Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been recently published in each speciality (Cardiology, Cardiac Surgery, Cardiac Imaging, Perioperative Medicine).
Summarised by Dr Sarah Catchpoole
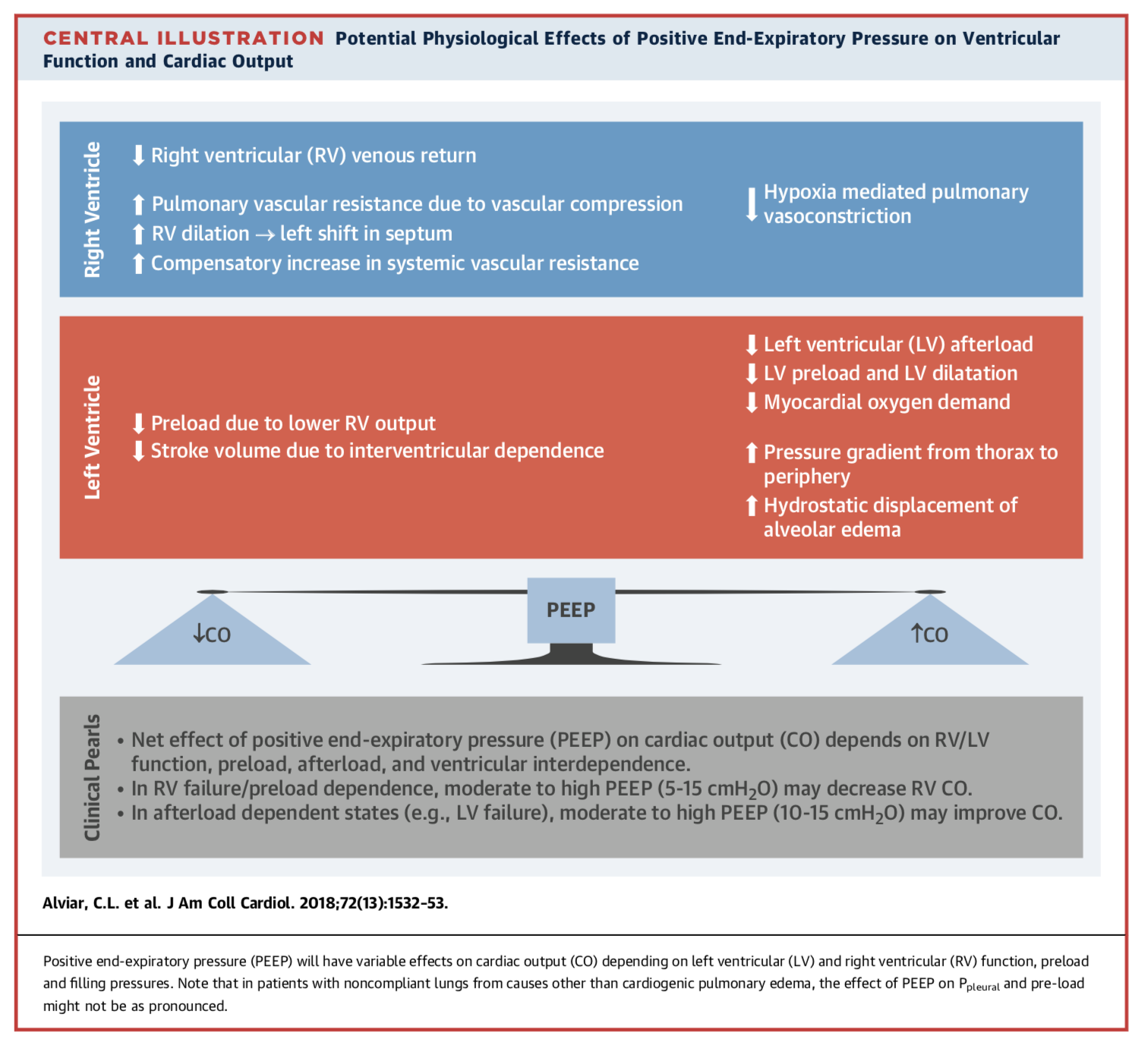
Understanding the cardiovascular effects of positive pressure ventilation (PPV) is essential for clinicians working in cardiac intensive care units. This excellent review article begins with an in-depth discussion of the physiology and pulmonary mechanics of PPV, followed by modes of delivery and management of ventilator settings, specific indications including cardiogenic pulmonary oedema, and finally complications and principles of weaning. Topics of note include precautions using PPV in the setting of preload dependent states such as RV failure and tamponade, and a useful summary table of the cardiac effects of drugs used in conjunction with PPV including sedatives, neuromuscular blockers, and analgesics.
