Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been published recently in each speciality (cardiology, cardiothoracic surgery, cardiac imaging, perioperative medicine).
Cardiology – summarised by Ruth Hadfield
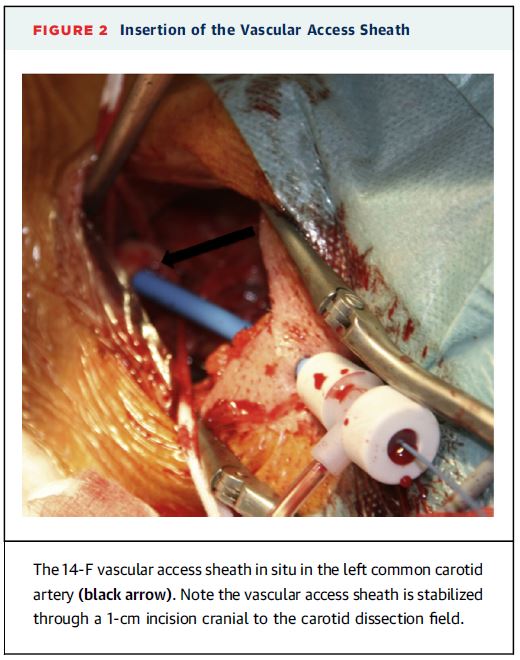
Transcarotid arterial access may be an option for patients that have vascular anatomy that makes transfemoral access problematic. In this French study of 96 elderly patients transcarotid transcatheter aortic valve replacement (TAVR) was assessed for safety. The mean Society of Thoracic Surgeons predicted risk of mortality score for these patients was 7.1%, and 92.7% were NYHA functional class III or IV.
Overall there were 3/96 procedural deaths. The 30-day and 1-year mortality rates were 6.3% and 16.7% respectively. There were 6 cases of transient ischemic attack (TIA) rate by 30 days.
The authors concluded that:
“Transcarotid vascular access for TAVR is feasible and is associated with encouraging short- and medium-term clinical outcomes.”
They also recommended that further prospective studies should be conducted to compare the safety and efficacy of transcarotid TAVR with other nonfemoral vascular access routes.
In a trial of 2,032 intermediate-risk patients with severe aortic stenosis that compared transcatheter (TAVR) or surgical aortic-valve replacement it was found that the primary end point of death or disabling stroke was comparable for both procedures.
The randomised trial was conducted across 57 centres and assessed the primary end point of death from any cause or disabling stroke at 2 years. Pre-randomisation clinical and imaging findings were used to divide patients into cohorts for either transfemoral (76.3%) or transthoracic (23.7%) access.
The frequency of death or disabling stroke did not differ significantly between the TAVR and surgical aortic-valve replacement groups (19.3% vs 21.1%; HR 0.89; P=0.25).
However, in those patients undergoing transfemoral-access cohort, TAVR resulted in a lower rate of death or disabling stroke than surgery (HR 0.79; 95% CI, 0.62 to 1.00; P=0.05).
“We found that in intermediate risk patients with severe symptomatic aortic stenosis, surgical and transcatheter valve replacement were similar with respect to the primary end point of death or disabling stroke for up to 2 years and resulted in a similar degree of lessening of cardiac symptoms,” the researcher’s concluded.
A NEJM QuickTake Video about this trial is available here.
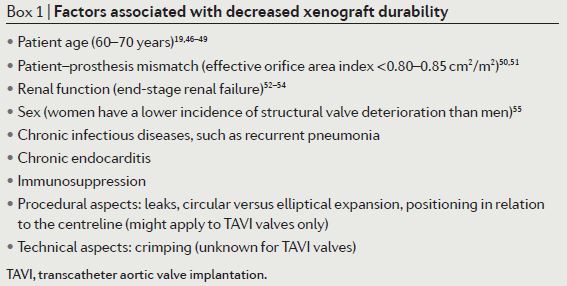
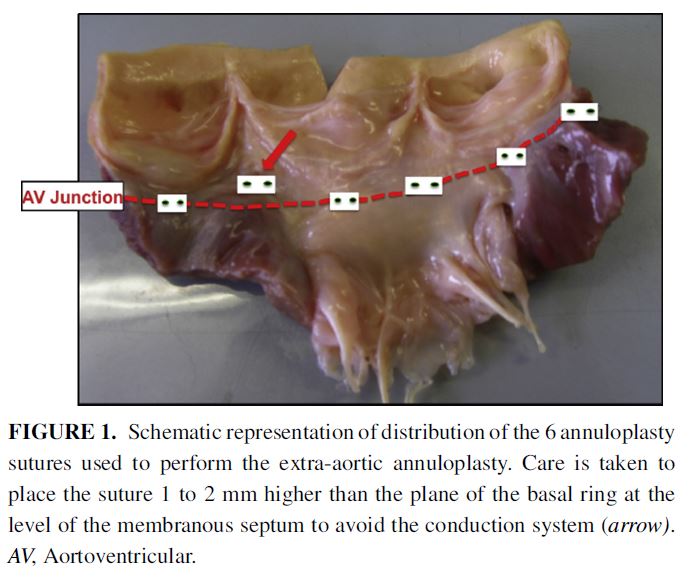
This overview summarises the evidence on transcatheter aortic valve implantation (TAVI) device durability. Until recently, TAVI was predominantly conducted in elderly or high-risk patients and therefore device durability was not a major consideration. A number of factors influence xenograft durability (Box 1) including age and an inverse association between age and structural valve deterioration exists.
