Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been recently published in each speciality (Cardiology, Cardiac Surgery, Cardiac Imaging, Perioperative Medicine).
Cardiology
Summarised by Sarah Catchpoole
The prognostic value of three fraility indices were compared with the European System for Cardiac Operative Risk Evaluation II (euroSCORE II) in this prospective cohort of 188 patients (median age 71) undergoing elective (n=155) or urgent cardiac surgery (n=33). Prevalence of frailty was 31.9-51.6%, depending on the scale. Follow-up was conducted at 9-19 months post-operatively, with the primary outcome of functional survival defined as freedom from mortality with adequate health-related quality of life (>60 on the EuroQol-Visual Analogue Scale). Higher pre-operative scores on all three frailty scales were associated with 2.0-3.5 fold increased risk of poor functional survival. In addition, all three scales provided incremental prognostic value to the euroSCORE II alone.
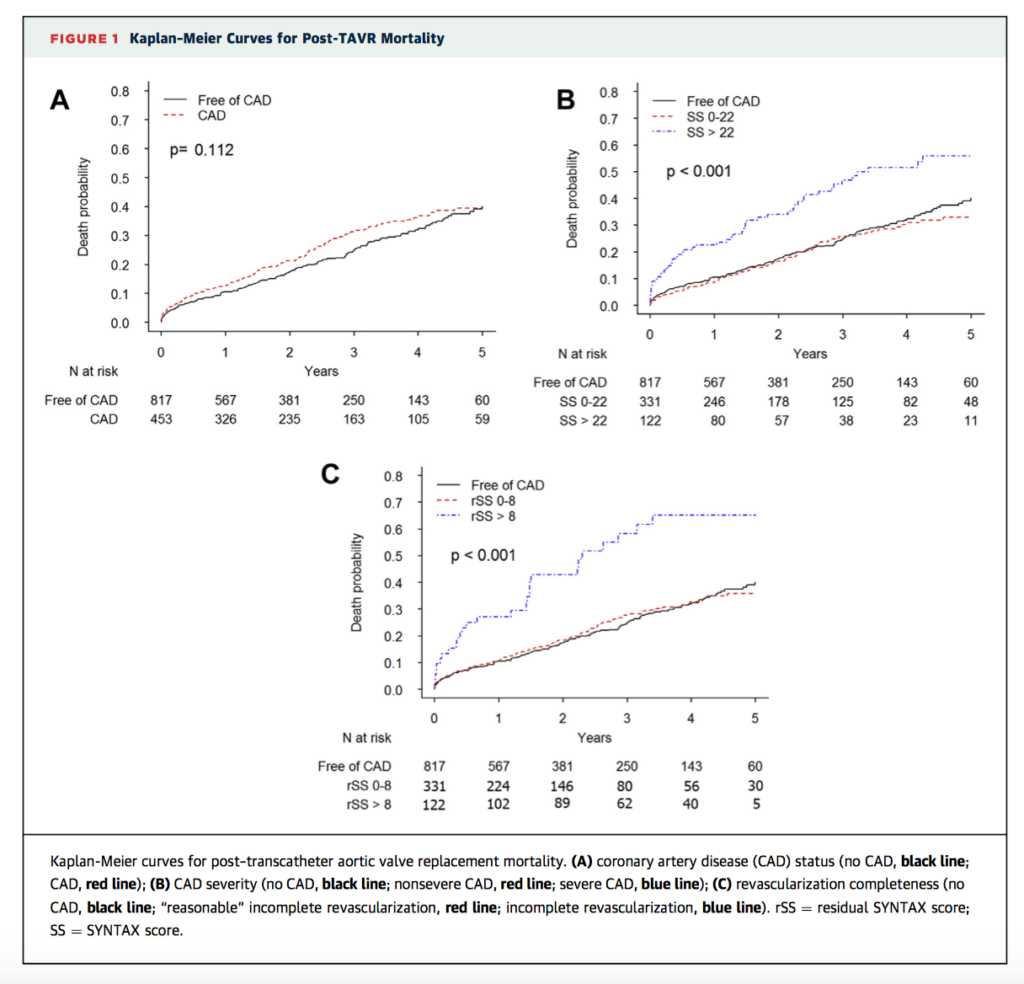
This is the first large, multicentre, retrospective observational study to examine the impact of coronary artery disease (CAD) on all-cause mortality after transcatheter aortic valve replacement (TAVR). Of the 1270 patients enrolled, 26% (n=311) had CAD and 122 (10%) had severe CAD (SYNTAX score (SS) <22), while incomplete revascularisation (ICR) was defined as residual SS >8 and “reasonable” ICR as residual SS <8. Only severe CAD and ICR were associated with increased mortality after a median follow up of 1.9 years (hazard ratio: 2.091; p<0.017 and hazard ratio: 1.720; p<0.031, respectively). If “reasonable” ICR was achieved, there was no difference in prognosis compared to patients without CAD (hazard ratio 0.749, p=0.178). The results suggest that CAD severity, rather than CAD itself predicts risk, while reasonable revascularisation can improve outcomes.