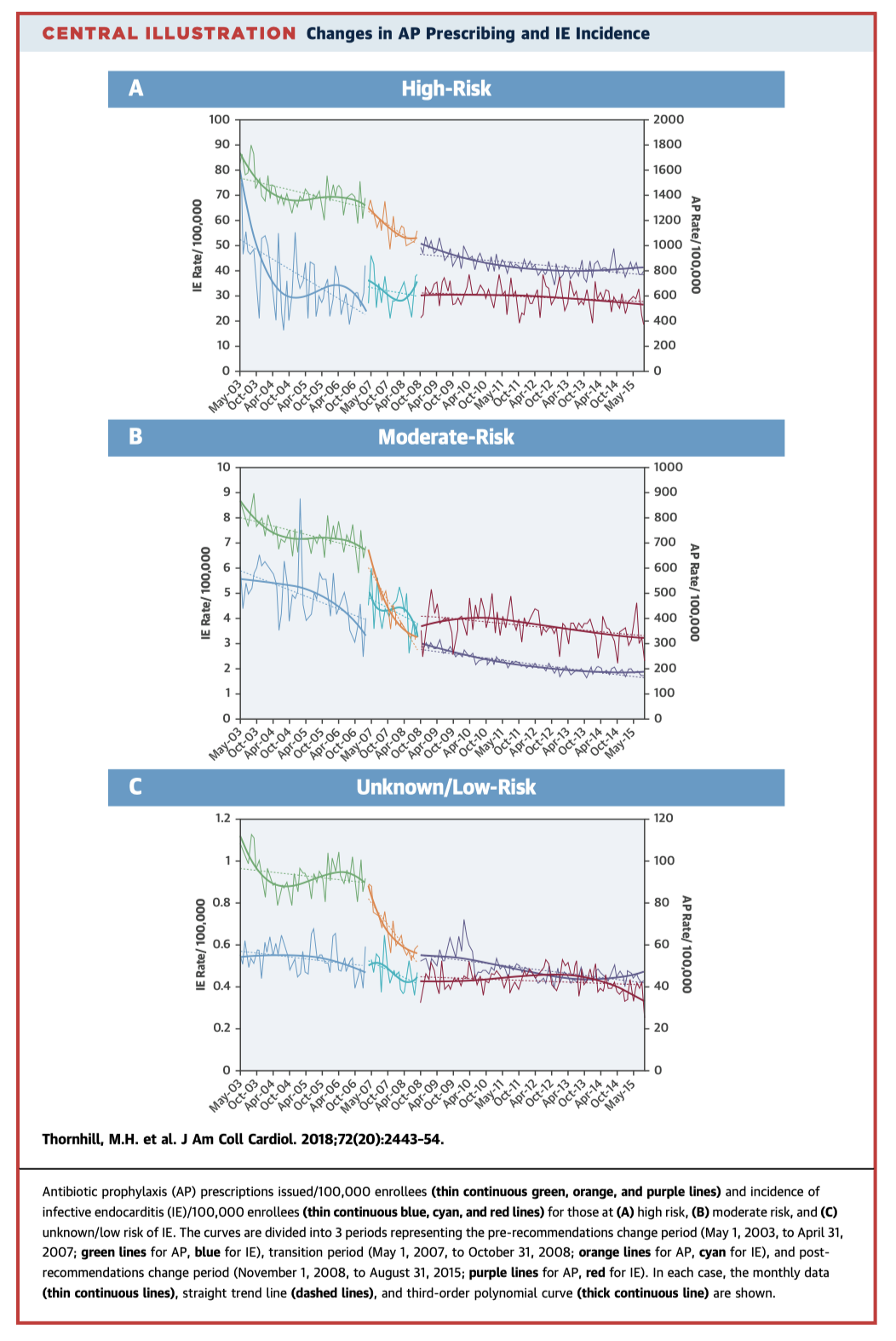
In 2007 the American Heart Association released new guidelines recommending antibiotic prophylaxis before invasive procedures should be continued for those at high risk for infective endocarditis (IE), but was no longer required for those at moderate risk. Since that time, antibiotic prophylaxis prescribing has fallen by 64% for moderate risk patients, and 20% for high risk patients. While overall IE incidence remains in decline, Poisson model analyses demonstrate an altered trend in the post-recommendation period, corresponding to a 75% increase of IE incidence in moderate risk patients and a 177% increase in high risk patients.
