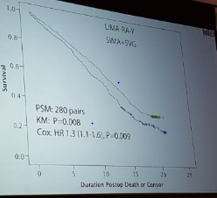
Royse – How to get arterial Y grafts right
- 22 hazard ratio (>20%) mortality with vein graft
- 1999 paper showed Hazard ratio of 1.3
Ng – Syntax score and PCI
- Synthesis of multiple coronary lesion complexity scoring systems
- Lesion severity (obstructive vs occlusive)
- Anatomic location and importance of arterial segment (Leaman score)
- Adverse lesion characteristics (ACC/AHA classification)
- Bifurcation characteristics (Medina classification)
- Total occlusion characteristics (TOTAL surveillance)
- Score shows low and high complexity coronary artery disease
- Syntax was the first CABG versus PCI trials
- 5 year outcome – no difference in low syntax score group, Benefit in CABG for intermediate syntax score and high syntax score, if 2/3 anatomical complexity then for CABG
- Conclusion is that CABG is recommended for intermediate and high risk patients
Brereton – Anaortic surgery: why should we do it and why we don’t
- Why we should do it
- To reduce the risk of stroke
- To use arterial grafts in the best possible way
- To promulgate a better treatment than PCI
- To move towards robotic coronary surgery
- To provide superior treatment in acute ischaemia*
- The reasons why we do not use it are the same
- The reduction in stroke risk
- Is less that one patient I a hundred with good on-pump techniques
- But it becomes better than PCI!
- The survival advantages
- Is late, and not seen before ten years
- Is unpredictable, for example in terms of malignancy
- Represents a lot of work for a late advantage, and fewer operations performed!
- The advantage over PCI
- Is lost when the patient is told that multi-vessel stenting is non-inferior at 1 or maybe 5 years
- The latest generation stent is being used
- The progression to robotic surgery
- This has been trialled and failed
- Robotic coronary surgery is performed in a few centres
- It is unlikely to become widely applicable
- The composite picture of anOPCABG of graft longevity, freedom from stroke, minimal invasion is a superior treatment for coronary disease
Anyanwu – When should the mitral valve be repaired in secondary MR?
- For
- Residual severe MR cay complicate immediate post operative course
- Persisting severe MR in long-term may lead to continued symptoms and/or reduced survival
- Against
- Adding MVR substantially increases the risk of surgery
- MR may decrease I severity after correction of AS or CAD
- No evidence that mitral intervention improves outcome
- Increased valve prosthesis related morbidity
- Clip therapy may be applicable for residual MR
- Repair
- As a general rule
- In optimal operating conditions
- Consider leaving alone
- High risk patient
- Annular calcification
- Suboptimal operating conditions
- Key points
- Little robust data to guide therapy
- Fix severe MR in operating room for other reason
- Fix moderate MR selectively during CABG and AVR
- GDMT remains cornerstone of treatment for severe secondary MR
- Valve replacement does not have long-term benefit over repair
- Consider LVAD/transplantation when cardiomyopathy advanced
Gaudino – Shall we use the radial artery for percutaneous procedures or for CABG?
- https://www.ncbi.nlm.nih.gov/pubmed/29519357
- Recommendations:
- The TRA should be preferred over the TFA for diagnostic angiography and PCI. This is particularly important in acute coronary syndromes and when intervention is required.
- When appropriate, the RA should be used in preference to the SV to achieve multi-arterial CABG because of its superior patency and potential for improved patient longevity. In particular, the RA may be the preferred second arterial conduit in patients who are at high risk for sternal wound complications.
- Ideally, an effort should be made to reserve one RA for TRA and the other for potential use as a conduit for CABG. Generally, the use of both RAs for TRA or for CABG is not advisable, unless there are clinical indications or conduits shortage.
- The laterality of the RA for use is at the discretion of the TRA operator. As most catheter laboratories are set up to use the right RA for TRA and most surgeons prefer to harvest the left RA, it seems reasonable to recommend that, whenever possible, TRA interventions should be performed through the right forearm, and the left arm should be reserved for possible use at surgery.