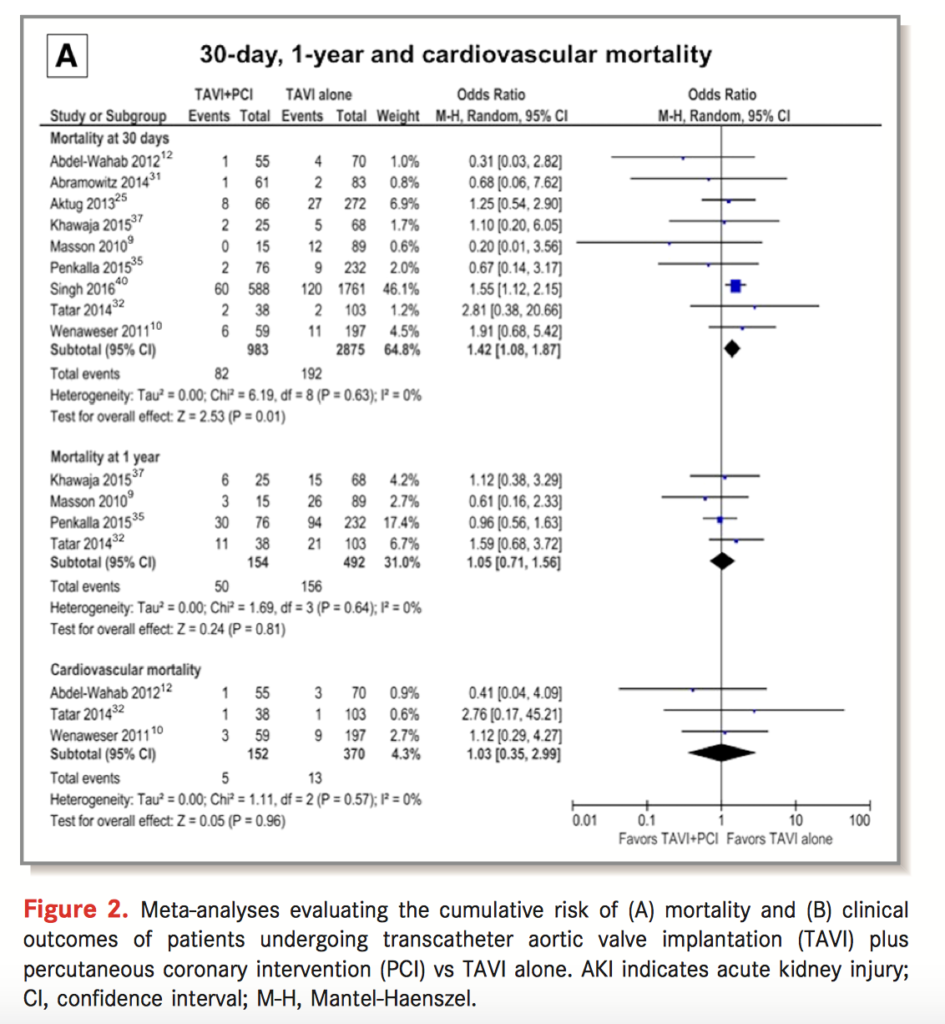
Coronary artery disease (CAD) is common in patients undergoing transcathter aortic valve replacement (TAVR), however the prognostic significance and benefit of pre-procedural intervention is uncertain. This systematic review identified 9 studies with a total of 3858 participants for inclusion in a meta-analysis. In the 983 patients that underwent revascularisation, there was no difference in 30 day cardiovascular mortality, 1 year mortality, and rates of myocardial infaction, acute kidney injury, and stroke. However, they had worse 30 day mortality (Odds ratio (OR): 1.42; P=0.01) and increased rates of major vascular complications (OR: 1.86; P=0.0003). The authors suggest there is no clear benefit of revascularisation prior to TAVR, however they note the poor quality of included studies and need for further randomised controlled trials.