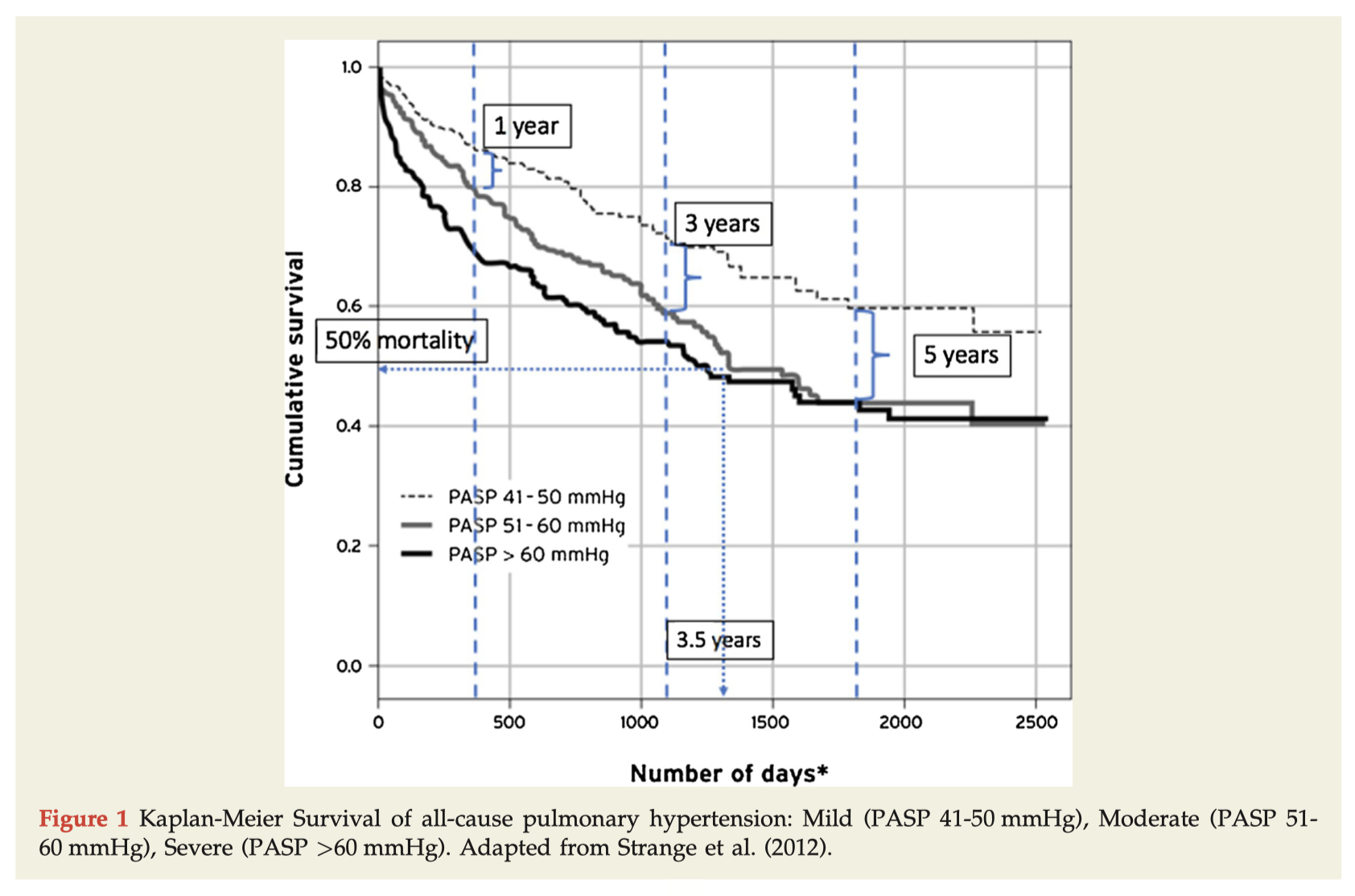
The natural history of pulmonary hypertension (PH) is insidious, with diagnosis commonly delayed. This review article recaps the epidemiology, pathophysiology, and diagnosis of PH, with a special focus on PH due to left heart disease, and surrogate echocardiographic markers of pulmonary vascular resistance.