- Recommendation 4 may result in a small percent- age of cases where the left RA is unusable at surgery due to lack of ulnar compensation. Consequently, in stable patients undergoing angiography, where there is a high likelihood of severe coronary artery disease and limited available conduits for bypass in institutions where the RA is used for CABG, one may consider discussion with the patient regarding alternatives to radial access or TRA on the side with the worst ulnar compensation.
- Every effort should be made to adopt strategies to minimize RA damage during TRA, including the use of the most distal RA access point, use of miniaturized equipment, optimal intravenous antithrombotic treatment, and patent hemostasis techniques.
- In patients previously submitted to TRA, the non- punctured artery should be used for CABG. In situations where the punctured RA is the only available conduit, consideration should be given to the risk of delaying surgery, although the specific time interval required to optimize graft patency is unknown at present.
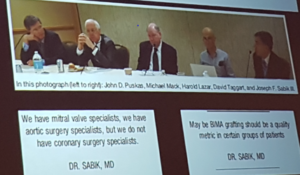
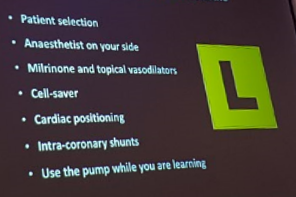
Vallely – How to build an OPCAB/MIDCABG program
- Good discussion https://www.ncbi.nlm.nih.gov/pubmed/24952761
- ROOBY trial – identified a lack of training, technique and supervision http://www.nejm.org/doi/full/10.1056/NEJMoa0902905
- Side-biter – has no role in OPCAB surgery
- Workup should be aggressive with investigating subclavian disease
- Consideration for endoscopic radial artery harvest?
- Guidelines are moving to total arterial grafting
- Open vein harvest
- Is the treatment worse than the disease?
- Often left in the ”hands” of the most junior member of the surgical team – poor quality conduit & poor quality wound(s)
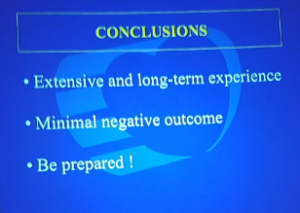
Casselman – Reasons for conversion during MIDCAB Surgery
- Summary
- Conversion in minimally invasive procedures is infrequent
- In MIDCAD surgery early conversion is mainly due to unexpected lung adhesions
- In MIDCAB surgery late conversion is related to graft dysfunction
- Conversion leads to inferior outcomes with increased morbidity and mortality
Scientific Session 6 – Current best practices for valve intervention
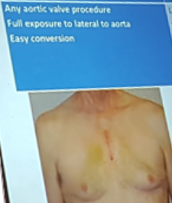
Casselman – Minimally invasive aortic valve surgery
- Hemi-sternotomy
- Any aortic valve procedure
- Full exposure to lateral aorta
- Easy conversion
- Right anterior mini thoracotomy
- Limited to uncomplicated primary aortic valve procedures
- Partial exposure to surrounding structures
- RIMA lost for future CABG
- Conversion timely and risky
- Long shafted instruments
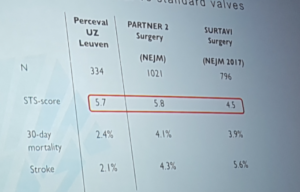
UZ Leuven – Perceval vs standard valve
- Indications
- AVR
- AVR in minimal access surgery
- AVR & Mitral valve plasty (& tricuspid valve replacement)
- AVR in damaged aortic annulus endocarditis (red)
- AVR & mitral valve replacement
- AVR in the calcified root (homograft)
- AVR in heart failure in young patients
- Conclusions
- Building evidence of good long term outcomes with Sutureless valves
- No explants or SVD
- Shorter procedural times
- Persist trial unique in its kind
- Expanding indications from minimal access to difficult to treat aortic roots
Yan – Sutureless aortic valve project: An international registry
- Current limitations of Sutureless AVR data
- Limited number of cases
- Short observational interval
- Retrospective studies
- Heterogeneous definitions of clinical variables
- Insufficient reporting of postoperative outcomes
- Lack of robust follow-up data
- There is a downward trend in paravalvular leak rate
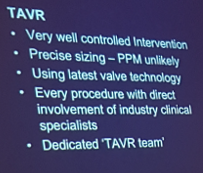