Cardiac Surgery
Summarised by Andrew Haymet
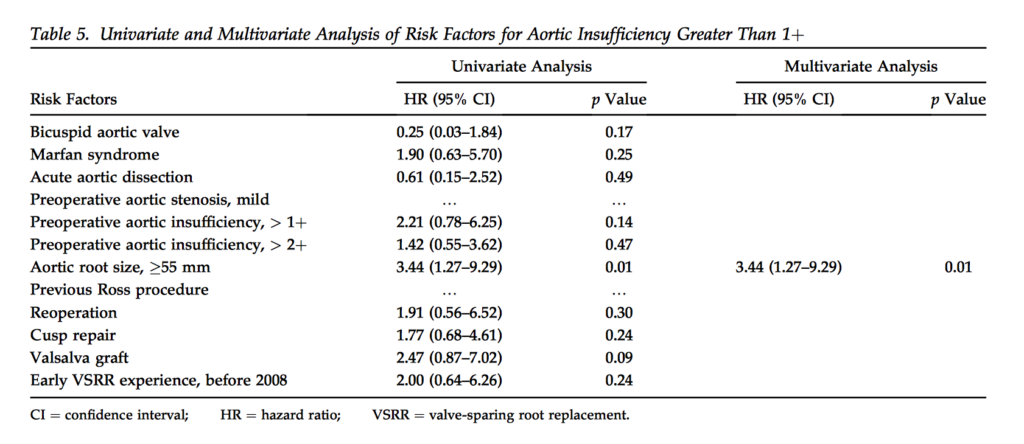
This retrospective review examined risk factors for late aortic insufficiency (AI) and aortic stenosis (AS) after David V valve sparing root replacement (VSRR). From 282 patients between 2005 to 2015 who underwent VSRR, 64 patients (22.7% had bicuspid valves) and 41 patients (14.5%) had Marfan syndrome. Operative mortality was 8 (2.8%). Seven year cumulative incidence of reoperation, greater than 2++ AI and greater than moderate AS were 3.1%, 2.2% and 0.8%, respectively. Multivariable analysis showed aortic root size 55mm or larger to be a risk factor for late AI (hazard ratio 3.44, 95% confidence interval: 1.27 to 9.29, p=0.01). Bicuspid valve and cusp repair were found to be risk factors for late AS (hazard ratio 16.07 and 5.91, 95% confidence intervals (3.12-82.68) and (1.17-29.86),p=0.001 and p=0.03 respectively]).