Summarised by Dr Andrew Haymet
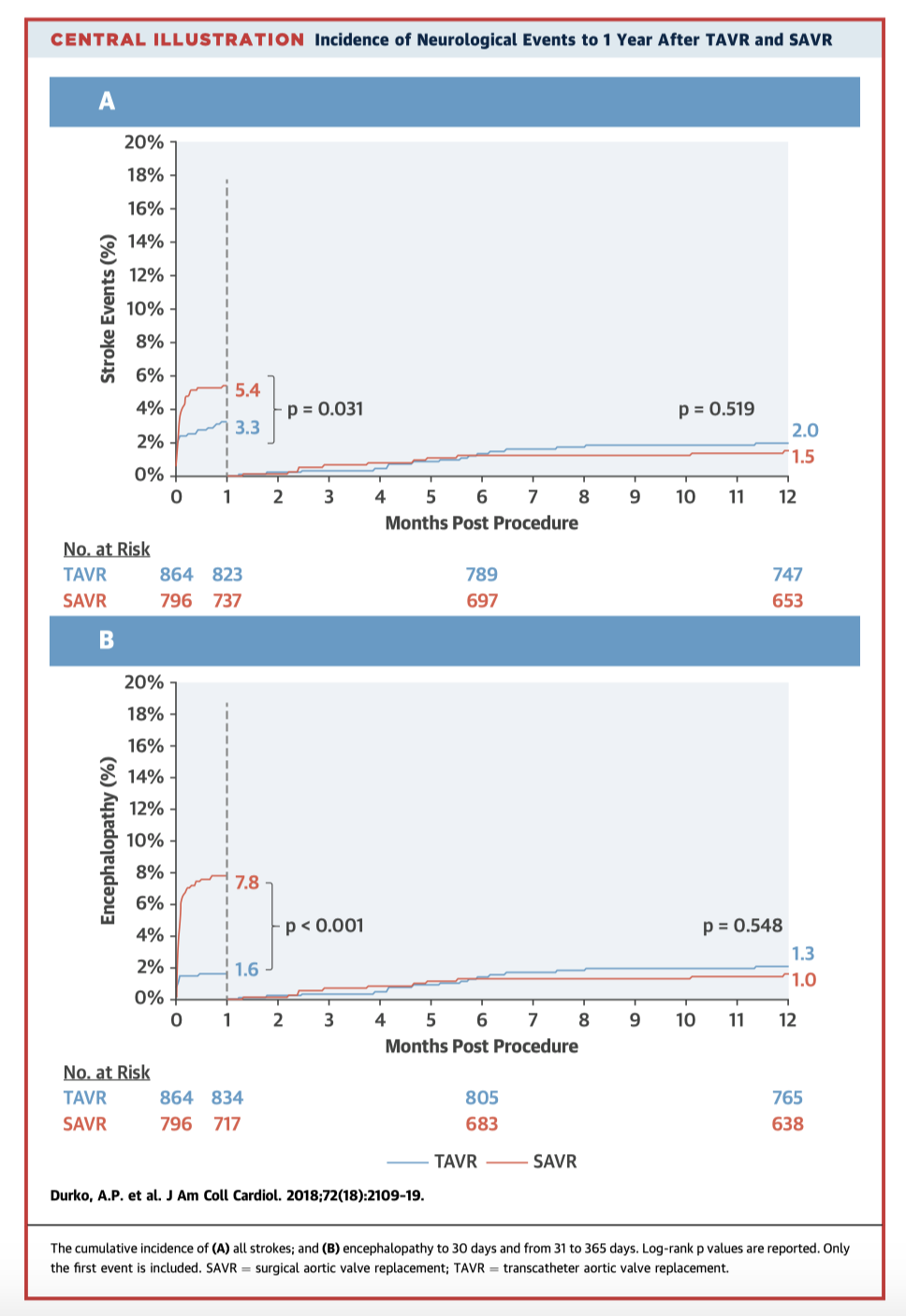
The SURTAVI trial randomised intermediate risk patients (STS predicted 30 day mortality 3 – 15%) with severe aortic stenosis to TAVR or SAVR. The rates of stroke and encephalopathy at 30-days post-procedure were higher after SAVR versus TAVR (5.4% vs. 3.3% and 7.8% vs. 1.6%, respectively). In patients with early strokes quality of life also improved earlier after TAVR. At 12-month follow-up, stroke rates and quality of life were not different.
