Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been recently published in each speciality (Cardiology, Cardiac Surgery, Cardiac Imaging, Perioperative Medicine).
Cardiology
Summarised by Dr Sarah Catchpoole
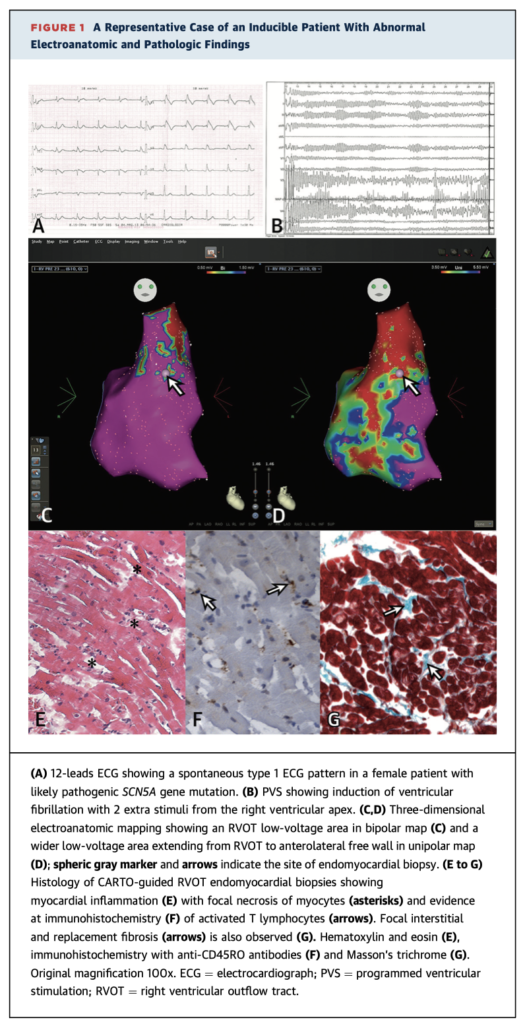
In 30 patients with Brugada syndrome, 3D electroanatomic unipolar mapping revealed areas of low voltage in the right ventricular outflow tract (RVOT) in 93% of patients. In addition, endomyocardial biopsies from the RVOT showed evidence of myocardial inflammation in up to 80% of patients. There was a higher rate of myocardial inflammation in patients inducible by programmed ventricular stimulation (83% vs. 25% in noninducible, p=0.032). The findings challenge the traditional conception of Brugada Syndrome as a channelopathy without structural heart disease, and demonstrate a localisation of pathology to the RVOT.
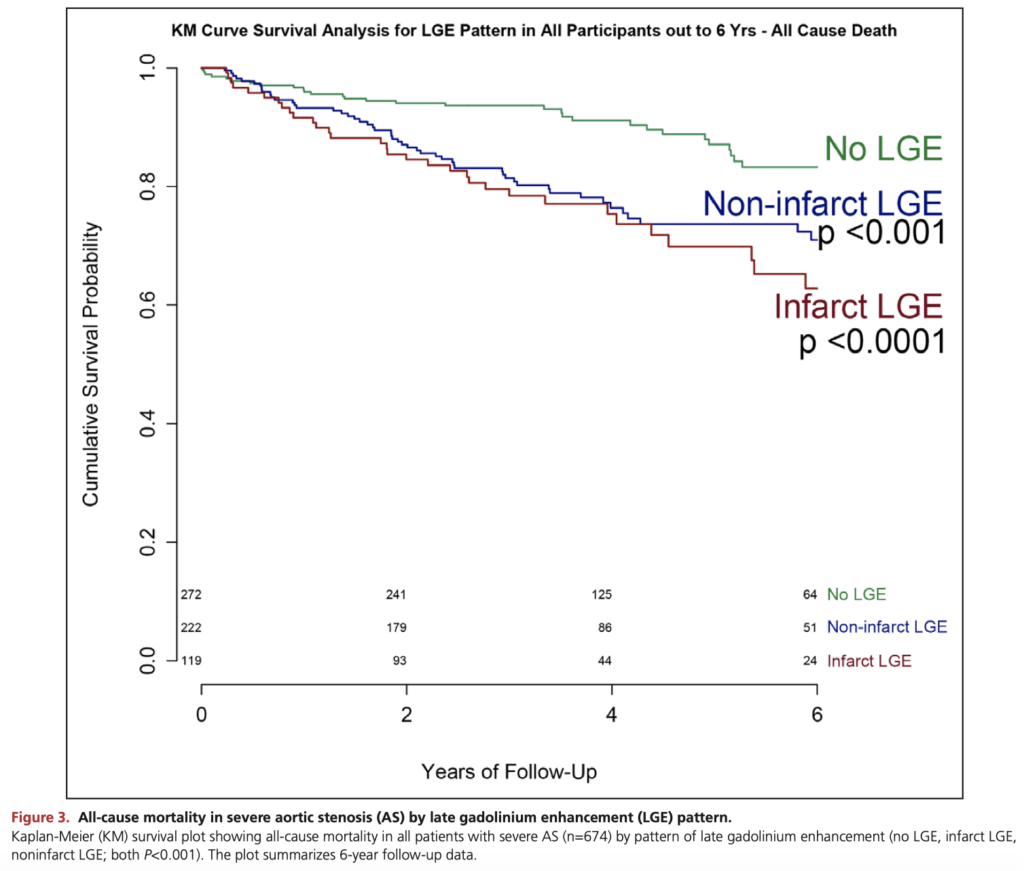
Musa TA, et al. Myocardial Scar and Mortality in Severe Aortic Stenosis. Circulation. 2018 Oct 30.