Redwood – TAVI: status in the UK and movement to intermediate to low risk patients
- Patient experience – TAVI
- 90-95% percutaneous
- 85-90% LA
- Lower morbidity
- No ICU stay
- Median stay 2-4 days
- Recovery 0-2 weeks
- More pacemakers and vascular complications
- Patient experience – SAVR
- Sternotomy
- GA, ventilation, CPB
- Higher morbidity
- 1-2 days ICU
- Median stay 5-10 days
- Recovery 2-3 months
- Conclusions
- TAVI is here to stay – an evidence-based clinical success story
- TF TAVI is equibalent and possibly superior to sAVR in high and intermiediate risk patients with respect to mortality and stroke
- TAVI is assosciated with
- Far lower morbidity than sAVR
- Preferable experience for the patient with a quicker recovery
- TAVI should be the treatment of choice NOW for all old (>80) and younger high/intermediate risk patients (70-80)
- More durability data with TAVI are needed before TAVI supplants SAVR in younger low-risk patients
- But valve in valve feasible
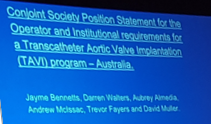
Gurvitch – TAVI: Current landscape and future directions in Australia
- Funding approved for high risk patients only
- Intermediate and low risk patients will need to fund both prosthesis and hospital costs
- Newly accredited sites without accredited operators will be unable to bill for the procedure
- Not all available devices are listed for reimbursement
- Very likely that some sites and operators will not meeting the requirements for reaccreditation
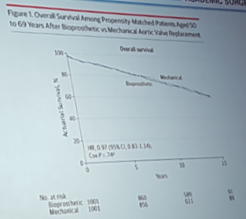
Anyanwu – Low risk TAVR trials – Saviour or nemesis
- There should be a focus on low risk trial endpoints
- Patient and doctors expect more than 1-2 year outcomes
- Low risk TAVR trials
- As designed will invariably demonstrates superiority (or non-inferiority) of TAVR over surgery in 1 to 2 year time frame
- This will lead to endorsement of TAVI in low-risk patients before true effectiveness is known
- Does the primary endpoint reflect our goals of therapy?
- Low-risk trial endpoints – alive at 1-2 years, stroke free at 1-2 years, re-hospitalisation at one year
- Are these why we intervene for aortic stenosis
- Are these the benefits and expectations we give our patients
- Is being alive and stroke free a year or two latera an achievement or an expectation?
- True determination of effectiveness of TAVY in low risk patients will come at mid-term follow-up (5 to 10 years)
- THE PLAYING FIELD AINT LEVEL
Ng – Do we need a surgeon in the room for trans-femoral TAVI?
- A surgeon and cardiologist provide complementary skill sets with the heart team approach
- Procedural teams that utilize synergistic skillsets of a cardiologist and surgeons have the broadest expertise to succeed in an evolving field
- Surgical knowledge and skills can improve day-to-day TF TAVI and is not just relevant for bailout of catastrophe
- Core skillset for TF TAVI is an endovascular – CT surgeons do need to upskill to be a relevant partner in TF TAVI
Feyers – Review of TAVI in Australia
- Absolute requirement
- Cardiac surgeon has to be in Institute at the time of TAVI
- Preferably involved in case (scrubbed)
- Surgical “team” available
- OR available
Scientific Session 7 – Current state of the art surgery for LVOT and aortic root pathologies
Bapat – How to facilitate future valve in valve procedures at the time of initial surgery
- Provide markers for sewing ring
- Provide markers for coronary ostia
Cole – Lessons from learning TAVI and why I think young surgeons should embrace transcatheter interventions
- Encompass frailty
- Muscle is our healthiest tissue
- Sarcopenia is frailty
- Who is “too frail for TAVR?”
