Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been recently published in each speciality (Cardiology, Cardiac Surgery, Cardiac Imaging, Perioperative Medicine).
Cardiology
Summarised by Dr Sarah Catchpoole
In this clinical trial 4,744 patients with heart failure (LVEF ≤40% and NYHA II-IV) were randomised to dapagliflozin 10mg daily or placebo. There was a significant difference in the primary composite outcome of worsening heart failure (hospitalization or an urgent visit resulting in intravenous therapy for heart failure) or cardiovascular death (16.3% for the dapagliflozin group vs. 21.2% for the placebo group, p<0.001). Of note, there was no significant difference between patients with and without diabetes, and the overall rate of adverse events did not differ between groups. The authors recommend consideration of the therapeutic role of dapagliflozin beyond the cohort of patients with diabetes.
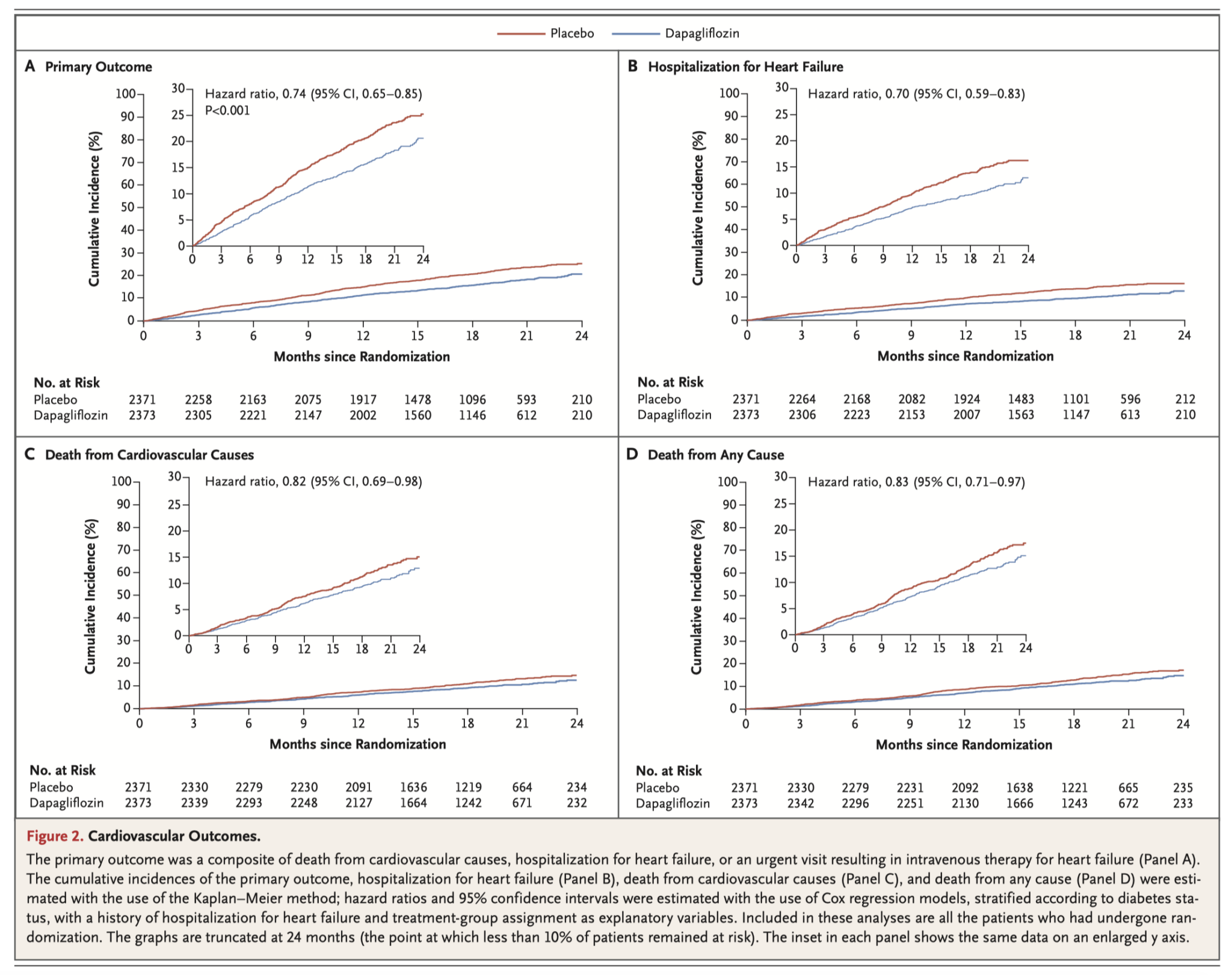
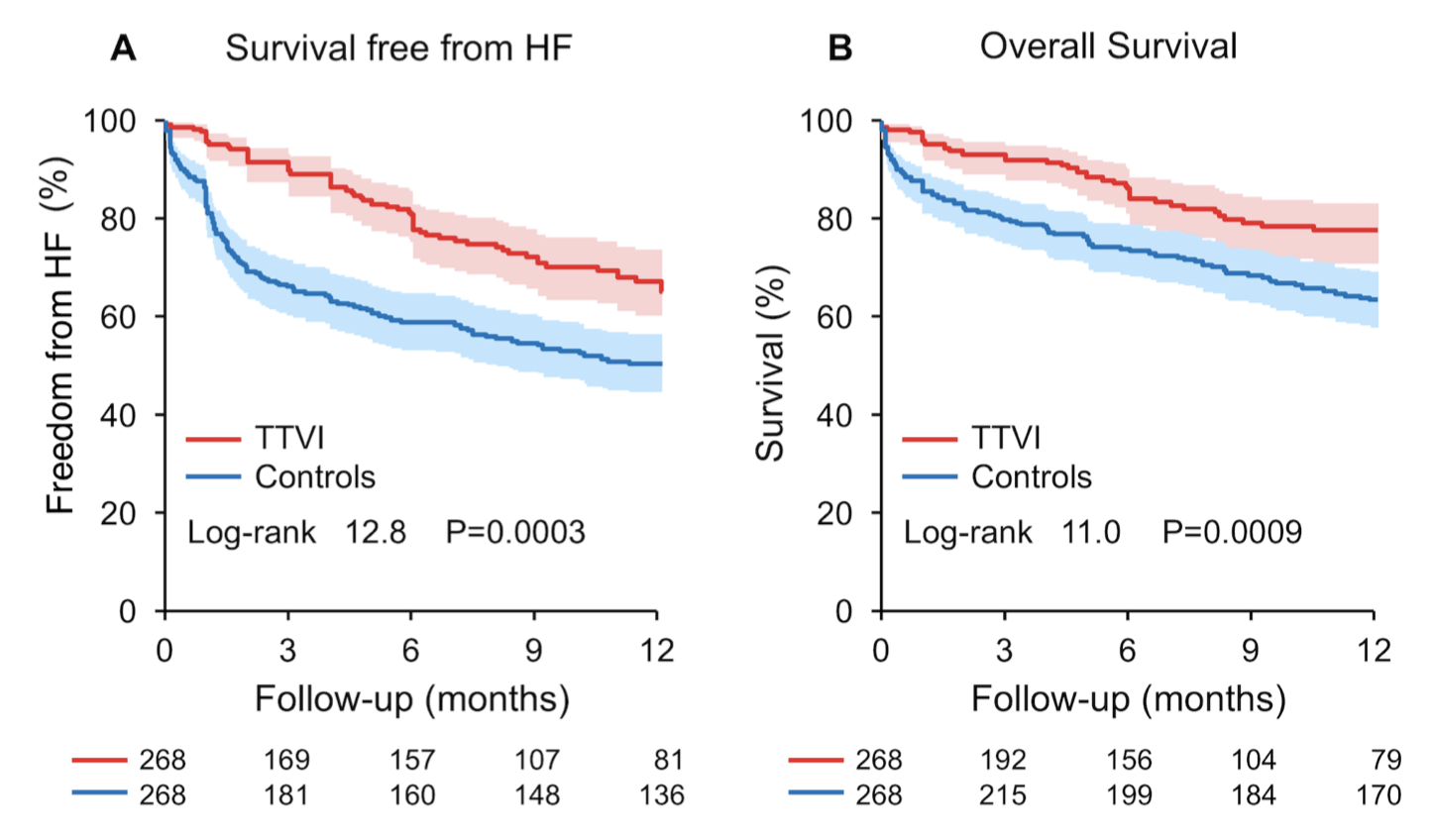
This study compared patients who had undergone transcatheter tricuspid valve interventions (TTVI; from the TriValve registry, n=472) to medical therapy (from a separate registry, n=1179). The cohorts were propensity-matched using age, EuroSCORE II, and systolic pulmonary artery pressure. There were 268 matched pairs.. At one year, the TTVI patients had lower rates of rehospitalisation (26 ± 3% vs 47 ± 3% p<0.0001) and mortality (23 ± 3% vs 36 ±3 %, p=0.001). Furthermore, there was also a significant improvement in mortality observed with procedural success. Overall this study represents encouraging results of the potential benefit of TTVI, however prospective randomised trials are needed.