A longitudinal observational study of 674 patients with severe aortic stenosis (AS) who underwent surgical (n=399) or transcatheter (n=275) valve replacement. At baseline, 51% had focal myocardial fibrosis evident on cardiac MRI. The presence of scar was a strongly associated with higher mortality (HR 2.39, p=0.001), and independently predicted both all-cause mortality and cardiovascular mortality regardless of valve replacement type. The authors conclude late gadolinium enhancement indicating left ventricular remodelling appears to be a useful biomarker of AS progression, and suggest randomised trials of earlier valve replacement.
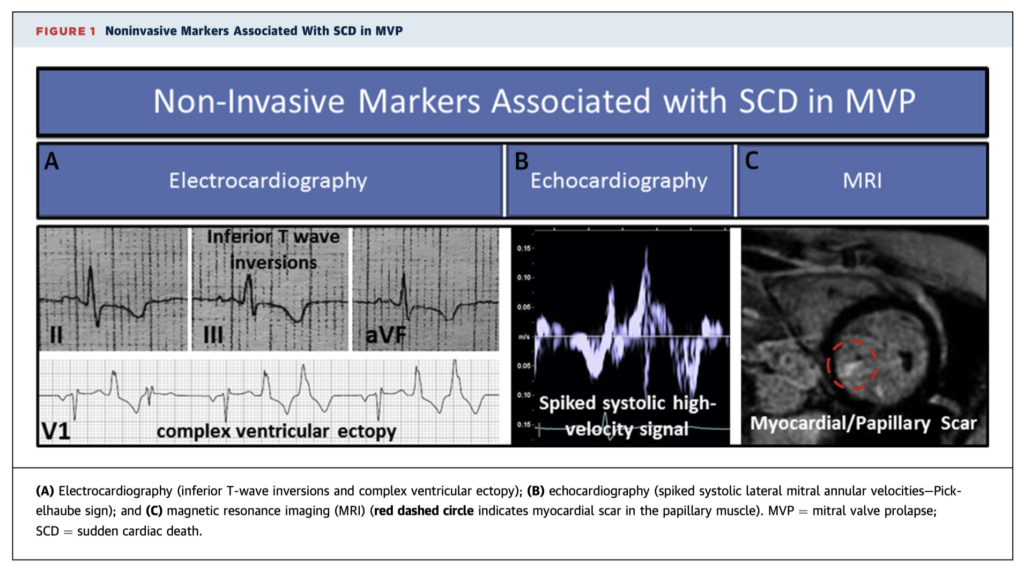
Mitral Valve Prolapse (MVP) affects 1-3% of the population, with emerging autopsy and observational studies estimating an annual risk of sudden cardiac death (SCD) between 0.2% to 1.9%. This review examines the known literature of MVP and SCD, including the mechanism of ventricular arrhythmias, identification and stratification of at-risk patients, and potential interventions for primary prevention.