Structural valve deterioration is age-dependent and is slow initially in patients aged >65years with reported rates of early valve failure <1% after 5 years and around 10% after 10 years. However, in patients <35 years high rates of structural valve deterioration have been reported, due to enhanced immunity and metabolism.
As TAVI is now being utilised in younger and intermediate-risk patients, and it is a relatively new treatment option for patients with aortic valve disease, device durability has become a more important consideration. In addition to wear and tear and calcification, common reasons for bioprosthetic valve failure include pannus, endocarditis and thrombus.
At present long-term data for TAVI devices is only available for up to 5 years. This review identifies only 4 studies in the literature assessing TAVI valve durability for ≥5years, with SVD ranging from 0 – 3.4% (see Fig below). However, the authors caution that:
“Unfortunately, owing to the fairly small number of valves implanted a sufficient time ago, these reports have limited informative value that should not be generalized or extrapolated to other devices or to longer durations of follow-up.”
Cardiothoracic Surgery – summarised by Andrew Haymet
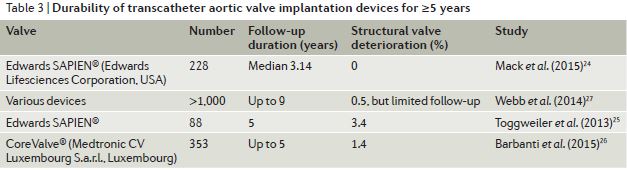
Dilation of the aortic annulus, commonly performed during Ross or Yacoub procedures, is a cause of recurrent aortic regurgitation. This study evaluated the early efficacy and mid-term stability of this surgical technique. Between 2011 and 2015, 50 patients (mean age 43 +/- 14 years) underwent adjunct extra-aortic annuloplasty ring implantation (n=39 Dacron rings and n=11 ExAo rings (CORONEO Inc, Montreal, Canada). Its use resulted in a significant decrease in both systolic (27.9+/-0.5mm preoperatively vs 23.6 +/- 0.3mm at discharge, P<0.001) and diastolic dimensions (24.8 +/-0.4mm preoperatively vs 20.3 +/- 0.3mm at discharge, P<0.001). This remained stable at mid-term follow up, however further studies are required to determine long term continuation of these results.
Pulmonary hypertension (PHT) has been considered a risk factor for mortality in cardiac surgery. This study of 1571 patients undergoing mitral valve surgery (MVS) between 2004-2013 sought to ascertain whether severe PHT increases mortality risk, and if patients who undergo concomitant tricuspid valve surgery (TVS) incur additional risk. Patients with severe PHT had higher mortality in both 30-day and 5 year survival (4% PHT vs 1% no PHT, p<0.02, and 75.5% severe vs 91.9% no PHT (P<0.001) respectively). Mortality in MVS is unaffected by severe PHT or the addition of TVS, however extreme PHT remains a risk factor.