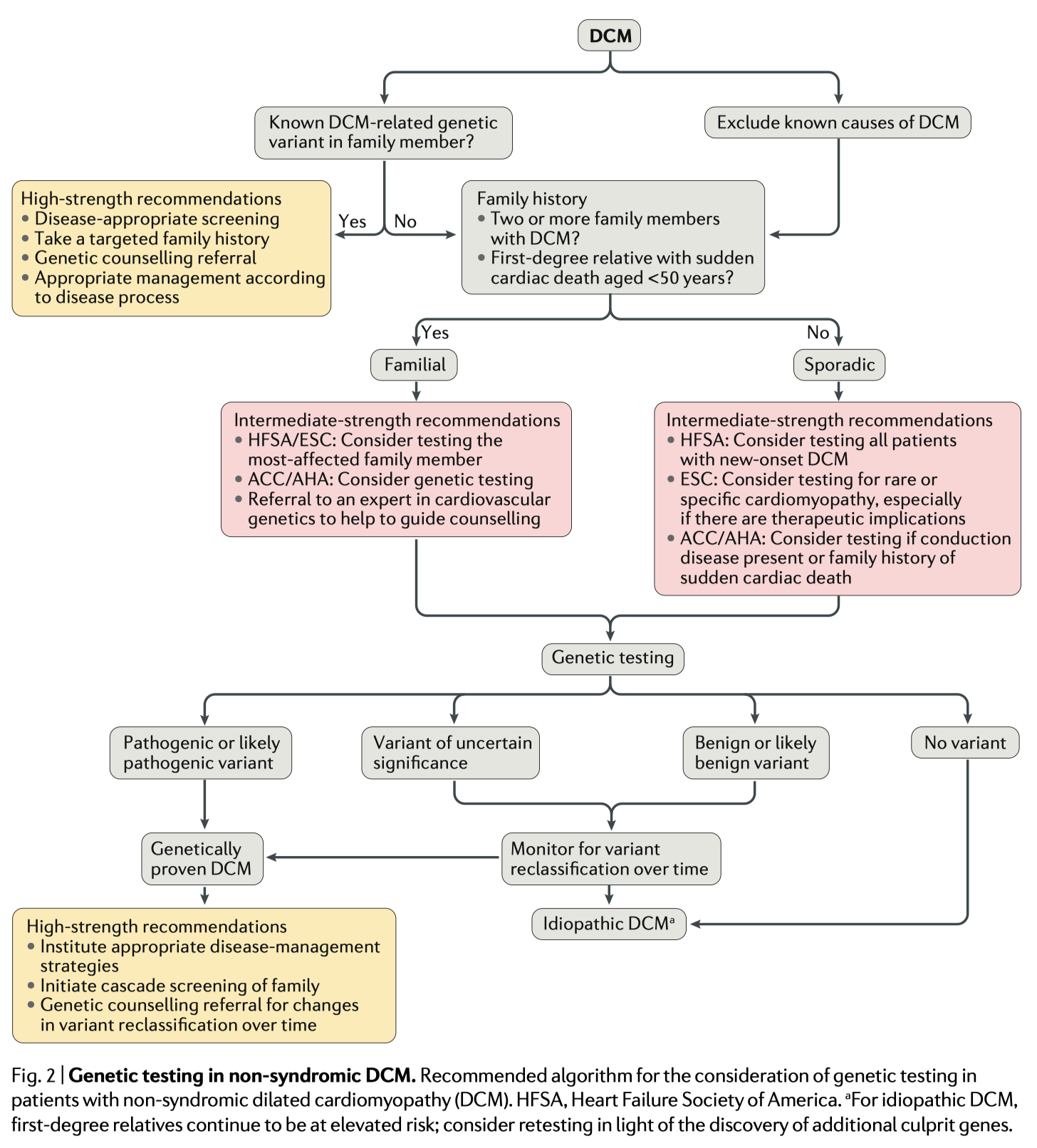
This review offers clinicians a focused, evidence-based resource on genetic testing in patients presenting with newly diagnosed dilated cardiomyopathy (DCM). The authors provide a broad summary of the most common DCM associated variants and compare and contrast current guidelines. The yield of genetic testing is approximately 20-40% in patients with familial DCM, and 15-25% in cases of sporadic DCM, with important prognostic and therapeutic implications. However, the authors acknowledge there remain many practical challenges in this area. Firstly, advances in genetics are being offset by an increasing understanding of the variability of gene and disease expression. Secondly, broader genetic testing yields a high number of variants of uncertain significance. Compounding these issues, the availability of genetic counselling remains limited.
Cardiac Surgery
Summarised by Dr David Bell
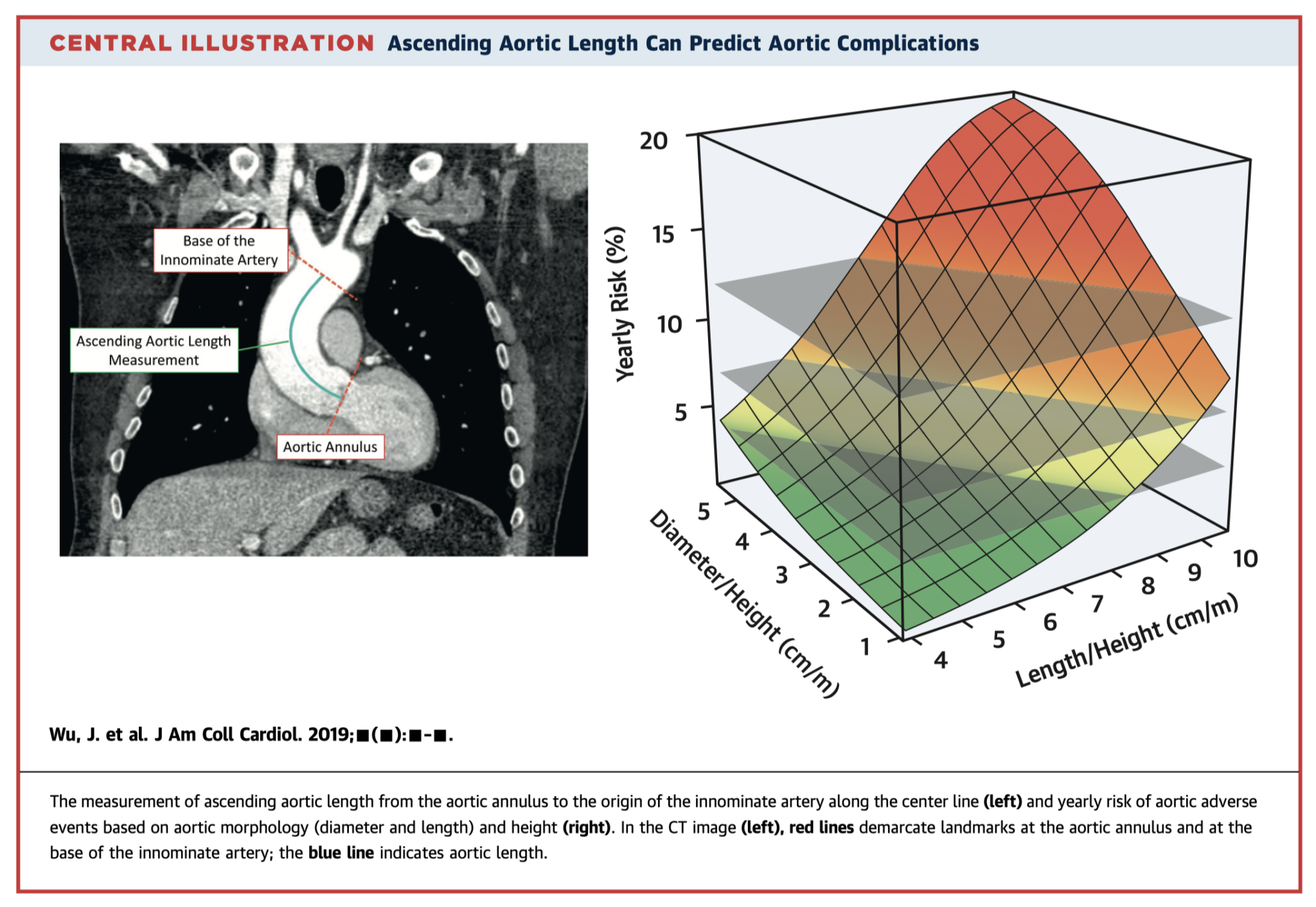
This retrospective, observational study of 522 patients sought to outline the relationship between Ascending Aortic Length (AAL; see figure), and adverse aortic events (AAE). The authors found an AAL of > 13cm was associated with a five-fold greater increase of AAEs, and that two ‘hinge’ points at aortic lengths of 11cm and 12cm saw sharp rises in the risk of AAEs. The paper concludes with a recommendation that an AAL of >11cm serves as a potential intervention criterion.