Cardiac Surgery
Summarised by Dr Andrew Haymet
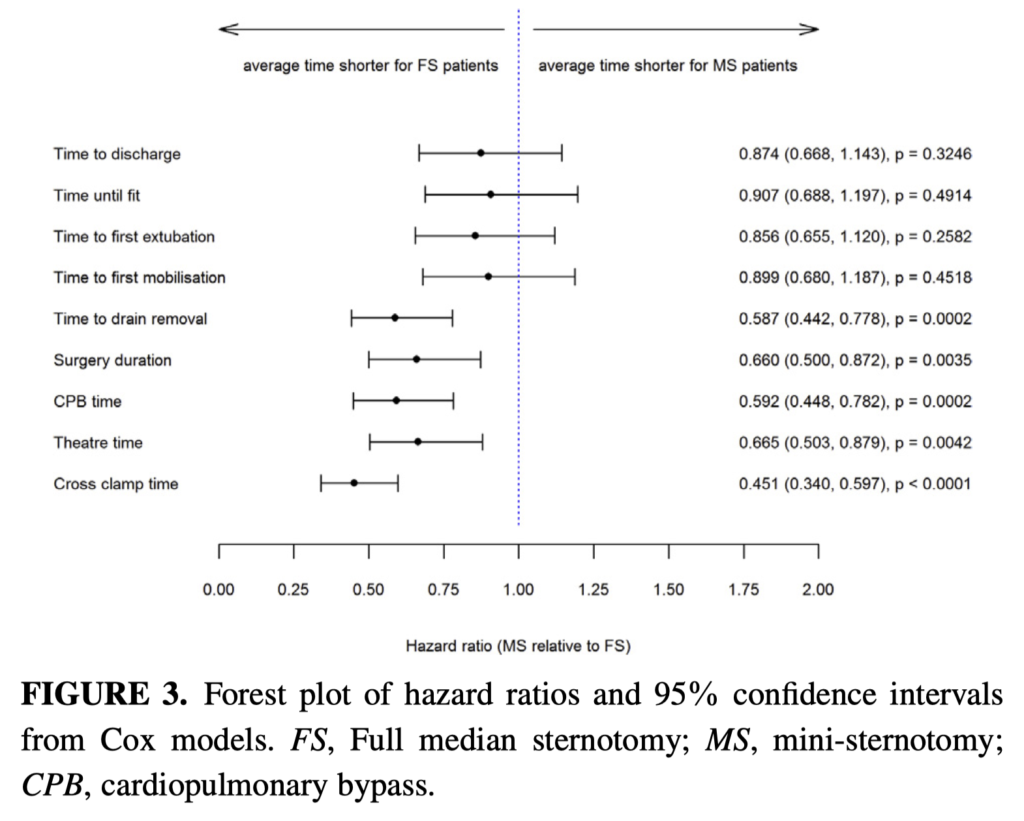
Aortic valve replacement can be performed through full sternotomy (FS) or upper hemi sternotomy (MS) (usually to the level of the 4th interspace). This open label parallel RCT with 222 patients compared MS with FS for first-time AVR in two UK NHS hospitals. The authors concluded that compared with FS for AVR, MS did not result in shorter hospital stay, faster recovery or improved survival and was not cost effective.