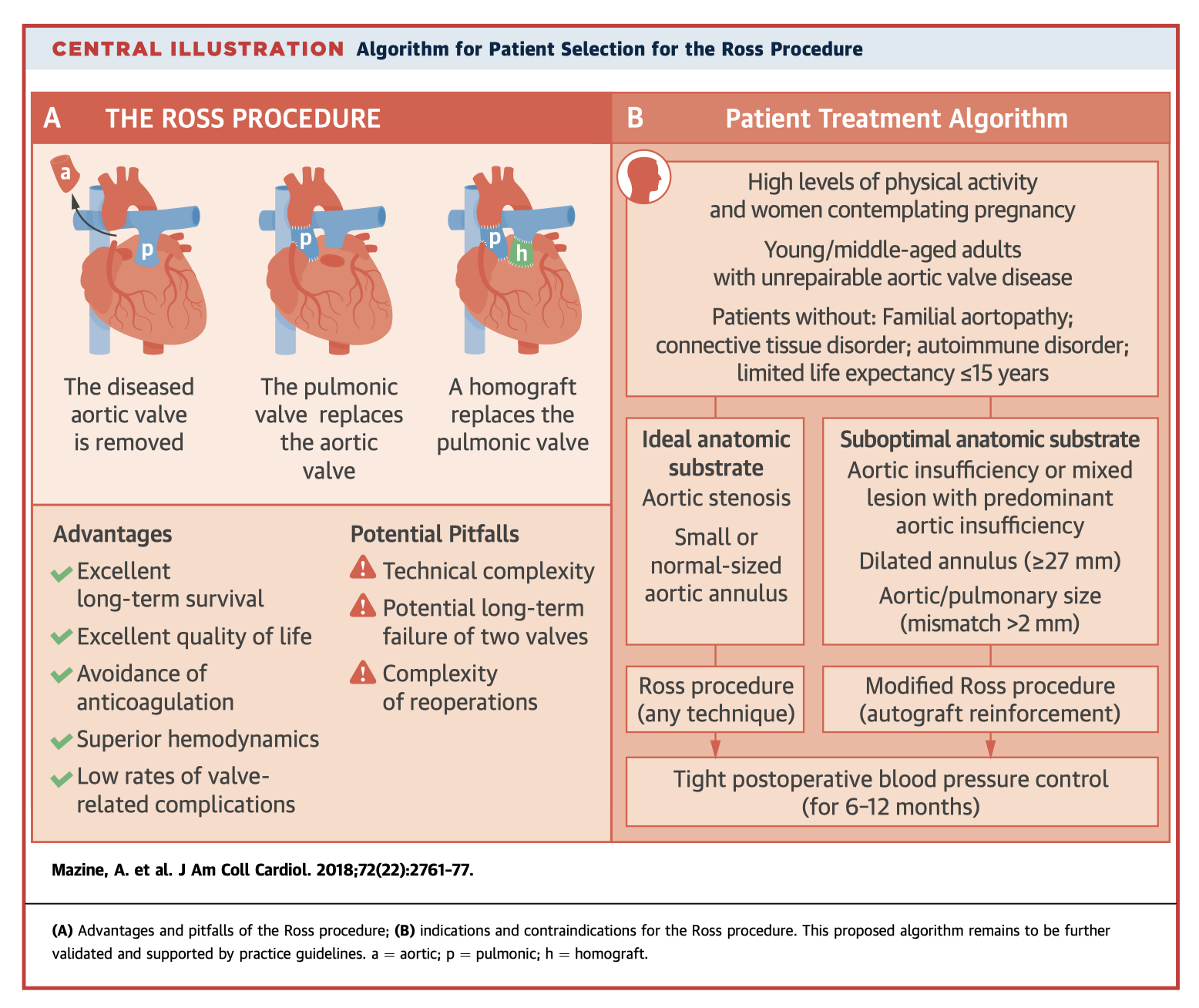
The Ross procedure is the only operation that allows replacement of the diseased aortic valve with a living substitute. Its use has declined significantly over concerns of increased surgical risk and potential long term failure. This paper reviews its indications and technical considerations, describes its advantages and drawbacks, and discusses patient selection criteria.