The paper did not address the fact that as aortic diameter increases (particularly if it does so asymmetrically), the height of the aorta (as defined by the blue line in the image) bends rightward and will therefore often increase in concordance. To best understand whether AAL is indeed a useful metric we would need to know how many patients with AAL >11cm who did not fit traditional intervention criteria suffered AAE. This paper presents yet another ‘one size fits all’ criterion for aortic intervention. The holy grail of predictive intervention for aortic disease likely lies in matching large sets of imaging and matched outcome data and utilising a deep learning approach.
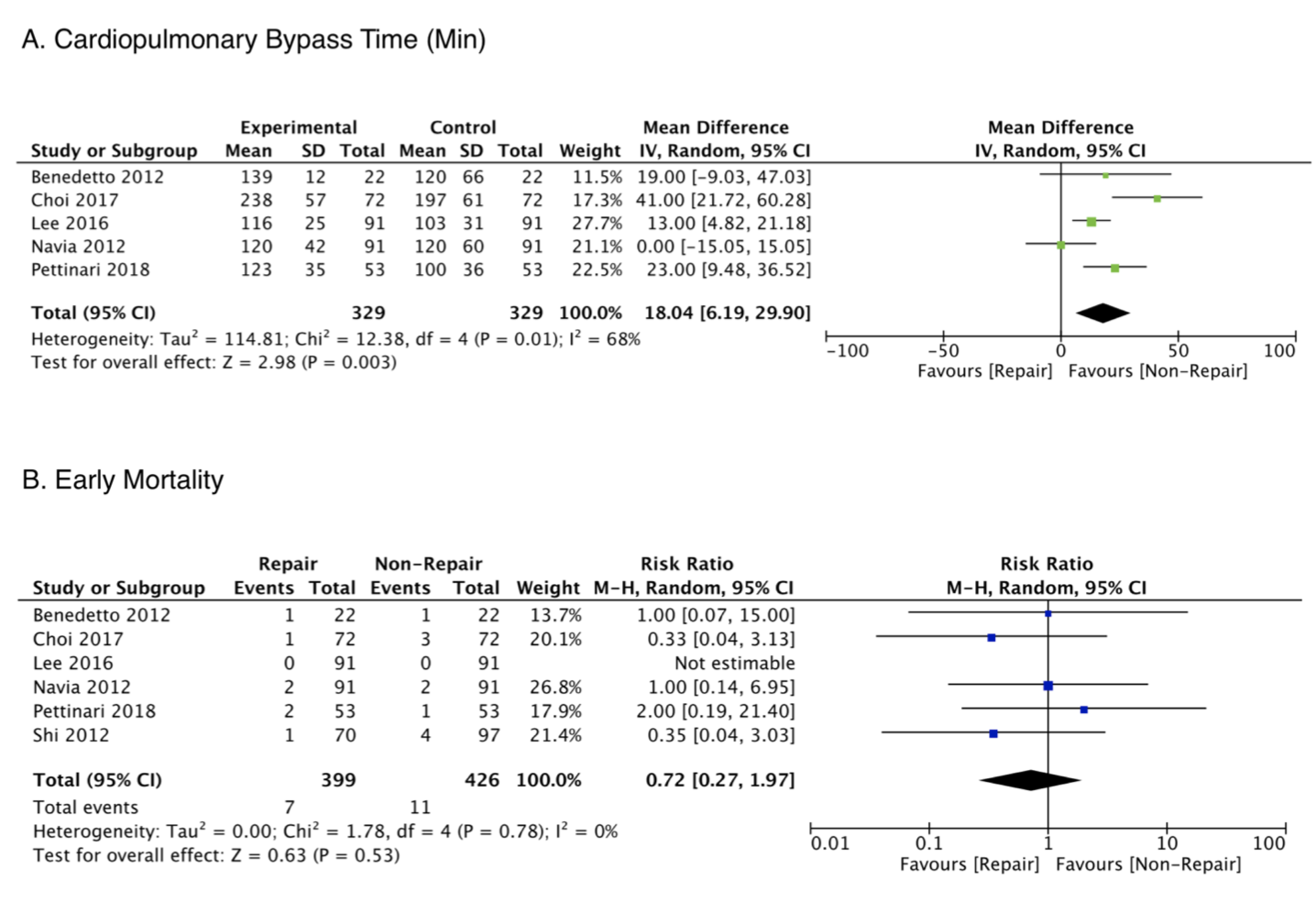
This systematic review lays out a strong case for repair of mild-moderate TR for patients undergoing concomitant left sided valve surgery. 399 repair and 426 non-repair patients from six studies were analysed and showed that repair of mild-moderate TR was associated with reduced risks of cardiovascular mortality, all-cause mortality and progression of tricuspid regurgitation over a median of 5.3 years follow up.