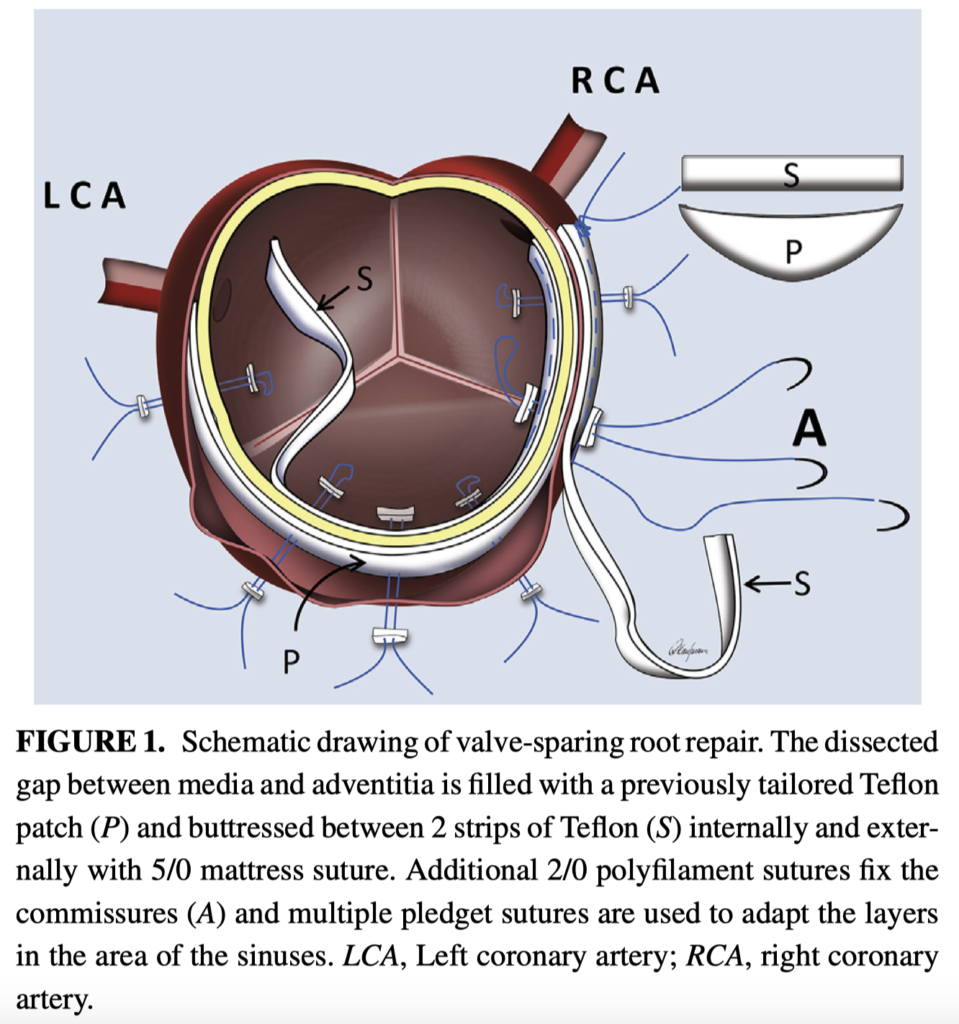
Optimal treatment of the dissected root in type A dissection is still controversial. This study of 179 patients with acute type A dissection between 1993 and 2017 found that the valve-preserving root repair technique has similar long term rates of survival and reoperation compared with root replacement techniques. It is useful as a less complex and even faster surgical technique if individually indicated.