- TAVI CT will help with sizing and provide vascular information
- Wire choice is important
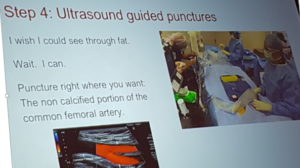
- Ultrasound guided punctures
- Puncture the non calcified portion of the common femoral artery
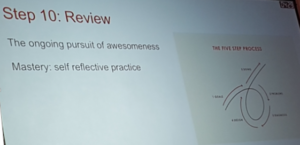
- Ongoing self review is important
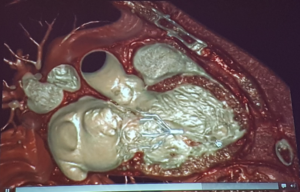
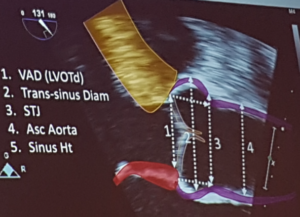
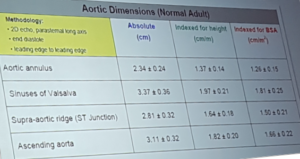
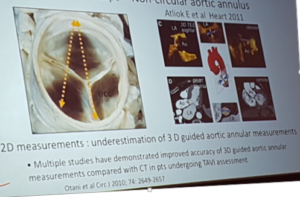
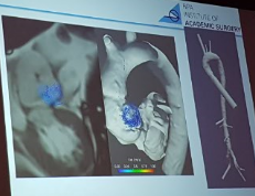
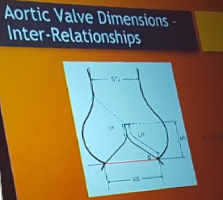
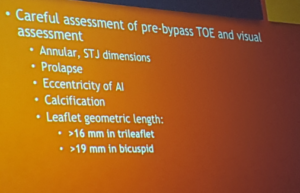
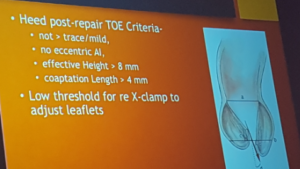
Burstow – Imaging for aortic root and aortic valve
- A functional apparatus
- Any structural abnormality causes dysfunction
- Normal aortic root dimensions
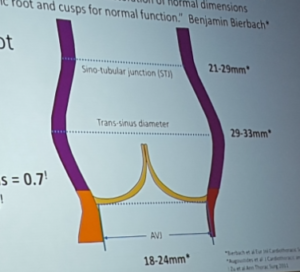
- STJ 21-29mm
- Trans-sinus diameter 29-33mm
- AVJ 18-24mm
- Asymmetric cusps = non circular aortic annulus
Bannon – Is it ethical to replace a normal or reparable aortic valve?
- David V aortic root reconstruction used in Marfan or Loeys Dietz
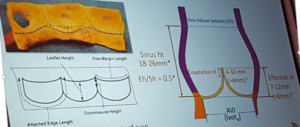
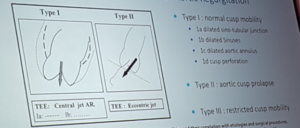
Matalanis – Mechanisms of native aortic valve failure leading to princples for aortic valve repair
- Prayer angle – uses diastolic force to ensure leaflet coaptation
- Annular dilatation – reduces coaptation zone
- STJ dilatation – failed meeting of leaflets
- Commisures closure together – leaflet prolapse and vice versa
- Free margin closure – saggy leaflets
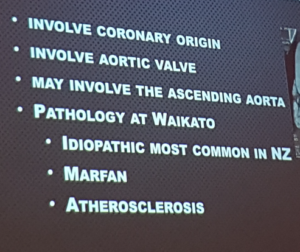
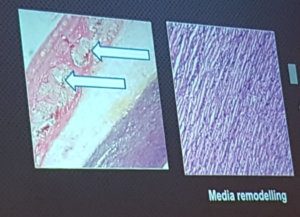
El Gamel – Personalised External Aortic Root Support (PEARS)
- The ExoVasc Personalised External Aortic Root Support aims to provide an alternative to aortic root replacement. A custom-made external support is made to exactly match the patient’s aorta. This is placed around the ascending aorta, which remains intact.