One limitation of the study is that it doesn’t analyse patients with mild and moderate TR separately. Furthermore, it is difficult to conclude that cohorts are well matched simply based of a few neatly defined parameters. Therefore, ongoing studies with prospectively defined inclusion criteria are required to further evaluate evidence-driven recommendations for concurrent tricuspid repair.
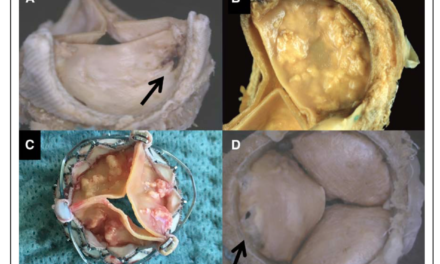
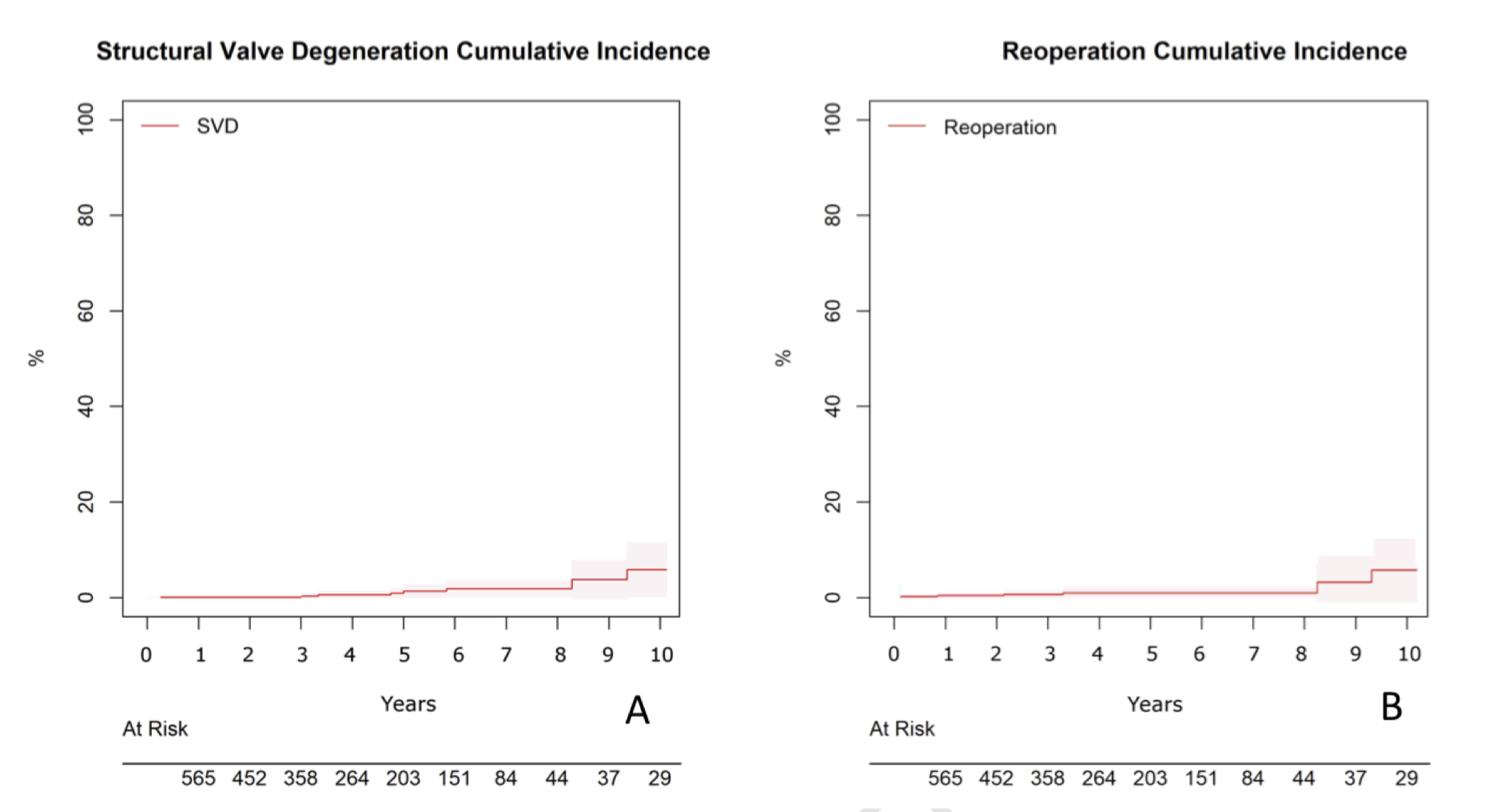
This study is a retrospective review of mitral valve replacement with the Mosaic valve. The early mortality rates were high, with the 30-day mortality found to be 7.8% (n=63), with 4.5% mortality in the elective cases. At 10 years, overall survival was 57.4% (95%CI 48.8% – 67.5%), and cumulative rates of cardiac- and valve-related death were 7.4% (95%CI 4.8% – 10.1%) and 1.1% (95%CI 0.2% – 1.9%). 10-year cumulative incidence of structural valve degeneration and reoperations were 5.8% (95% CI 0.2% – 11.5%) and 4.8% (95%CI 0.7% – 10.3%), respectively. However, the median follow-up was only 44 months (IQR range 16 – 63) with very few patients followed up past 10 years.
