Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been recently published in each speciality (Cardiology, Cardiac Surgery, Cardiac Imaging, Perioperative Medicine).
Summarised by Dr Sarah Catchpoole
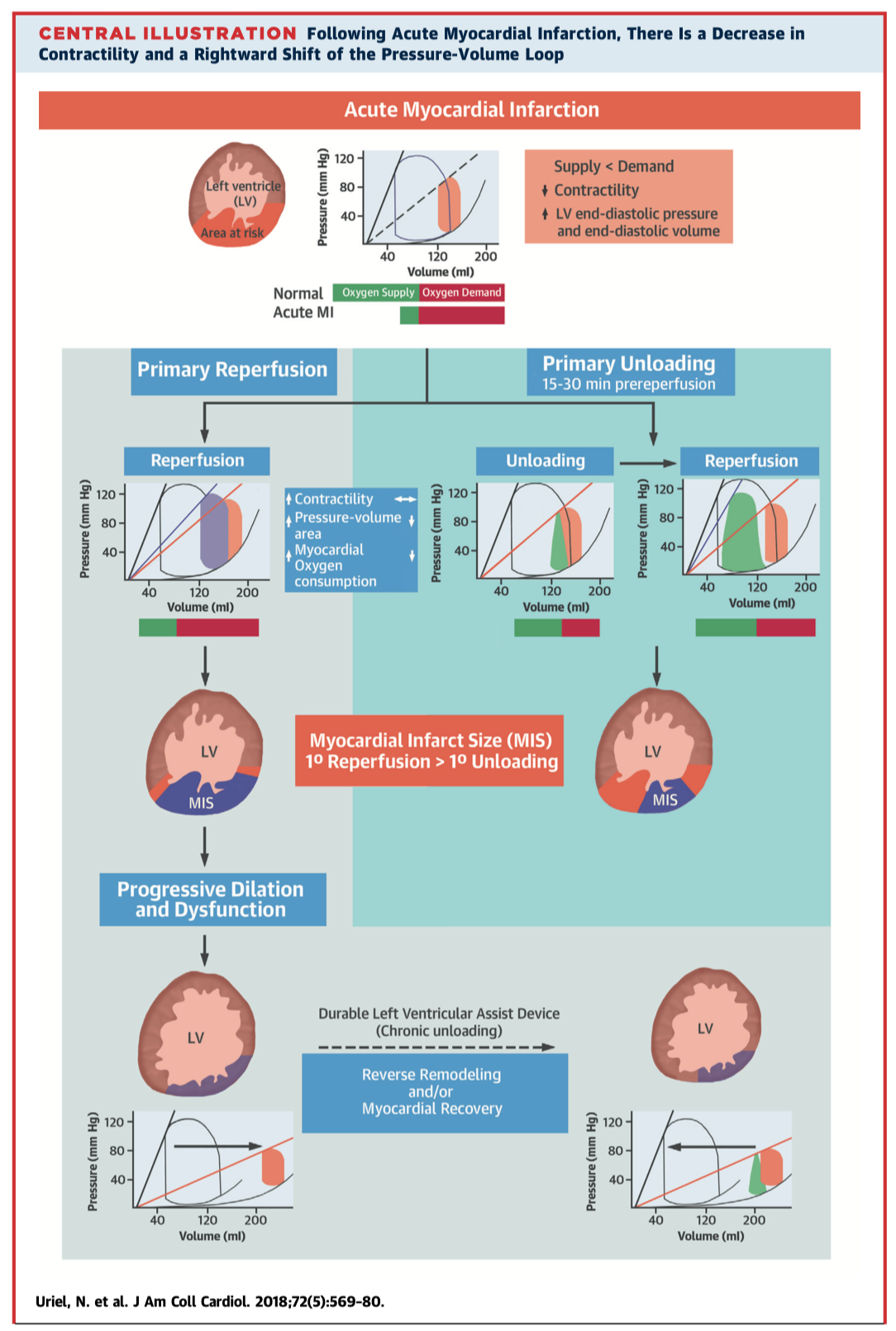
Uriel N, et al. Mechanical Unloading in Heart Failure. J Am Coll Cardiol. 2018 Jul 31.
Mechanical unloading reduces the power expenditure and hence stress on the left ventricle, with positive structural, cellular, molecular, and genetic changes in both the short and long-term setting. This review details the pathophysiology and clinical potential of mechanical unloading to reduce or even reverse adverse left ventricular remodelling. Current clinical trials are examining the benefits of both early unloading, for example in the setting of acute myocardial infarction; and late unloading in chronic heart failure.