Summarised by Dr Sarah Catchpoole
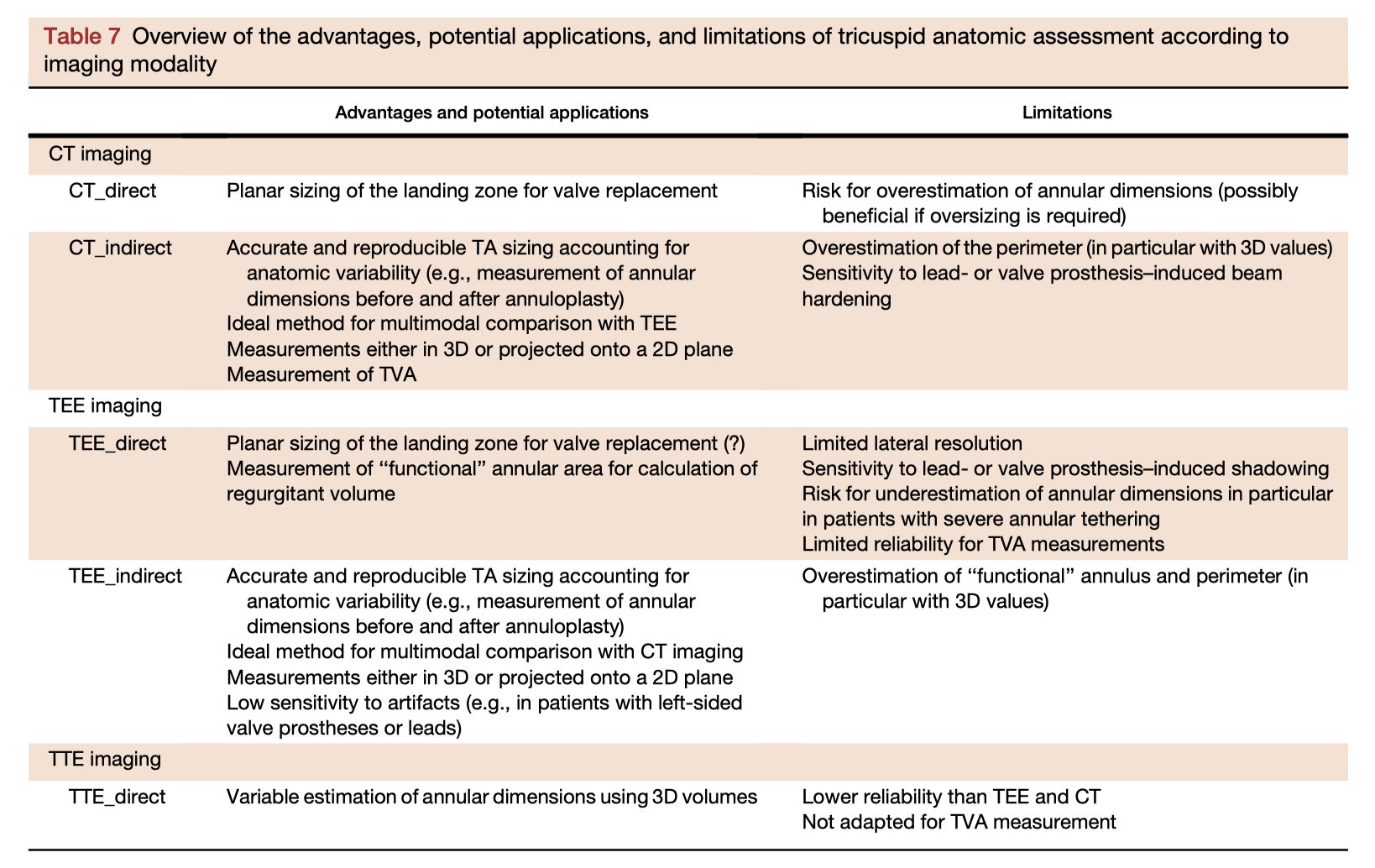
Accurate imaging of the tricuspid valve is essential for interventional planning. In a retrospective analysis, 38 patients with severe symptomatic tricuspid regurgitation (TR) underwent transthoracic echocardiography (TTE), transoesophageal echocardiography (TOE), and CT imaging. The most accurate measure of TR severity was obtained with TOE, while semiautomated indirect planimetry found high agreement between TOE and CT for measurement of the tricuspid valve area and annulus.
Ejection fraction (EF) was one of the earliest measurements of cardiac function and remains a cornerstone of modern cardiology guidelines and clinical practice. This review poses the question – what should the status be of EF in 2018, in an era when newer markers of cardiac function are available to answer the complex questions of modern cardiology? The review discusses EF physiology, measurement and technical considerations, clinical applications and population health, and finally the limitations and future of EF. While EF is here to stay, newer parameters can provide earlier diagnostic and prognostic information.