Cardiac Imaging
Summarised by Dr David Bell
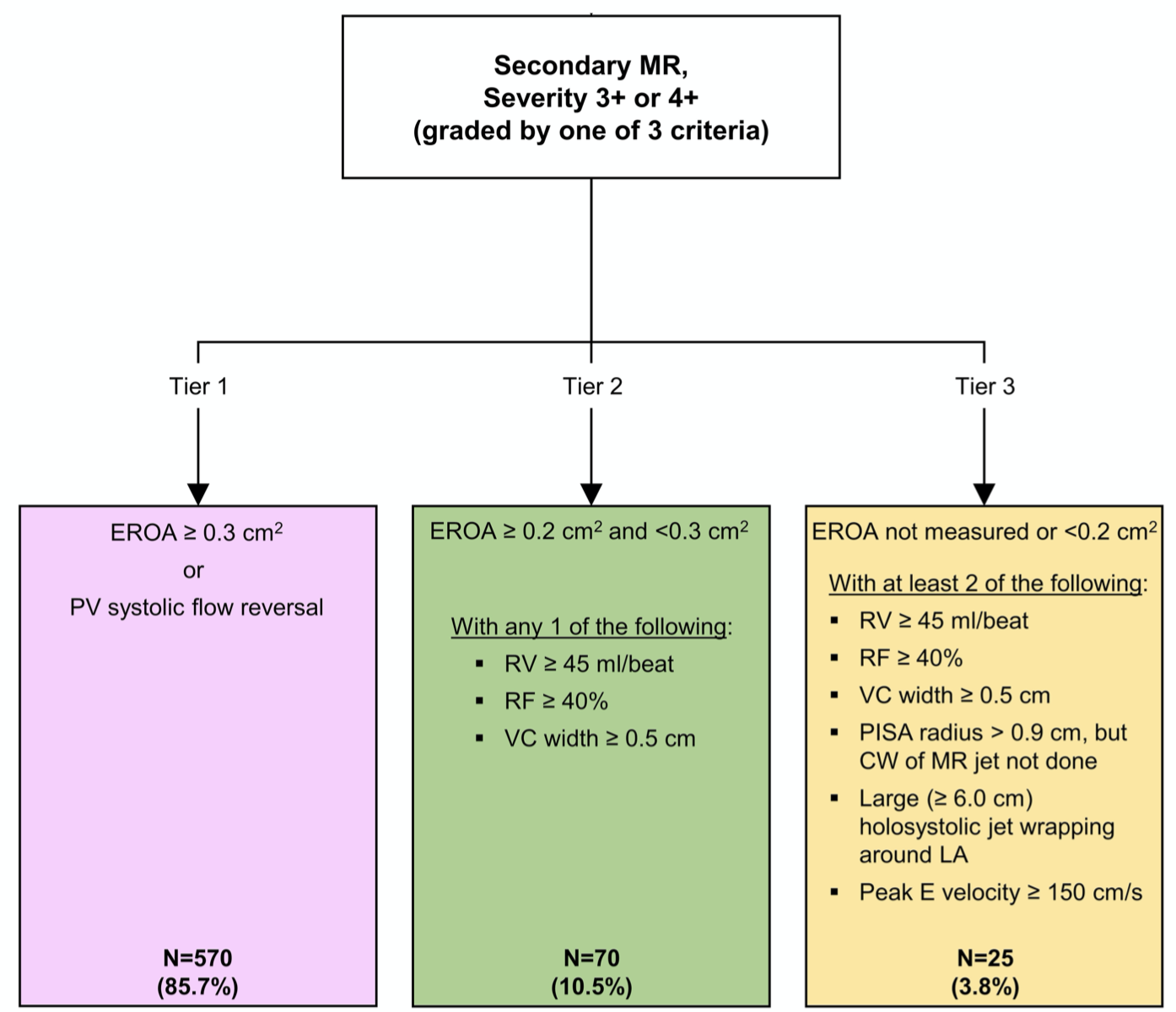
In the COAPT RCT, treatment of patients with heart failure secondary to severe mitral regurgitation (MR) with transcatheter mitral valve replacement (TMVR) was shown to improve rates of hospitalisation and mortality. However, as the shape of the MR regurgitant orifice in secondary MR (SMR) is elliptical rather than circular, the use of classic MR parameters such as proximal isovelocity surface area or vena contracta can be problematic in MR evaluation and patient selection. Furthermore, evaluating SMR severity after TMVR is especially challenging. To address these issues the COAPT investigators developed a set of objective, quantitative criteria to identify candidate patients for TMVR and evaluate them post operatively. Based on this model no groups of non-responders were identified. Adherence to these criteria is essential if the COAPT results are to be duplicated in clinical practice.