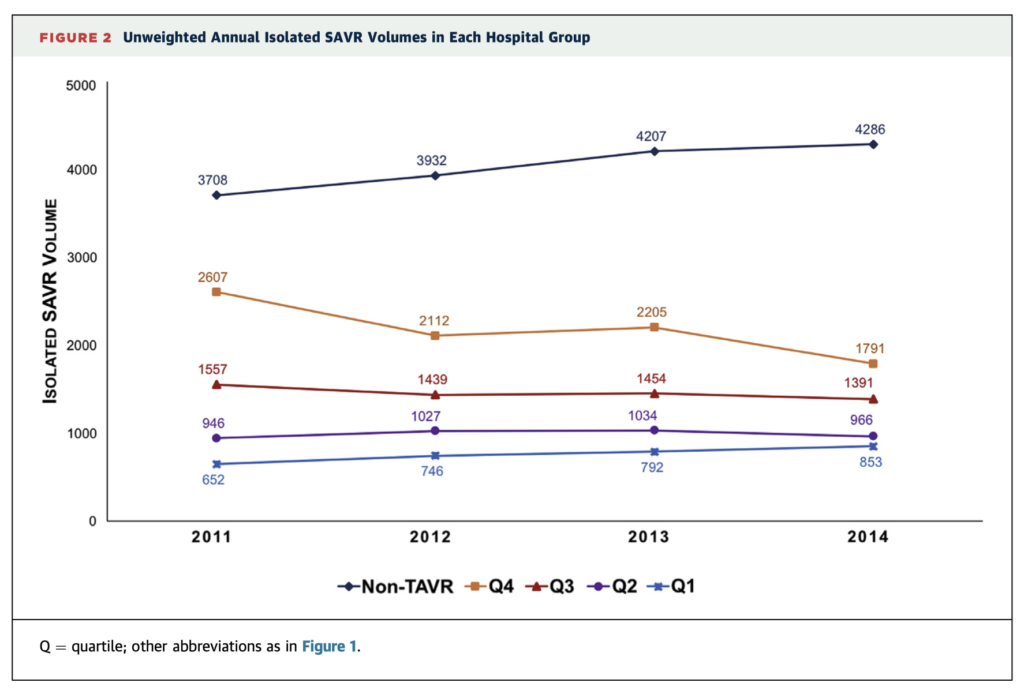
The volume of transcatheter aortic valve replacement (TAVR) has increased in the US since its approval, now exceeding that of isolated surgical aortic valve replacement (SAVR). This study of 37,705 SAVR procedures over a 4 year period found that the advent of TAVR was associated with a reduction in isolated SAVR volumes, a decrease in comorbidities among patients undergoing SAVR, and corresponding reductions in observed short and long term SAVR mortality among hospitals performing the greatest volumes of TAVRs.
Cardiac Imaging
Summarised by Dr Sarah Catchpoole
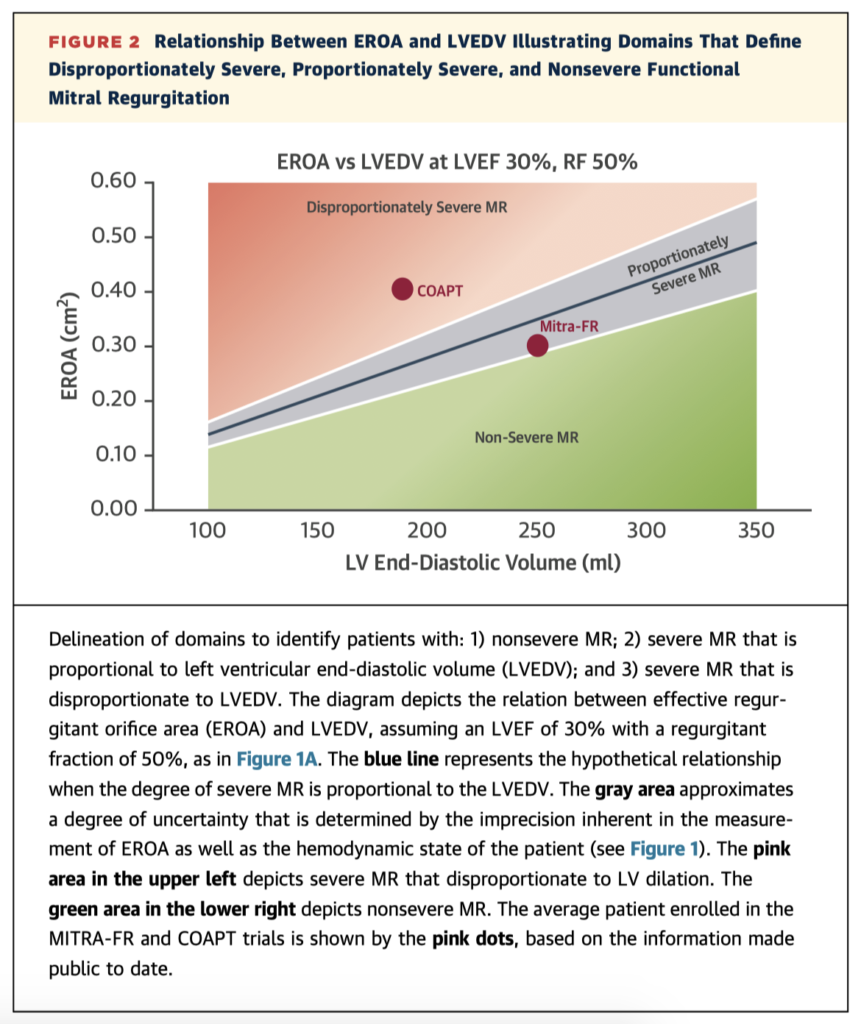
In this paper Grayburn et al. offer a way of reconciling the results of the COAPT and MITRA-FR trials. In the former trial MitraClip reduced the risk of death and hospitalization and improved LV dilatation; though in latter trial the device did not improve outcomes. They suggest functional MR can be characterised as ‘proportional’ (where the MR is entirely explained by global LV enlargement) or ‘disproportional’ (where the MR is more severe than expected from the degree of LV impairment, likely because of specific impairment of LV segments that support normal mitral valve coaption). Thus the benefit of MitraClip likely lies in treating disproportionate MR (as in COAPT), where traditional medical therapies to reduce LV volumes may not adequately reduce MR severity.
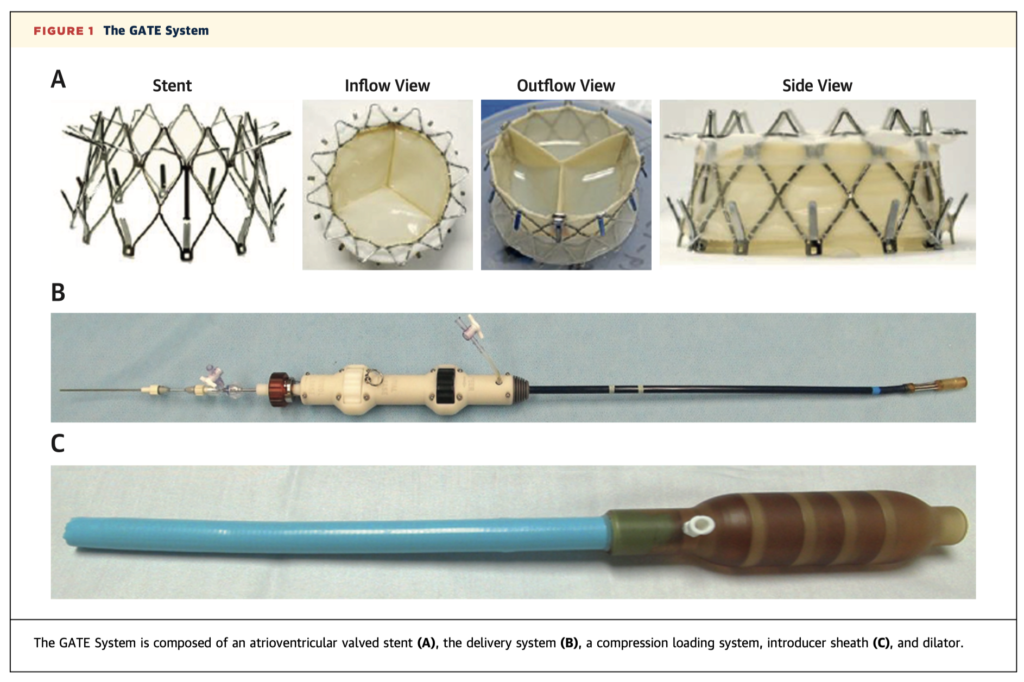
This single-site pilot trial of 5 patients undergoing first-generation transcatheter tricuspid valve replacement has shown good procedural feasibility, but mixed outcomes. While reduction in tricuspid regurgitation (TR) was excellent, the elimination of severe TR in patients with right ventricular dysfunction may be poorly tolerated, with greater RV dysfunction associated with worse clinical outcomes. There were a number of complications in the post-operative period including inotropic dependence, severe bleeding, valve thrombosis, and one death at 28 days. The authors suggest further research to determine an appropriate patient population.
