Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been recently published in each speciality (perioperative medicine, cardiac imaging, cardiology, cardiothoracic surgery).
Perioperative Medicine
Summarised by Sarah Catchpoole
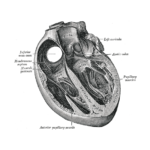
Calleja et al. performed a retrospective analysis of 94 patients who underwent 3D transesophageal echocardiography prior to mitral valve repair to determine predictive parameters for surgical planning. 3D annular circumference was an independent predictor of implanted annuloplasty band length. P2 segment length and leaflet area best discriminated the need for leaflet resection. These parameters could provide guidance for choice of mitral annuloplasty ring or band size and the decision regarding leaflet modification.
General agreement on the best anesthetic management of patients undergoing transcatheter aortic valve implantation (TAVI) is lacking. This expert review discusses current attitudes, including local vs. general anaesthesia, management of intraprocedural complications, patient fitness, and performance of intraprocedural TEE. While indicated in less experienced teams, the authors suggest the low incidence of intraoperative complications does not justify the widespread use of general anaesthesia for percutaneous transfemoral and transaxillary approaches.
Furniss & Sneyd. Safe sedation in modern cardiological practice. Heart. 2015 Oct
A report produced following new guidance on safe sedation in the United Kingdom. It gives an overview of considerations for sedation in specific procedures such as TOE and transcatheter aortic valve replacement, as well as specific recommendations and guidelines derived from the new guidance document.
Cardiac Imaging
Summarised by Sarah Catchpoole
Measures of ventilatory efficiency are prognostic of mortality in patients who may require transcatheter pulmonary valve implantation (TPVI), and speckle-tracking echocardiographic (STE) measures of RV function appear to improve after TPVI. However, the relationship between these two measures is unknown. In a retrospective secondary analysis of data collected for the COMPASSION trial, change in minute ventilation [VE]/carbon dioxide production [VCO2] slope was independently associated with change in RV longitudinal early diastolic strain rate and tricuspid A velocity. In addition, pre-procedure RV longitudinal strain was found to be a predictor of change in VE/VCO2 after TPVI, demonstrating predictive potential of RV STE measurement for outcomes of TVPI.
This comprehensive resource will be useful to all cardiac specialties and details the contributions of echocardiography in management of patients with Left Ventricular Assist Devices (LVAD), with a focus on continuous flow models. It provides considerations, recommendations and sample protocols for the timing of echocardiography during patient selection, device implantation, and postoperative care.
Echocardiography is the standard for follow-up of prosthetic heart valve (PHV) function, but has several well-known limitations. Sucha et al. identified 82 articles for inclusion in a systematic evidence-based literature overview assessing CT and MRI as additional imaging modalities for PHV evaluation, emphasising feasibility, diagnostic role, and added value in relation to established techniques. MRI was best for evaluation of PHV-related flow patterns and velocities. CT is prone to artefact in older valves and showed no advantage over echocardiography for detection of vegetations or periprosthetic regurgitation. However, it may make significant contributions in detection of obstruction cause (pannus or thrombus), bioprosthesis calcifications, and endocarditis extent.
Cardiology
Summarised by Sarah Catchpoole
Moderate mitral regurgitation (MR) in aortic valve replacement is associated with significantly higher mortality. MR in patients undergoing TAVI is common but of uncertain clinical relevance. Takagi et al. have undertaken the first meta-analysis of post-TAVI mortality in patients with various grades of MR. 16 eligible studies with a total of 13,672 patients were identified; pooled analyses revealed a significant increase in early and overall all-cause mortality in patients with coexisting MR.
In this retrospective cohort study, 107 patients discharged within 72 hours after TAVI were compared with a propensity matched cohort of 358 patients discharged after 3 days. At 30 days after discharge, there were no significant differences in patient outcomes (rates of death, bleeding, permanent pacemaker implantation, and rehospitalisation). Early discharge was predicted by less severe baseline symptoms, no in-hospital bleeding, and a prior permanent pacemaker. Year of procedure also predicted early discharge, suggesting outcomes improve with increasing staff experience in TAVI. These findings support the feasibility of early discharge in low-risk patients after TAVI, with the benefit of reduced costs.
There is no current medical therapy to prevent development or progression of aortic stenosis (AS). Following 220 patients over 3.5 years, Capoulade et al. found elevated levels of lipoprotein(a) (Lp(a)) and oxidized phospholipids on apolipoprotein B-100 (OxPL-apoB ) are associated with faster AS progression and need for aortic valve replacement. Interestingly, progression of AS for high vs. low Lp(a) levels was more pronounced in individuals under 57 years, indicating a pathological role more pronounced in the young due to the strong genetic determination of Lp(a). While disease mechanisms are still unclear, these findings could provide a rationale for randomized trials of Lp(a)-lowering and OxPL-apoB lowering therapies in AS.
Cardiothoracic Surgery
Summarised by Andrew Haymet
Whilst valve-in-valve transcatheter aortic valve therapies have been showing promise for treating failed bioprosthetic valves, their haemodynamic performance within deteriorated surgical valves remains unknown. The in vitro hydrodynamic performance of two commercially available valves, the Medtronic CoreValve and the Edwards SAPIEN XT, were assessed in two different bioprosthetic aortic valves, the Edwards Perimount and St Jude Trifecta. Both transcatheter valve prostheses performed well, with all hydrodynamic results complying with the International Organization for Standardization standards for all configurations.
Exposing the papillary muscles during minimally invasive mitral valve repair can be challenging. A simple but effective technique of cutting, rolling and suturing a sterile paper ruler, which is then inserted within the mitral leaflets, has been described. This technique exposed the papillary muscles well and avoided both leaflet and chordal damage during artificial chordal implantation.’ 
Percutaneous mitral repair with the MitraClip system (Abbott Vascular) is currently approved for patients with degenerative mitral valve disease who are of prohibitive surgical risk. 468 patients were referred for MitraClip between 2007 and 2014, of whom 156 (33.3%) received a MitraClip and 82 (17.5%) underwent surgical interventions. The volume of isolated mitral valve operations increased by 80%, with operative mortality of 2.6%. A successful percutaneous and surgical mitral valve program requires multidisciplinary input, including from experienced mitral surgeons.





 Stainback et al. Echocardiography in the Management of Patients with Left Ventricular Assist Devices: Recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2015 Aug
Stainback et al. Echocardiography in the Management of Patients with Left Ventricular Assist Devices: Recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2015 Aug