- High incidence of idiopathic aortic root dilatation
- Problem is within the media and adventitia
- Benefit in keeping patients native valve
- The first patient devised his own engineering approach to PEARS https://www.independent.co.uk/life-style/health-and-families/the-engineer-who-fixed-his-own-heart-a7397016.html
Burstow – Imaging of the LVOT and HOCM
- Role of echo in HCM and LVOTO
- Confirming the appropriate ‘morho-functional’ phenotype
- Assessing the haemodynamic characteristics of LVOTO
- Feasibility for intervention
- Detecting assosicated abnormalities
- Guidance for surgical myectomy and TASH
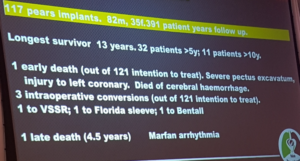
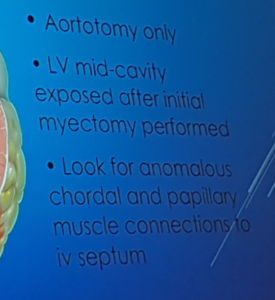
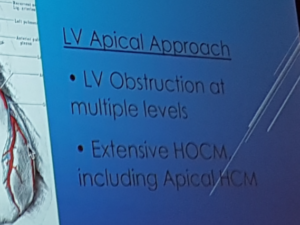
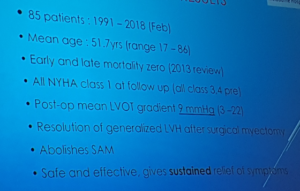
Skillington – HOCM surgical repair
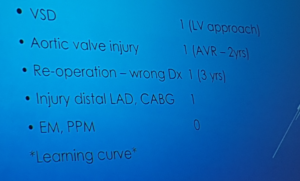
- Myectomy – effective, resolves SAM, resolves LVOT
- Alcohol septal ablation – less effective
- Be aware of the AV node
- VSD – avoid in aorto/LV approach
- Frequent bimanual assessment
- Fill heart at end of procedire – look for venous blood
- Aortic valve – care with entry, removal of scalpel blade, retraction
- Conduction defects
- Partial LBBB inevitable
- CHB only if RBBB pre-op
- Conclusions
- LV myectomy is a near-uniform successful operation, with regards to relief of symptoms and LVOT gradient
- Gold standard procedure for HOCM
- Learning
- Awareness of potential for damage to associated structures critical
- Anomalous mitral valve chordae and papillary muscles should be looked for at the time of myectomy, and if present should be divided (15-20%_
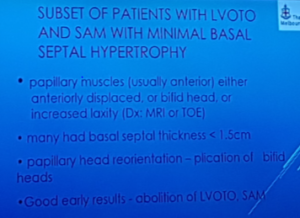
- Especially look for associated mitral or sub-mitral pathology when basal septum no significantly hypertrophoed (preop MRI)
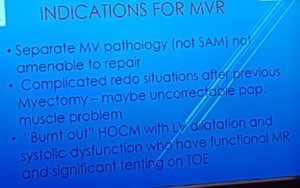
- Reserve MV replacement for unrepairable MV pathology – rare
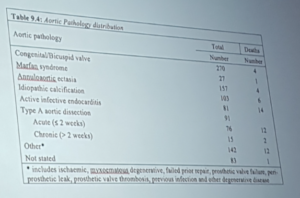
Scientific Session 8 – Arch and endovascular procedures for the non-super-specialised teams
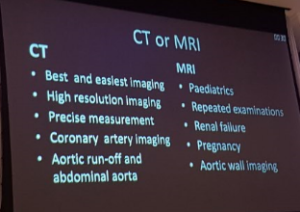
Otton – Imaging of the Aorta and Arch: MRI and CT
- Gated imaging (in diastole) – removes artefact
- Non gated (in systole) – artefac
- Black blood imaging – looking at the aortic wall
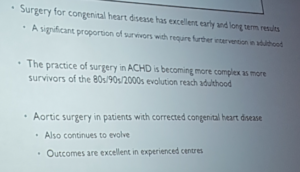
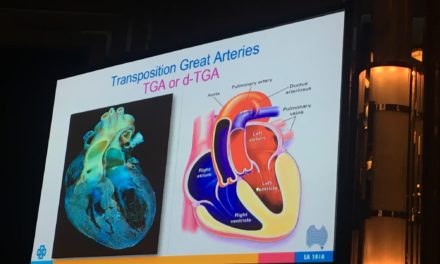
Larobina – When to operate on dilated aorta in ACHD
- With bicuspid aortic valve, the guidelines for the operator have changed
- Bicuspid aortopathy
- Variable pattern of aortopathy – root, ascending, both, or arch
- Variable family patterns
- Patern of aortopathy dictates surgical strategy
- Bicuspid aortic valve disease
- Ross is normal or mild-moderately dilated root
- Valve repair 2nd alternative