Patient selection for transcatheter edge-to-edge mitral valve repair remains challenging because of variability across patients in both mitral valve anatomy and pathology. This study sought to identify both the anatomical and quantitative features associated with optimal MR reduction (defined as less than moderate residual MR) based on quantitative 3D transesophageal echocardiography. Of the 59 patients in the study, 35 had primary MR and 24 had mixed or secondary MR. Optimal MR reduction was achieved in 40 of 59 patients (68%). In primary MR, reduced leaflet tenting was associated with optimal MR reduction and in functional MR, reduced annular height was associated with optimal MR reduction.
This small, single unit retrospective study (296 TAVR patients) sought to investigate the role basal septal hypertrophy (BSH) had on procedural and post procedural outcomes. BSH is a common finding in patients undergoing TAVR and has been postulated to be associated with complications after TAVR. This study showed that in their cohort patients with BSH patients received post-dilation more frequently (BSH+ vs BSH−: 41.8% vs 29.9%, P = .04) but there was no difference in rates of post-operative conduction disturbance between patients with and without BSH.
Perioperative Medicine
Summarised by Dr Andrew Haymet
This is the latest guideline on the conduct and management of cardiopulmonary bypass (CPB) in adult patients undergoing cardiac surgery, with a focus on summarizing the scientific rationale for various technical aspects of CPB. Topics covered include an overview of heart-lung hardware and consumables, preparation for and procedures conducted during CPB, and separation from CPB.
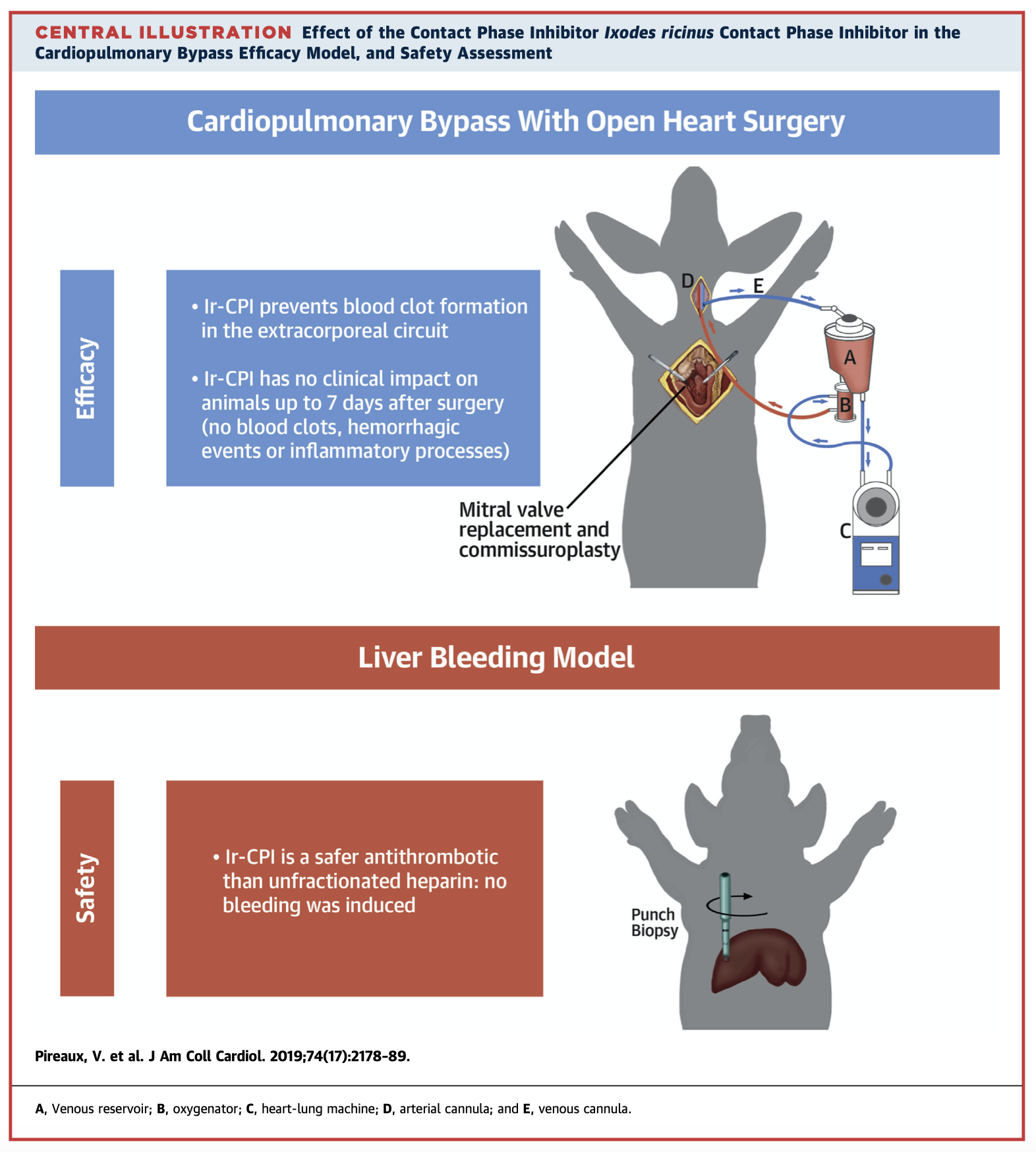
Anticoagulation is necessary in artificial circuits, such as cardiopulmonary bypass, where the contact of blood induces a procoagulant state. Unfractionated heparin (UFH) is frequently used but can be associated with life threatening bleeding or hypercoagulable states. This preclinical animal study aimed to assess the antithrombotic activity of Ic-CPI, a protein expressed by I. ricinus ticks which inhibits factors XIIa and XIa. This study found Ir-CPI to be an effective and safe antithrombotic agent which is clinically applicable to bypass systems, including CPB.