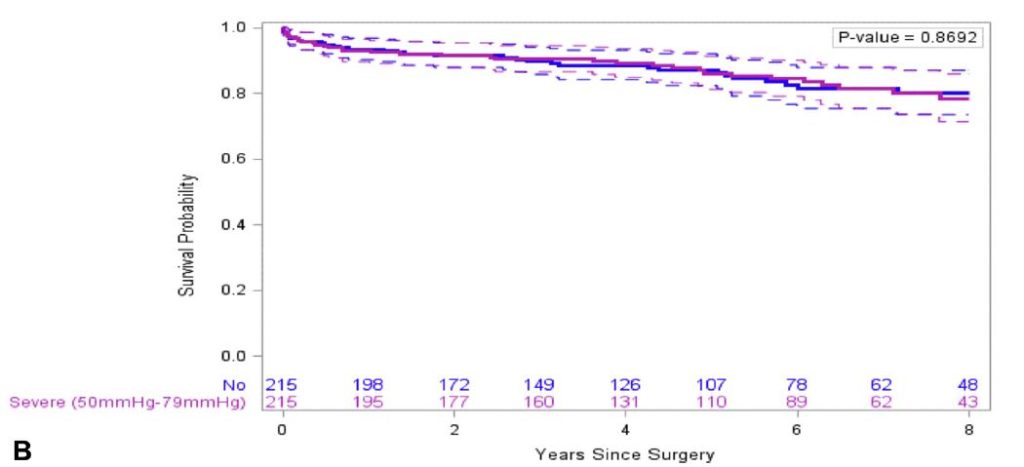
Figure legend: Kaplan-Meier survival estimates in PS-matched analyses for severe versus no PHT.
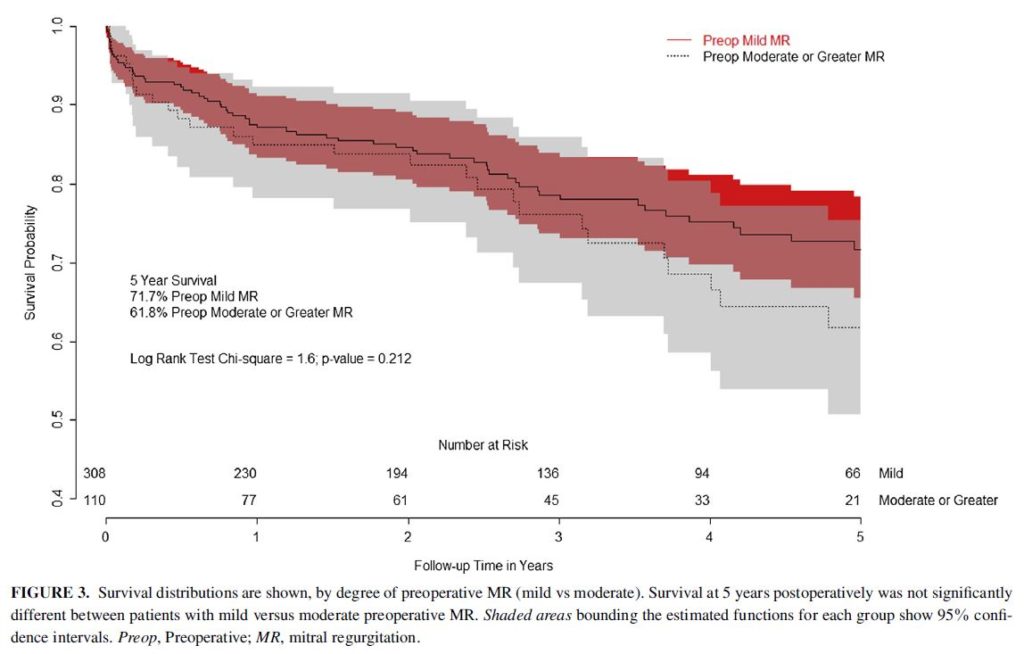
The long-term evolution of coexistent mitral regurgitation (MR) after aortic valve replacement (AVR) remains unclear. The evolution of MR after AVR was investigated in a retrospective study of 423 patients who underwent primary isolated AVR from 2004-2013, along with prognostic indicators for MR improvement. The overall acute reduction in MR was -0.23 degrees per patient. The reduction in MR for patients with moderate and mild MR was -0.53 and -0.13 degrees respectively (p<0.001). Patients with a lower degree of MR after AVR had superior long term survival. More aggressive treatment of MR should be considered at the time of AVR.
TAVR with the Sapien 3 has shown promising 30-day clinical outcomes in patients with severe aortic stenosis who are at risk of surgical mortality. This observational study compared all-cause mortality, stroke, re-intervention and aortic regurgitation of 1077 patients receiving TAVR between February and September 2014 in the USA and Canada, with 1-year outcomes with intermediate risk patients treated with SAVR in the PARTNER 2A trial between 2011 and 2013. At 1 year follow-up, for the primary composite endpoint of mortality, strokes and moderate or severe aortic regurgitation, TAVR was both non-inferior (pooled weighted proportion difference of –9·2%; 90% CI –12·4 to –6; p<0·0001) and superior (–9·2%, 95% CI –13·0 to –5·4; p<0·0001) to surgical valve replacement.