- Replace ascending aorta at 5cm
- Liberal hemiarch replacement
- Marfans syndrome
- Valve sparing root replacement optimal
- Mechanical Bentall is reasonable alternative
- Prophylactic arch replacement not necessary
- Surveillance and screening
- Adult congenital heart disease
- Surgical challenges – access, cannulation for bypass, coronary anatomy, valve hoices, ventricular dysnfunction, conduits, outflow tract obstruction
- Indications for operation
- ?natural history – dissection/rupture, rate of growth
- Aortic valve regurgitations
- Difficulty of redo surgery with larger aneurysms
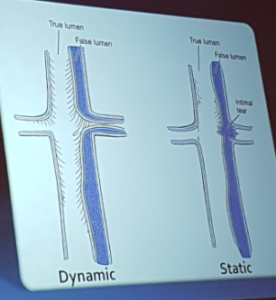
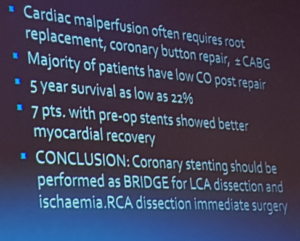
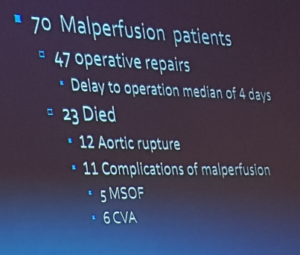
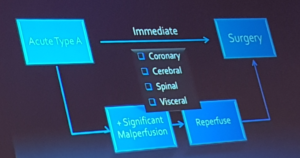
Mathur – Malperfusion in Acute Type A dissection
- Coronary malperfusion
- Risk of hospital mortality highest with preoperative CP arrest
- Significant increased in ischaemia (33% v 7%)
- By culprit artery https://www.ncbi.nlm.nih.gov/pubmed/23504116
- RCA – 17%
- LM – 49%
- LCA 47%
- LCA + RCA – 100%
- Often requires root replacement, coronary button repair, ± CABG
- Majority of patients have low CO post repair
- 5 year survival as low as 22%
- New ischaemic changes post repair
- Likely secondary to TL/FL pressure difference at the root after repair rather than extension of dissection
- Minor residual leage into the thrombosed FL -> TL compression
- CABG or PCI may be required
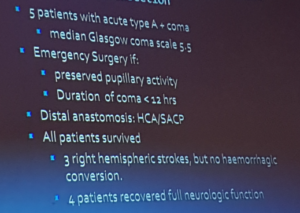
- Coma might not preclude operation in Type A Aortic Dissection
Forrest – Team work to improve organ protection and hemostasis in aortic and arch surgery
- Blood conservation for aortic surgery
- Cease antiplatelets agents preop
- Correct preoperative anaemia
- Rountine use of antifibrinolytics
- Cell salvage
- Transfusion threahold: Hct <20 on CPB, <25 post-CPB
- Modified CPB circuit
- Ultrafiltration
- Point of care coagulation tests
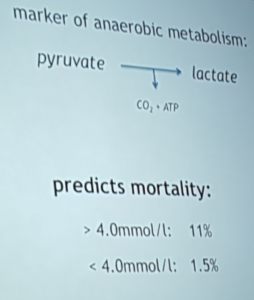
- Increased blood lactate during CPB is a marker of anaerobic metabolism
- Predicts mortality
- >4.0 = 11%
- <4.0 = 1.5%
- Thoraco-abdominal aneurysm repair = biggest anesthetic challenge
- Dexmedetomadine versus placebo in 200 CPB cases
- AKI 14 vs. 33% (p=0.002)
- Decreased morbidity and ICU stay
- Hyperthermia increase cognitive dysfunction
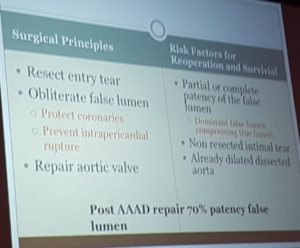
French – Aortic and Arch surgeries that every competent CT surgeon and team should be able to perform
- SurgicaL exposure for type A involves extenson into the nexk to expose the great vessels
- Surgery ois 90% esxposure and 10% skill
- Entry tear is resected à false lumen is obliterated à normal sized aorta
Matalantis – When should arch surgery be done by a specialised aortic surgeon