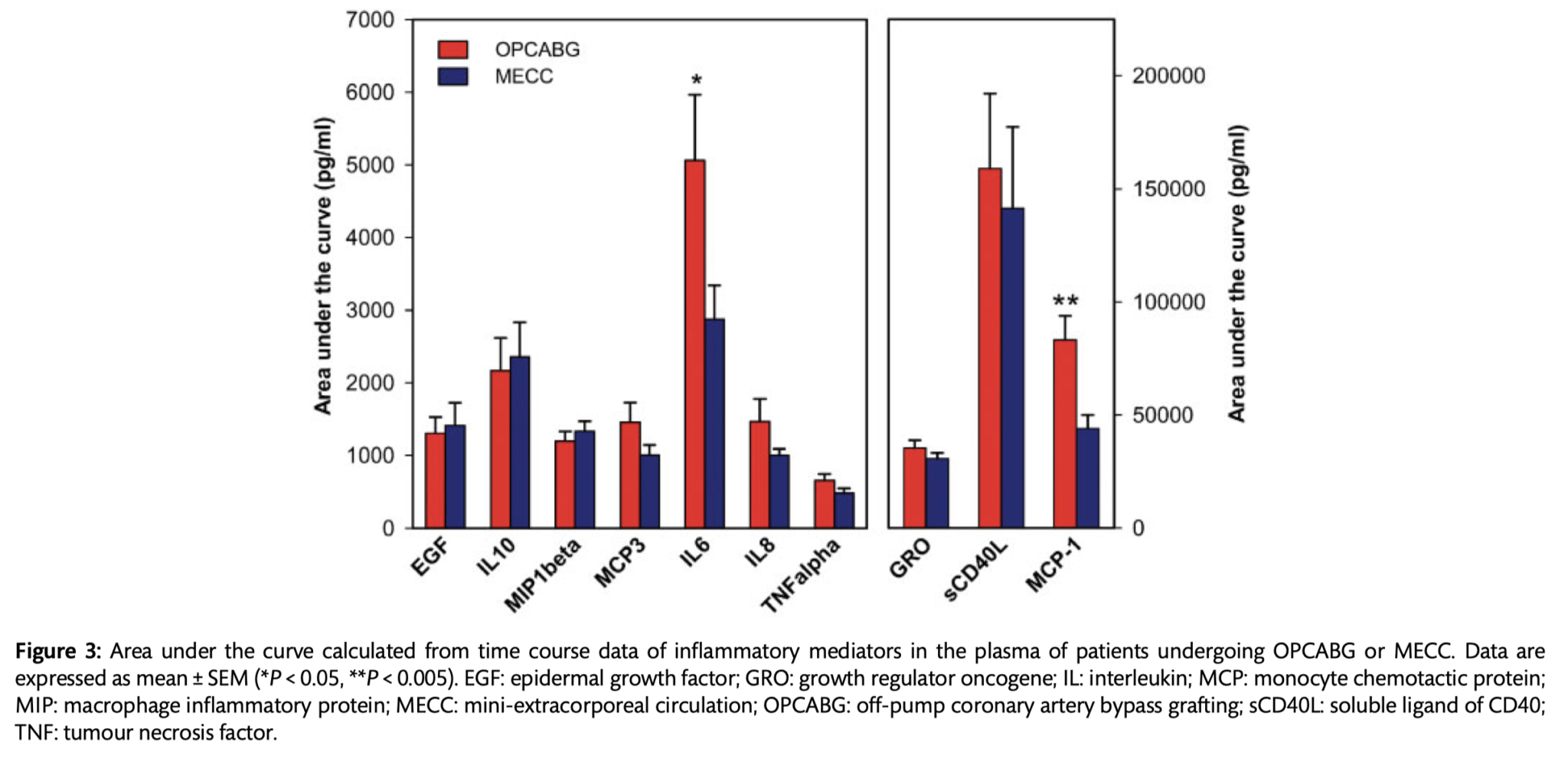
Both off-pump coronary artery bypass graft surgery (OPCABG) and mini-extracorporeal circulation (MECC) have been associated with lower mortality, morbidity, and inflammation than surgery on cardiopulmonary bypass (CPB). This prospective, randomized study of 230 low-risk patients undergoing coronary bypass surgery aimed to compare circulating inflammatory markers in an OPCABG cohort compared to a MECC cohort. No significant clinical differences were found in low-risk patients undergoing either type of surgery, however the OPCABG cohort demonstrated higher release of proinflammatory cytokines.