Cardiac Imaging – summarised by Ruth Hadfield
This study investigated patients with chronic pulmonary hypertension to compare three-dimensional (3D), and 2D and 3D speckle-tracking (2D-STE, 3D-STE) echocardiographic parameters with conventional right ventricular (RV) echocardiographic parameters. The aim was to ascertain which method correlates best with the haemodynamic variables characteristic of heart failure. Healthy subjects were used as controls.
The researchers reported that:
“RV 3D global-free-wall longitudinal strain (3DGFW-RVLS), 2D global-free-wall longitudinal strain (GFW-RVLS), apical-free-wall longitudinal strain, basal-free-wall longitudinal strain, and 3D-RVEF were lower in patients with pre-capillary pulmonary hypertension (P<0.0001) and post-capillary pulmonary hypertension (P<0.01) compared to controls.”
Furthermore, they found that 3DGFW-RVLS and 3D-RVEF were independent predictors of mortality. It was concluded that, in chronic pulmonary hypertension, 3D, 2D-STE and 3D-STE parameters are better indicators of global and regional RV dysfunction than conventional echocardiographic RV indices.
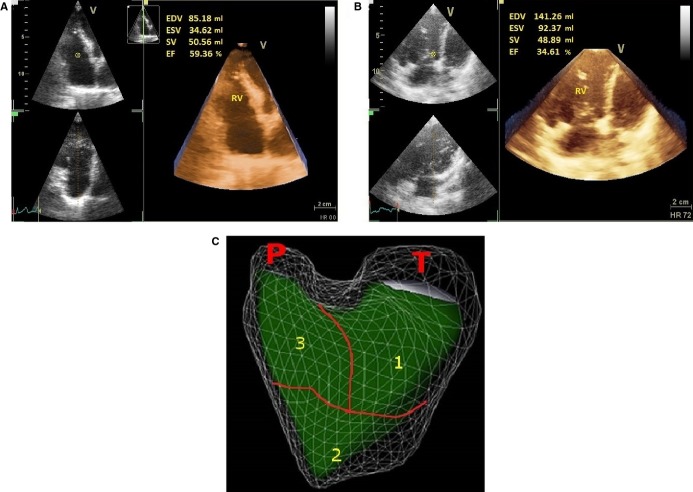
Figure: Representative 3D RV volumes and ejection fraction in normal controls and PH patients. A, Three‐dimensional RV ejection fraction (3D‐RVEF) in a normal subject. 3D‐RVEF=59%. B, Decrease of 3D‐RVEF in a patient with chronic PH. 3D‐RVEF=35%. C, Regional three‐dimensional RV ejection fraction. RV components are illustrated in a three‐dimensional reconstruction of the echocardiographic images seen in a front view. 1, inlet; 2, apical trabecular; 3, outlet component. EDV indicates end‐diastolic volume; EF, ejection fraction; ESV, end‐systolic volume; P, pulmonary outflow; PH, pulmonary hypertension; RV, right ventricular; RVEF, RV ejection fraction; SV, stroke volume; T, tricuspid inflow.
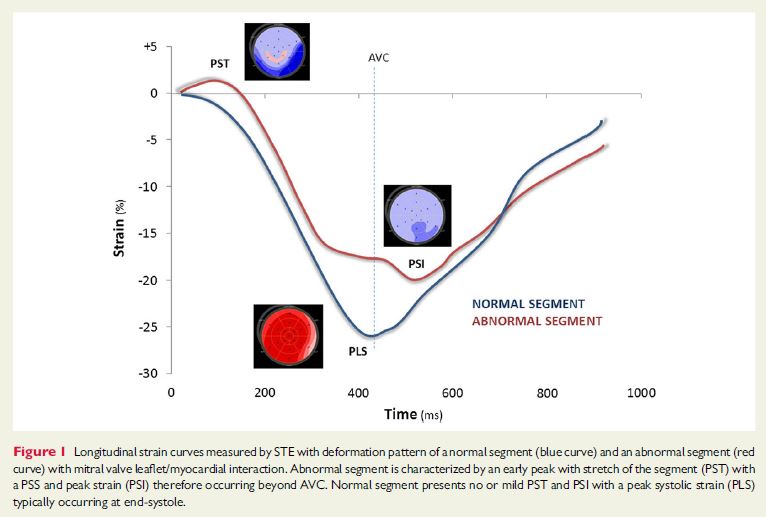
This new study adds weight to the hypothesis that in patients with mitral valve prolapse, pathological early-systolic shortening and late systolic, post-systolic deformation result from increased interaction between wall deformation and mitral valve events.