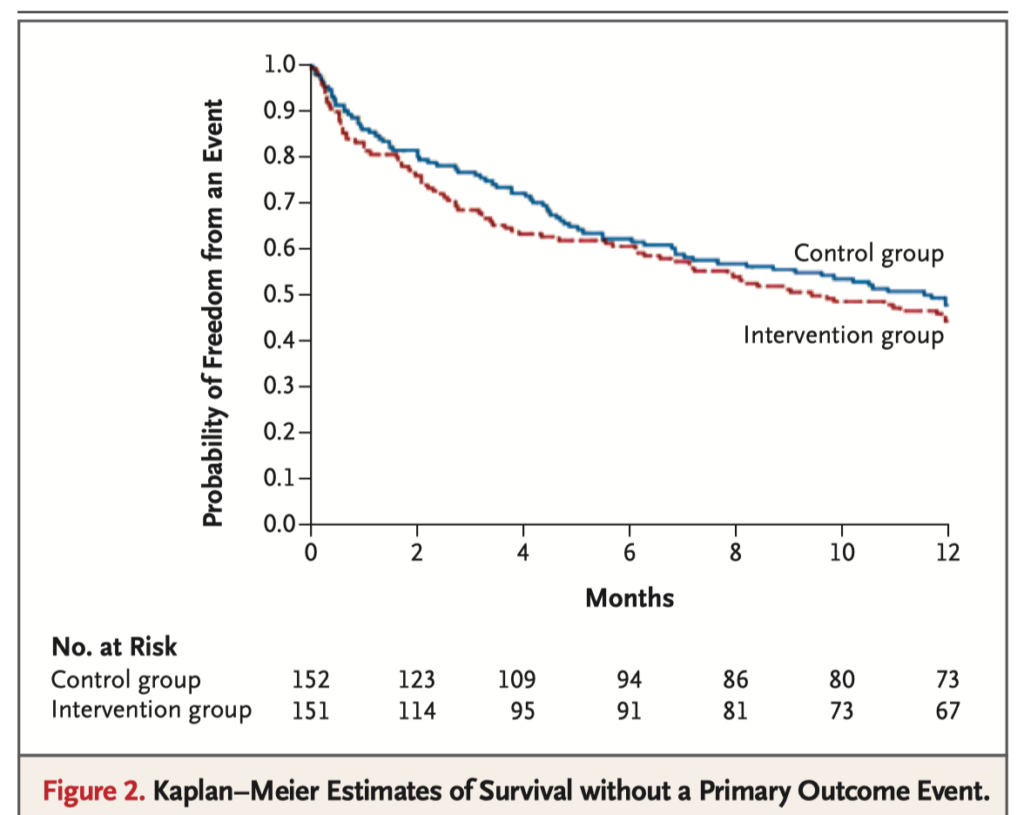
Results of the MITRA-FR trial show no clinical benefit of percutaneous mitral valve repair (MVR) over medical therapy alone in the setting of chronic heart failure with secondary severe mitral regurgitation. In this national multicenter randomized controlled trial, there was no difference at one year between the control group (n=152, medical therapy alone) and intervention group (n=152, medical therapy + percutaneous MVR) for the primary outcome of all cause death or unplanned hospitalization for congestive heart failure (51.3% vs 54.6%, respectively, OR 1.1, CI 0.73-1.84; p=0.53).
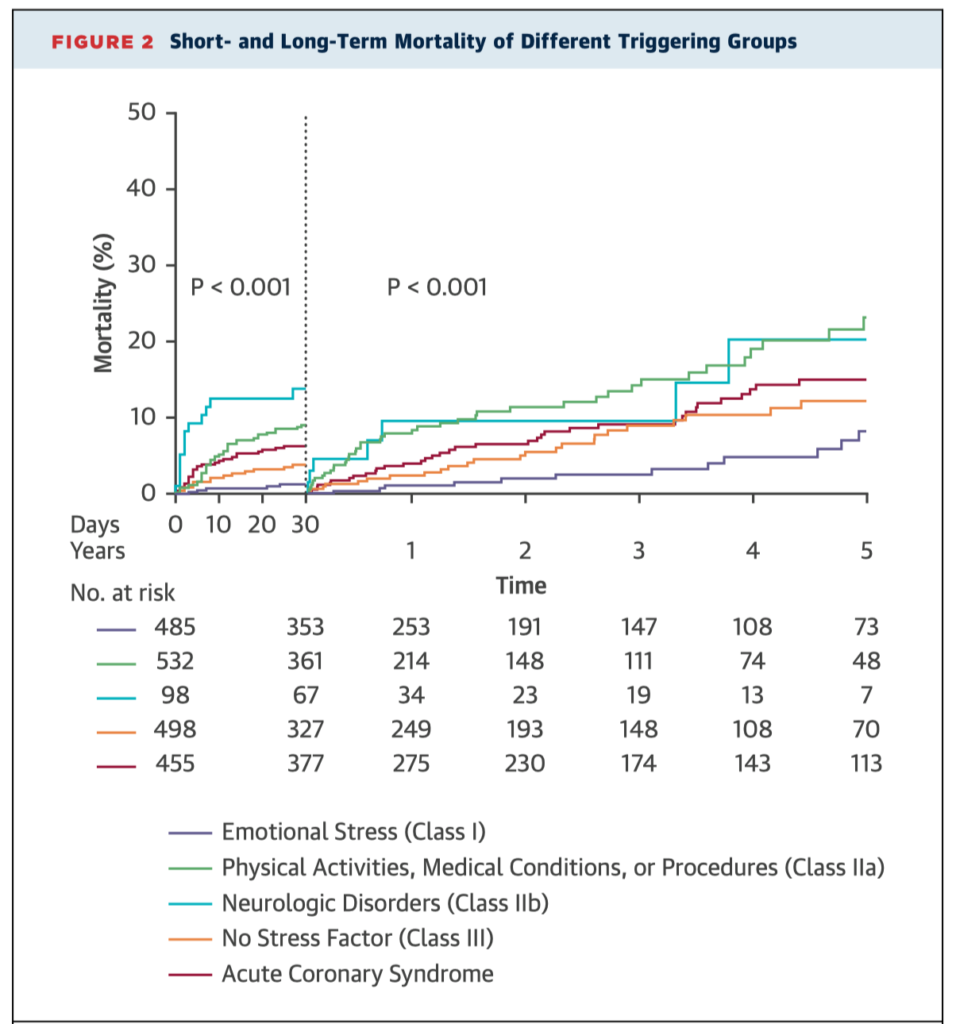
Takotsubo cardiomyopathy remains poorly understood, with possible triggers including both physical and emotional stress. This study shows the prognosis of takotsubo syndrome varies significantly according to precipitating event, with physical and neurologic triggers associated with higher mortality. A new classification system (InterTAK) is proposed to aid risk stratification.