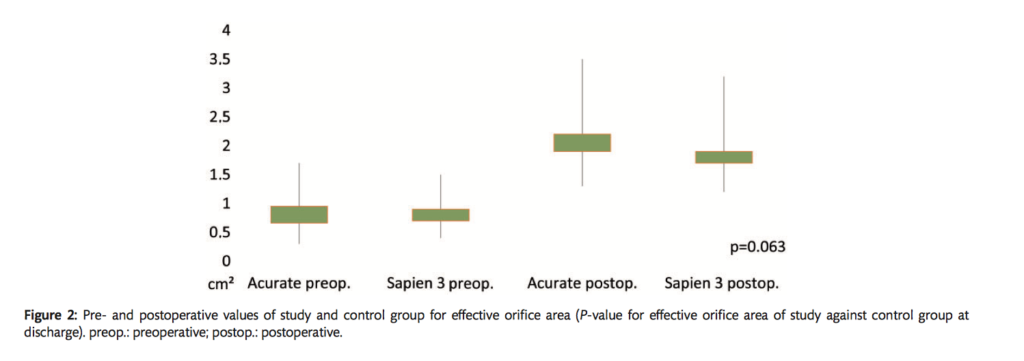
This study evaluated the 30-day outcomes of latest-generation self-expandable and balloon-expandable transcatheter heart valves in 104 patients between 2012 and 2016. The Symetis ACURATE Neo transcatheter heart valve was studied with a control group receiving the Edwards Sapien 3. Device success was 94.2% (98 of 104) and 98.1% (102 of 104) in study and control groups, respectively (P = 0.157). All-cause 30day mortality was 3.9 (4 of 104) vs 0.9% (1 of 104) (P=0.317). Resultant transvalvular peak/mean gradients and effective orifice area were 14.2 ± 5.7 vs 22.6 ± 6.8 mmHg (P < 0.001)/7.3 ± 2.8 vs 11.8 ± 3.5 mmHg (P < 0.001) and 2.0 ± 0.4 vs 1.7 ± 0.4 cm2 (P=0.063). Next generation transcatheter heart valves were found to preserve superiority in terms of post-interventional haemodynamics (eg paravalvular leakage) without presenting former drawbacks.
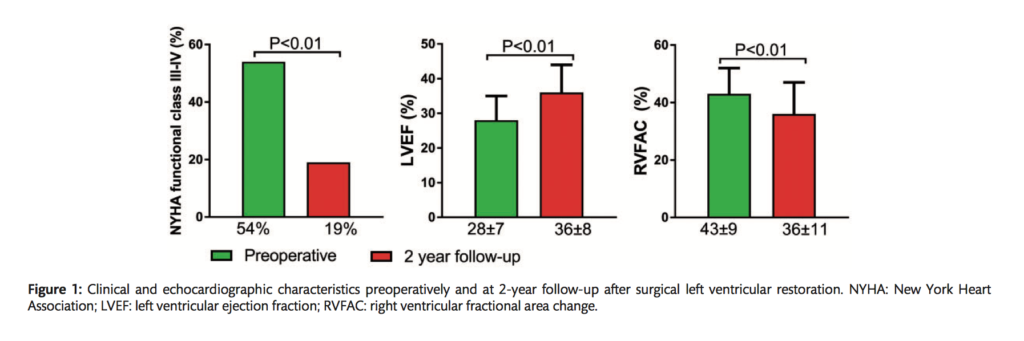
Surgical left ventricular (LV) restoration (SVR) induces changes in LV systolic and diastolic function that may affect postoperative right ventricular (RV) function. This study of 86 patients aimed to evaluate the long term effect of SVR on RV function, with specific focus on determinants and prognostic implications of RV dysfunction. RV dysfunction at follow-up was present in 40% of patients and was associated with worse preoperative RV fractional area change (39 ± 9 vs 46 ± 7%, P< 0.01), pulmonary hypertension (18 vs 4%, P= 0.03) and higher follow-up LV filling pressures (E/E’ ratio23±8 vs 15±8, P=0.02). Patients with RV dysfunction were more frequently in New York Heart Association Class III or IV (30 vs 12%, P=0.04)and 5-year mortality, heart transplantation and LV assist device implantation rate was increased (49 vs 17%, P< 0.01) as compared to patients with normal RV function. Patients with RV dysfunction after SVR had worse clinical functioning and outcome as compared to patients with normal RV functioning.