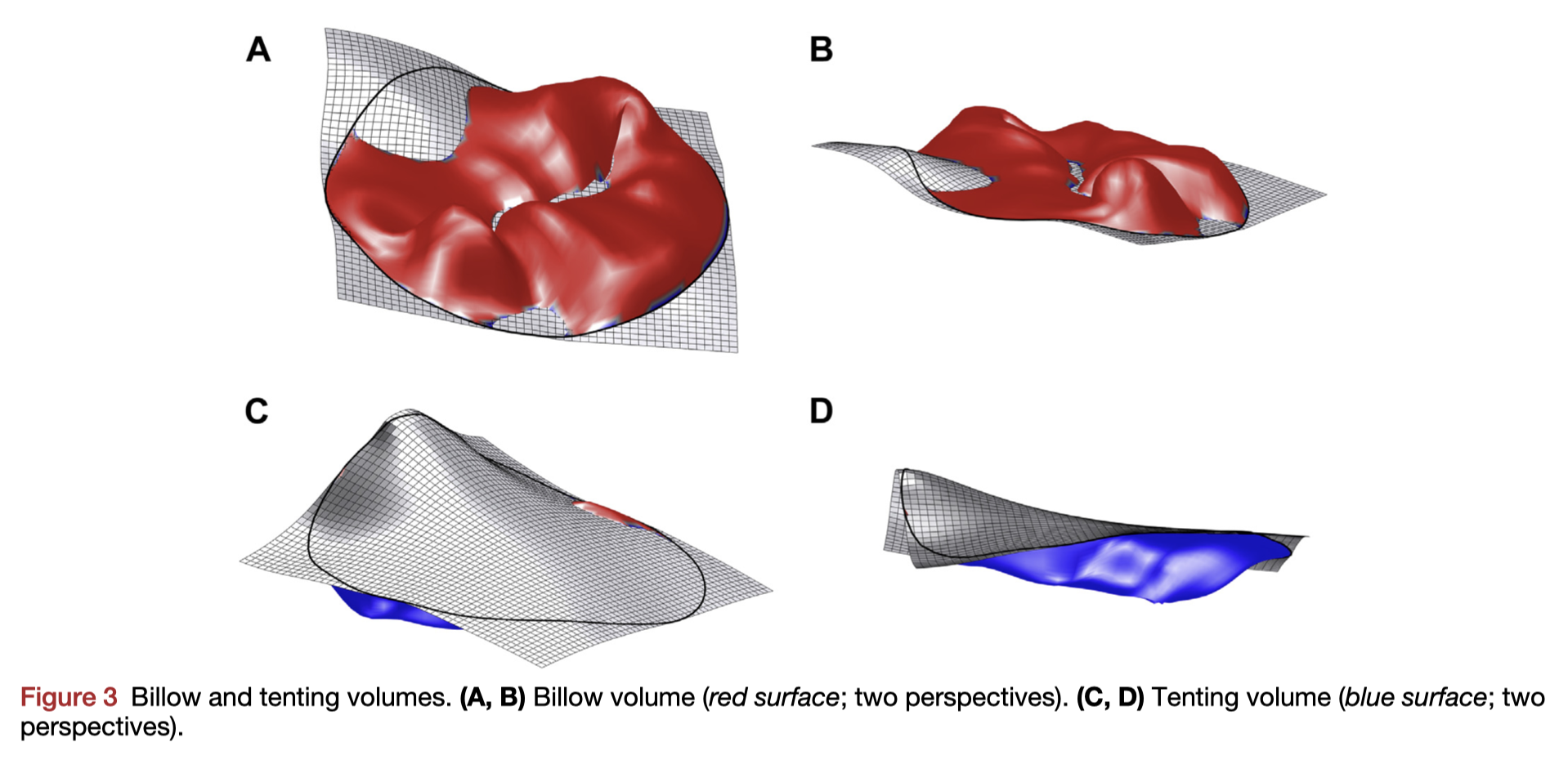
The 3D morphology of the paediatric mitral valve in Marfan Syndrome and potential relationship to mitral regurgitation (MR) is unknown. In 27 patients age 3-21, 3D echocardiography revealed a number of differences including flatter and larger annular area, greater billow volume, and smaller tenting heights compared to age-matched controls. Billow volume was strongly associated with degree of MR on multivariate analysis.
Summarised by Dr Andrew Haymet
This special article contains research highlights for the past year in cardiothoracic and vascular anaesthesia and critical care. The themes include blood management with a focus on transfusion recommendations and storage guidelines, management of cardiogenic shock and heart failure, immunosuppression for heart transplants, and transcatheter valve therapies. Other major themes include anticoagulation strategies for patients with recent percutaneous coronary interventions and concomitant AF, electrophysiology for anaesthetists, and patients with cardiovascular implantable devices who require MRI.
This paper reported the case of a 49 year old man with a potentially fatal allergy to propofol and fentanyl who underwent awake minimally invasive surgery with cardiopulmonary bypass using thoracic epidural anaesthesia, without the need for endotracheal general anaesthesia. They strongly recommend to manage spontaneous ventilation using the up and down methods of PaCO2 during CPB to prevent surgical difficulty and to restart ventilation in patients who undergo this awake procedure.