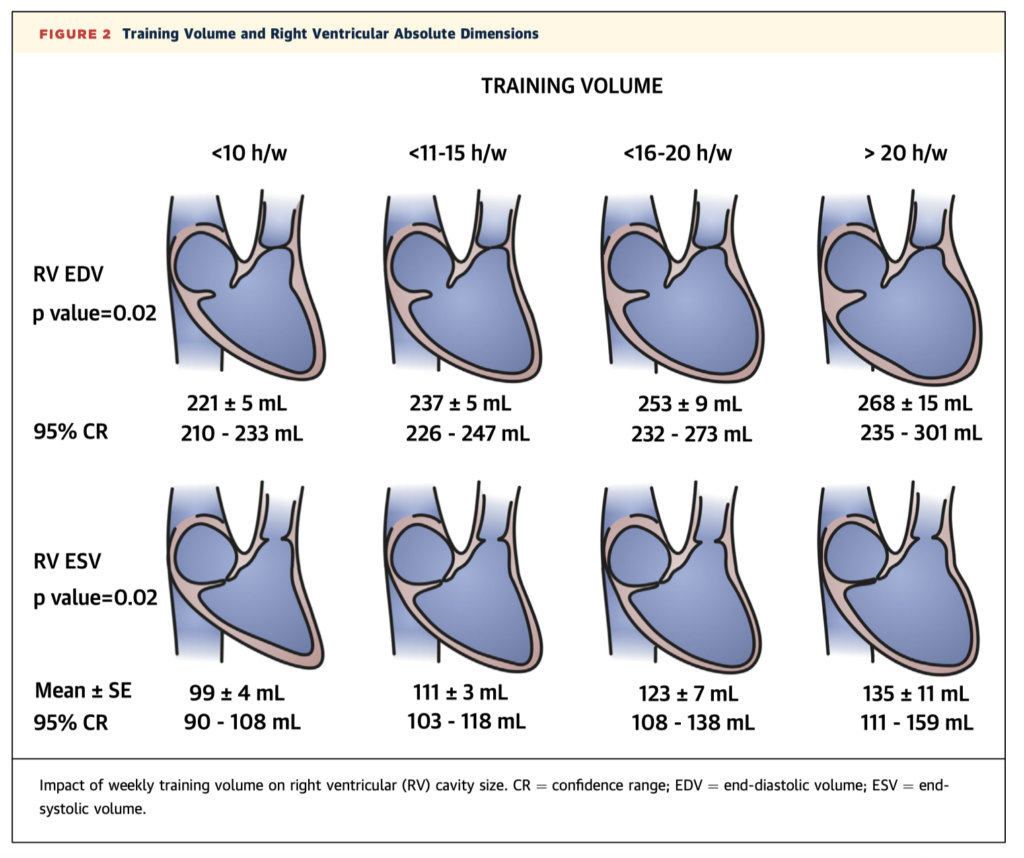
Exercise-induced structural heart changes in athletes can mimic other pathologies and there is a lack of normal reference values for this unique population. This systematic review and meta-analysis combines data from 27 studies and 983 male competitive athletes who underwent cardiac magnetic resonance imaging (CMR) to establish new normal upper limits. The authors suggest interpretation within the context of years and intensity of training, as there was a significant impact of training volume on right ventricular remodelling.