- Deep hypothermic arrest > 20 minutes results in neurological consequences
- Cerebral perfusion would provide >20minutes (selective antegrade and retrograde)
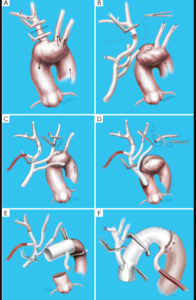
- Branch first technique http://www.annalscts.com/article/view/1694/2381
Masterclass 1 – TAVI and Endovascular Aortic interventions
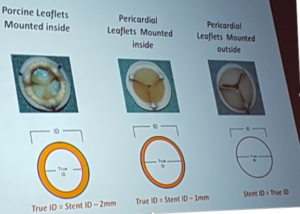
Bapat – TAVR: alternate access
- Selfexpanding Evolut R and Pro version are preferable in
- Small canuli
- Calcified aorrtic root
- VIV with true ID <19
- Small peripheral access
Redwood – Alternate access – Transcaval TAVI
- Good option when access is difficult
- Leak out of the aorta is going to go into the IVC due to pressure difference
- Snare grabs wire and ascends up the descen ding aorta
- Occluder is reployed
- Ignore the IVC hole
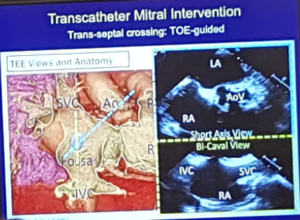
Muller – Learning transcatheter mitral interventions
- Fluroscopy over a stiff wire in times of difficult venous access
- TOE guidance in bicaval and short axis view is recommended
Bapat – Right Anterior Thoracotomy approach
- Right anterior thoracotomy – easy to convert
- Good LV is critical
- Big learning curve
- Emphasis on the team approach
- Careful with mini aortic clamp
- Cross clamp time is longer
Perrier – Why did I change to minimally invasive mitral valve surgery?
- The early stages of MI surgery were disasterous
- Mortality 9.8%
- Progressive increase in complexity of procedures
- Rate of blood transfusion decreased
- Trace regurgitation on discharge
- Learning curve of approximately 200 patients
El Gamel – De-airing in mitral MI procedures
- Humidified CO2 simplifies deairing
- Deairing should follow the law of gases
- Shaking the field with CO2 in it, witll create more bubbles
- http://www.heartlungcirc.org/article/S1443-9506(14)00929-9/fulltext
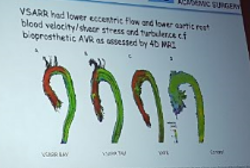
Masterclass 2 – VSARR, Ross and Arch and HOCM
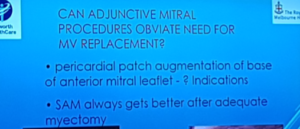
Skillington – Should we ever need to replace the MV in HOCM?
- SAM always gets better after successful myectomy
- Papillary muscle debuling or reorientation is usually required
- In regards to prosthetic type – mechanical à reduces risk of LVOTO, bioprosthetic à beware LVOTO due to strut posts but is probably overstated
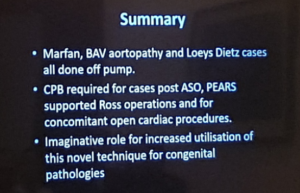
El Gamel – PEARS – how to, tips and tricks
- There should be early intervention in families with Marfans history
- PEARS graft is soft and pliable
- Take care around the LM coronary artery
- Consider it a 2 consultant operation
- Expensive
Yan – Minimally invasive aortic arch surgery
- Davids procedure – tie sutures gently due to risk of tearing the subannular membrane
- Mortality was 1.4% in 70 patients
- No sternal wound infections