Cardiac Imaging
Summarised by Sarah Catchpoole
In patients with asymptomatic aortic stenosis (AS), changes in blood pressure changes or development of symptoms on exercise testing are well-known indications for valve replacement. However, the role of echocardiographic parameters is uncertain. In this single-centre observational study, 148 patients with mild to moderate isolated AS who underwent exercise-stress echocardiography were followed up for a median of 14±8 months. Measures of AS severity at rest (mean pressure gradient (MPG), peak velocity, and aortic valve area) were prognostic for progression to aortic valve replacement and AS related events (p<0.0001). However, there was no association found for peak systolic pulmonary artery pressure (SPAP) and MPG values at peak exercise.
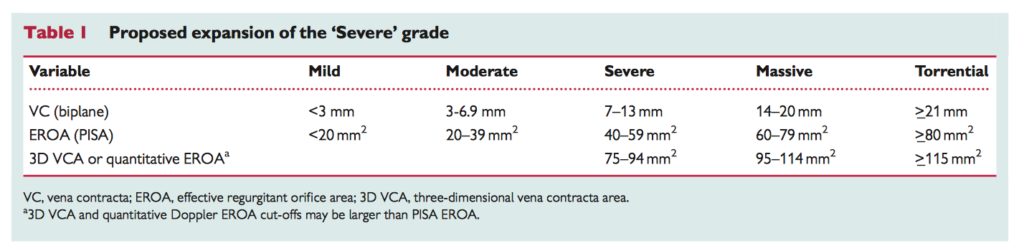
Contemporary feasibility trials of transcutaneous tricuspid valve devices have revealed that current definitions of “severe” tricuspid regurgitation (TR) do not adequately capture the severity of end-stage disease in the patients enrolled. Nor can current grade boundaries capture the post-intervention improvements in TR measures and quality of life that are likely to have some prognostic benefit. Consequently, Hahn and Zamorano have proposed the expansion of the “severe” TR grade to include “massive” and “torrential” categories. In addition, they hope a new grading system would facilitate better trial design and monitoring of long-term differences in outcomes.
Transoesophageal echocardiography (TOE) is the current gold standard for diagnosis of infective endocarditis (IE). However, have advances in harmonic imaging and probe technology improved the sensitivity and specificity of less-invasive, cheaper transthoracic echocardiography (TTE)? In this meta-analysis of 16 studies and a total of 2807 patients (n=793 with IE vegetations), the authors found harmonic TTE can detect vegetations with a sensitivity of 61%, specificity of 94%, and negative likelihood ratio (NLR) of 0.42. While NLR was improved in patients without prosthetic valves (NLR = 0.36) or in the setting of conclusively negative results (NLR = 0.17), the authors conclude that TTE nevertheless may miss many vegetations, with subsequent TOE inevitably required.
Perioperative Medicine
Summarised by Andrew Haymet
Lomivorotov, V.V. et al. Low-Cardiac-Output Syndrome After Cardiac Surgery JCTVA 2017 Feb.