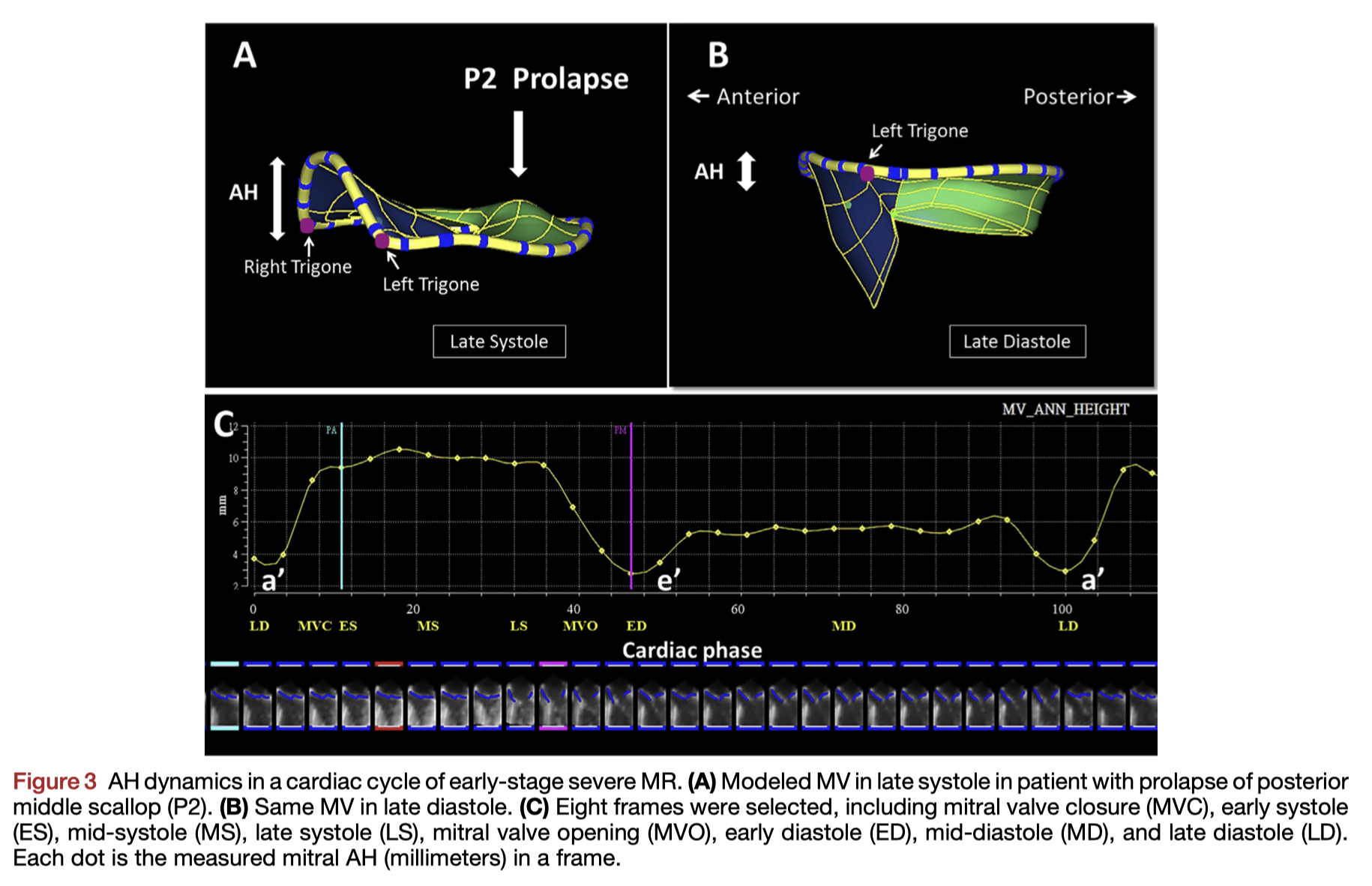
This study assessed differences in mitral annular physiology and surgical effects between early and late stage severe MR. They found that ventricular-annular decoupling was present in the late stage group, but was absent in the early stage group. Mitral valve surgery did not disrupt mitral annular saddle shape in the early stage group, however it failed to correct annular dysfunction in the late stage group. Therefore mitral annular function evaluation using sequential 3D TEE may have value in determining the stage of severe MR.