Perioperative Medicine
Summarised by Dr Andrew Haymet
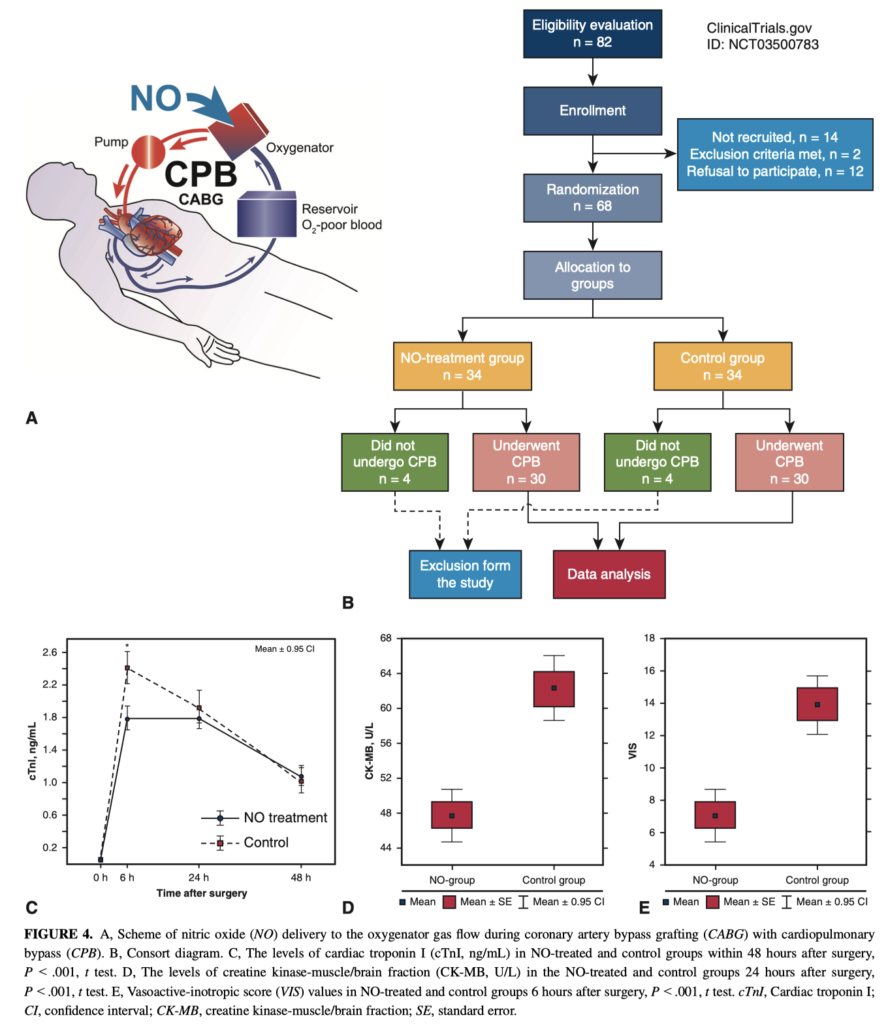
This prospective randomized study of 60 patients examined the effect of adding nitric oxide (NO) to the cardiopulmonary bypass (CPB) circuit for cardioprotection against ischaemia-reperfusion injury during coronary artery bypass grafting. Nitric oxide supply to the CPB circuit was found to be cardioprotective and associated lower levels of cardiac biomarkers and improved vasoactive inotropic score.
This paper reviews heparin induced thrombocytopenia (HIT), a rare but serious risk after cardiac surgery. Diagnosis can be difficult, if based solely on development of thrombocytopenia, because cardiac surgical patients have multiple reasons to be thrombocytopenic. Clinical assessment with laboratory evaluation should guide the diagnostic evaluation. Several clinical scoring systems have been reviewed with a diagnostic algorithm. Anticoagulation is recommended after the acute phase of HIT has resolved, commonly with a bridge of DTI’s to vitamin K antagonists.
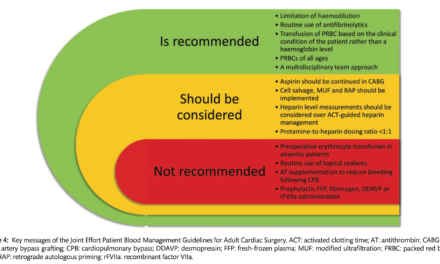
This review article describes the rationale for discontinuing dual antiplatelet therapy before cardiac surgery and its limitations, the assays available to assess pharmacodynamic effects, and the association between platelet inhibition with surgery-related bleeding. Patients at high risk may especially benefit from preoperative platelet function monitoring to both guide individualized preoperative waiting and serve as part of a transfusion algorithm aimed at targeted postcardiopulmonary bypass haemostasis management. Individualized preoperative waiting time and intraoperative transfusion management are expected to shorten length of stay and reduce costs.