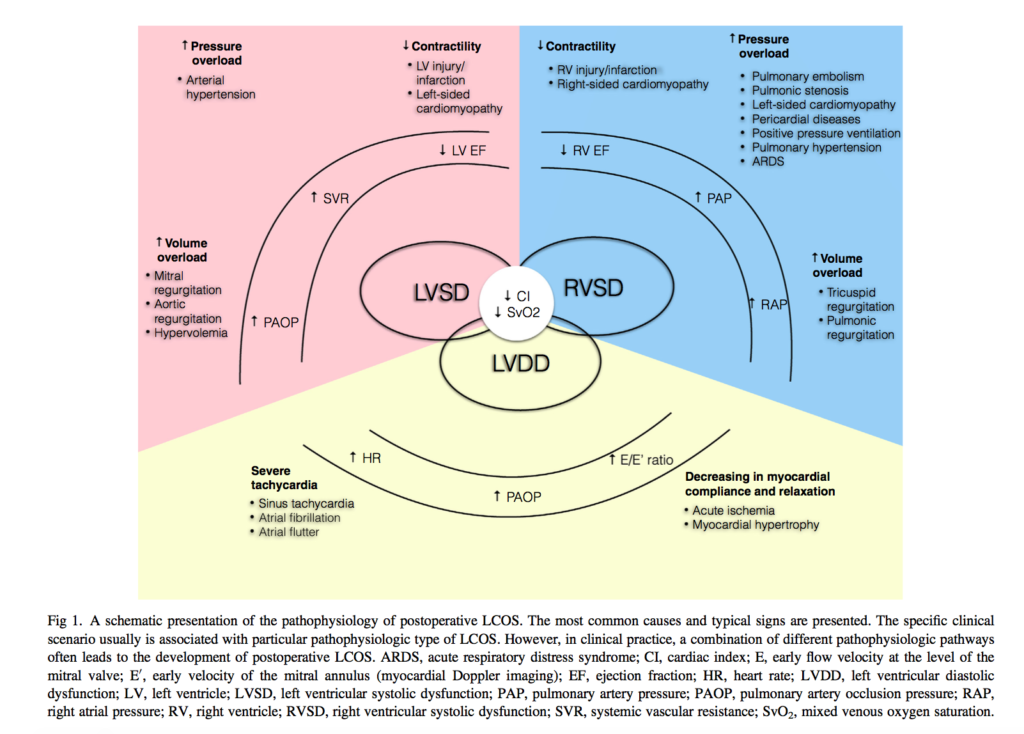
Over the past decade, there has been a significant decline in cardiac surgery-associated mortality, despite an increase in the complexity of operations. The low cardiac output syndrome (LCOS) remains the most common complication, characterized by decreased heart pump function, leading to reduced oxygen delivery (DO2 ) and subsequent tissue hypoxia. The most common definition of LCOS decreases in the cardiac index (CI) to <2.0 L/min/m2 and a systolic blood pressure of <90 mmHg, in conjunction with signs of tissue hypoperfusion in the absence of hypovolemia. Inotropes or mechanical support are invariably required. Acute renal failure, neurologic and pulmonary complications, as well as atrial fibrillation, are common sequelae of LCOS, and mortality may exceed 20%. Prompt identification of LCOS is necessary to instigate goal directed therapy to maximize DO2 and to restore organ perfusion and function.
Digoxin is widely used in patients with atrial fibrillation despite the lack of randomized controlled trials. In the ENGAGE AF-TIMI 48 trial, 21,105 patients were enrolled with 6327 (30%) were treated with digoxin at baseline. Among patients without HF (n=8981), digoxin use (20%) was independently associated with sudden cardiac death (adjusted hazard ratio, 1.51; 95% CI, 1.10–2.08), with no significant interaction by age, sex, left ventricular ejection fraction, renal function, or concomitant medications (P>0.05 for each). Among patients with HF (n=12 124), digoxin use (37%) was associated with an increase in all-cause death, cardiovascular death, sudden cardiac death, and death caused by HF/cardiogenic shock (P<0.01 for each), but not with noncardiovascular death, stroke/systemic embolism, or myocardial infarction. Whilst residual confounding cannot be excluded, the association between digoxin usage and worse clinical outcomes warrants further investigation.
This multicentre, double blind, cluster-randomized, double-crossover study and prospective nested single centre study compared the effect of Plasma-Lyte 148 (PL-148) with 0.9% saline on blood product use and postoperative bleeding admitted to the intensive care unit following cardiac surgery. 128 of 475 patients (26.9%) in the PL-148 group received blood or a blood product compared with 94 of 479 patients (19.6%) in the saline group (OR [95% confidence interval], 1.51 [1.11-2.05]; p = 0.008). There were no differences between groups in chest drain output from the time of arrival in the ICU until 12 hours postoperatively (geometric mean, 566 mL for the PL-148 group v 547 mL in the saline group; p = 0.60). The hypothesis that using PL-148 for fluid therapy in ICU reduces transfusion requirements post cardiac surgery was not supported by these findings.