“Our findings suggest that the mechanical interaction between MVP and LV wall through chordae and papillary muscles can potentially change temporal segmental myocardial deformation patterns,” the authors conclude in their European Heart Journal Cardiovascular Imaging manuscript.
In patients with mitral valve prolapse atypical lateral wall kinetics are often observed at 2D echocardiography. MVR patients may present with symptoms such as atypical chest pain, palpitation, or syncope but the reason for such symptoms are unclear. It is thought a number of mechanisms could affect the function of the LV wall leading to ventricular arrhythmias, such as chordal tension throughout systole and non-uniformity of muscle contraction with isovolumic stretch.
The researchers also concluded that speckle tracking echocardiography is a valuable tool for assessing the interaction between MV leaflets and myocardium.
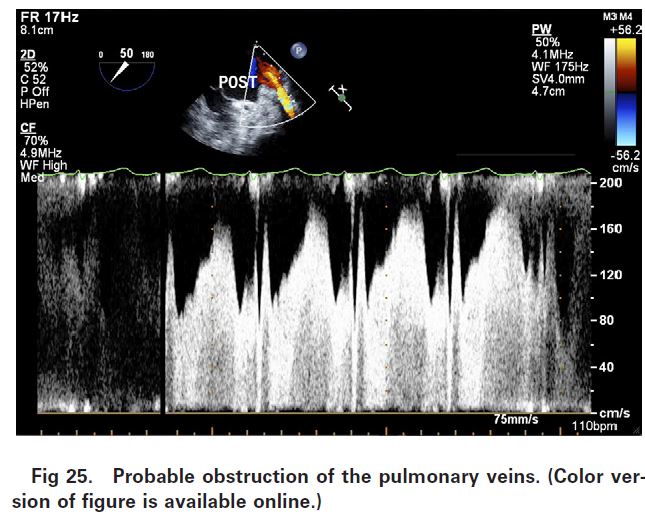
This comprehensive review aims to bridge the gap between what is taught in many transoesophageal echocardiography (TEE) courses and a lack of knowledge about intraoperative TEE, leading to a missed opportunity for intraoperative pulmonary vein inspection, imaging and examination.
Suggestions for pulmonary vein sonography by TEE, and a discussion of the ability to conduct intraoperative imaging and Doppler of the PVs is included in the review. Topics covered include background PV embryology and the more recent anatomic discoveries that relate to the pulmonary vein.
“The intraoperative TEE examination is performed in the setting of variable changes in hemodynamics, and with an appreciation of the embryology and variations in the development of pulmonary venous anatomy, the cardiac anesthesiologist is well placed to delineate the anatomy and differentiate physiology and pathophysiology through the use of 2-dimensional and Doppler examinations,” the authors of the review conclude.
Perioperative Medicine – summarised by Ruth Hadfield
This article highlights the major research breakthroughs in cardiothoracic and vascular anaesthesia during 2015. Key research discussed includes the ‘mitral valve revolution’ and new evidence from the Cardiothoracic Trials Surgical Network (CTSN) following publication of the results of two recent RCTs.
In the first, Acker et al compared mitral valve repair versus replacement in severe ischemic mitral regurgitation (MR) patients, and found that the risk of recurrence at 12 months was significantly higher for the repair (32.6% vs 2.3%; p<0.001).
In the second RCT, Smith et al investigated 301 patients with moderate ischemic MR. Patients were randomised to receive coronary artery bypass grafting (CABG) alone or CABG with mitral valve repair. There was no significant difference between groups for the primary outcome of LV end-systolic volume index at 1-year (p=0.61). Risk of recurrence was lower in the MV repair group, but the investigators concluded that “there was not meaningful advantage to adding MV repair to CABG in patients with incidental moderate MR.”
This review also discussed surgical intervention for asymptomatic severe mitral valve regurgitation, the role of TEE & 3D TEE in mitral imaging, percutaneous mitral valve interventions.
They also outline and summarise the new thermal guidelines for cardiopulmonary bypass (see Fig below). The new recommendations followed from a 2011 survey which reported that during re-warming after induced mild hypothermia during cardiopulmonary bypass, 44% of centres exceeded a peak temperature of 37˚C. Furthermore, very low rates of routine calibration of arterial line temperature probes were also reported, which is likely to result in erroneous readings.
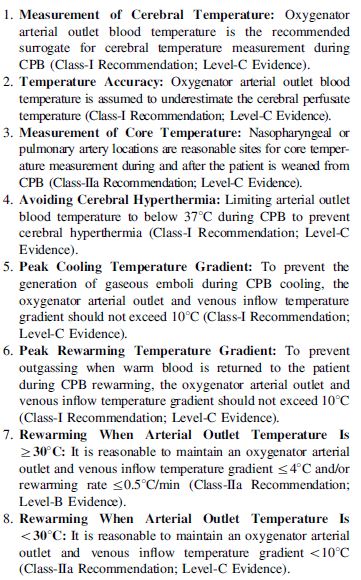
Figure: Thermal guidelines for cardiopulmonary bypass.
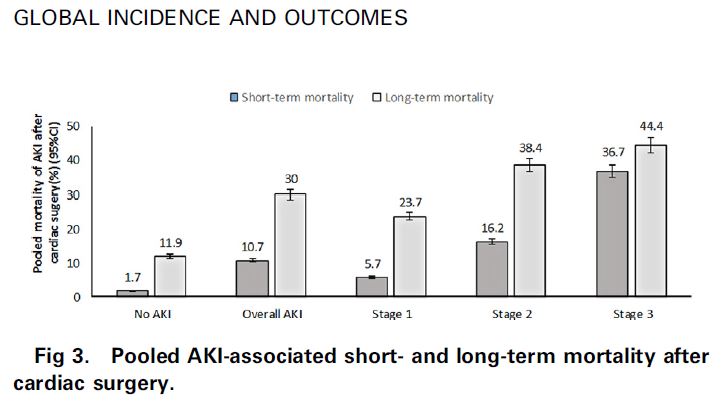
Acute kidney injury (AKI) is a common and serious postoperative problem following cardiac surgery. AKI results from multiple pathways including prolonged cardiopulmonary bypass and the resulting inflammatory response, and long duration aortic cross-clamping and associated cardiac ischaemia reperfusion injury.
This systematic review and meta-analysis was conducted to determine the global incidence and outcomes of acute kidney injury (AKI) following cardiac surgery. A total of 91 studies (320,086 patients) were eligible for inclusion and the pooled incidence rate of AKI was 22.3%.
Short-term AKI mortality (pooled) was 10.7% and long-term mortality was 30% (see Fig below). Both short and long-term mortality were significantly higher for patients with AKI than patients without. Average length of time spent in ICU and hospital were also longer for those cardiac surgery patients who developed AKI at 5.4 and 15 days, respectively compared to 2.2 and 10.5 days in patients who did not develop AKI.
“AKI is a great burden for patients undergoing cardiac surgery and can affect short-term and long-term prognoses of these patients,” the authors concluded.
New study suggests point-of-care testing may be lacking.
Point-of-care testing allows rapid patient assessment and has a number of advantages. The aim of this study was to compare haemoglobin and haematocrit readings from three different devices for accuracy and reliability. The devices tested were the Radical-7 pulse oximeter (Radical-7, Neuchȃtel, Switzerland), the i-STAT (Abbott Point of Care, Princeton, NJ), and the GEM 4000 (Instrumentation Laboratory, Bedford, MA). Results obtained were compared to reference values from a hospital cellular analysis system, the UniCel DxH 800 (Beckman Coulter, Brea, CA).
The study was conducted in 24 cardiac surgery patients at 96 different time points. Correlation with the hospital reference value was best with the GEM 4000 and i-STAT devices (see Fig below). Mean bias was lowest with the i-STAT device (Hct 0.22%; Hgb 0.05 g/dL).
Interestingly, for all devices changes in accuracy of measurement were noted following and/or during surgery. For example, the GEM 4000 device consistently produced higher readings than the reference values but after bypass surgery the readings were closer to the reference. The i-STAT device also had a bias towards higher readings, which changed to readings lower than the reference in the post-cardiopulmonary bypass period.
“Important clinical differences and limitations were found among the three point-of-care testing devices that should caution clinicians from relying on these data as sole determinants of when or when not to perform transfusion in patients,” the researchers concluded.