The prevalence of adult congenital heart disease (ACHD) continues to grow largely due to the successes of paediatric cardiology and cardiothoracic surgery. These comprehensive new guidelines from the AHA/ACC will assist clinicians to provide best-practice evidence based treatment in this sometimes challenging population.
Summarised by Dr Andrew Haymet
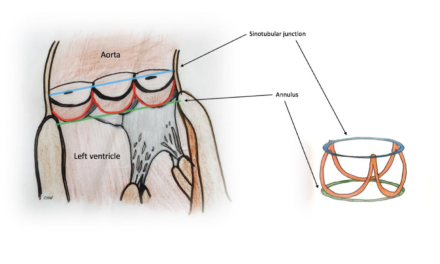
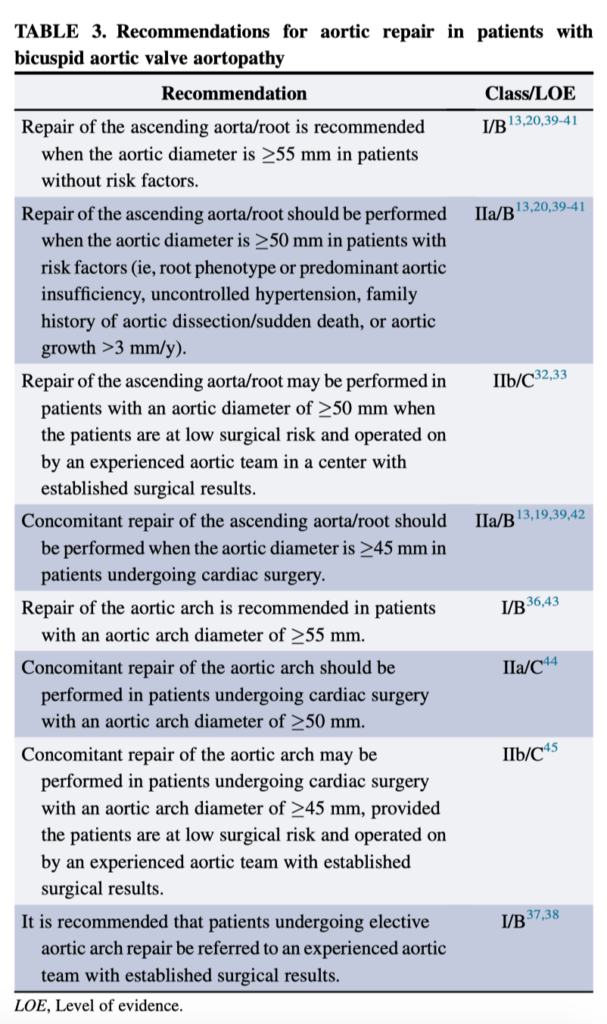
Bicuspid aortic valve disease is a common congenital cardiac disorder, present in 1% to 2% of the general population. Associated thoracic aortic dilation is noted in approximately 40% of patients in referral centers. This document is an executive summary of The American Association for Thoracic Surgery Guidelines on Bicuspid Aortic Valve–Related Aortopathy. These guidelines provide a comprehensive review of the natural history, imaging, indications for surgery and follow-up recommendations.
Excellent commentary: Braverman AC. Aortic replacement for bicuspid aortic valve aortopathy: When and why? The Journal of Thoracic and Cardiovascular Surgery. 2018 Jul 3.
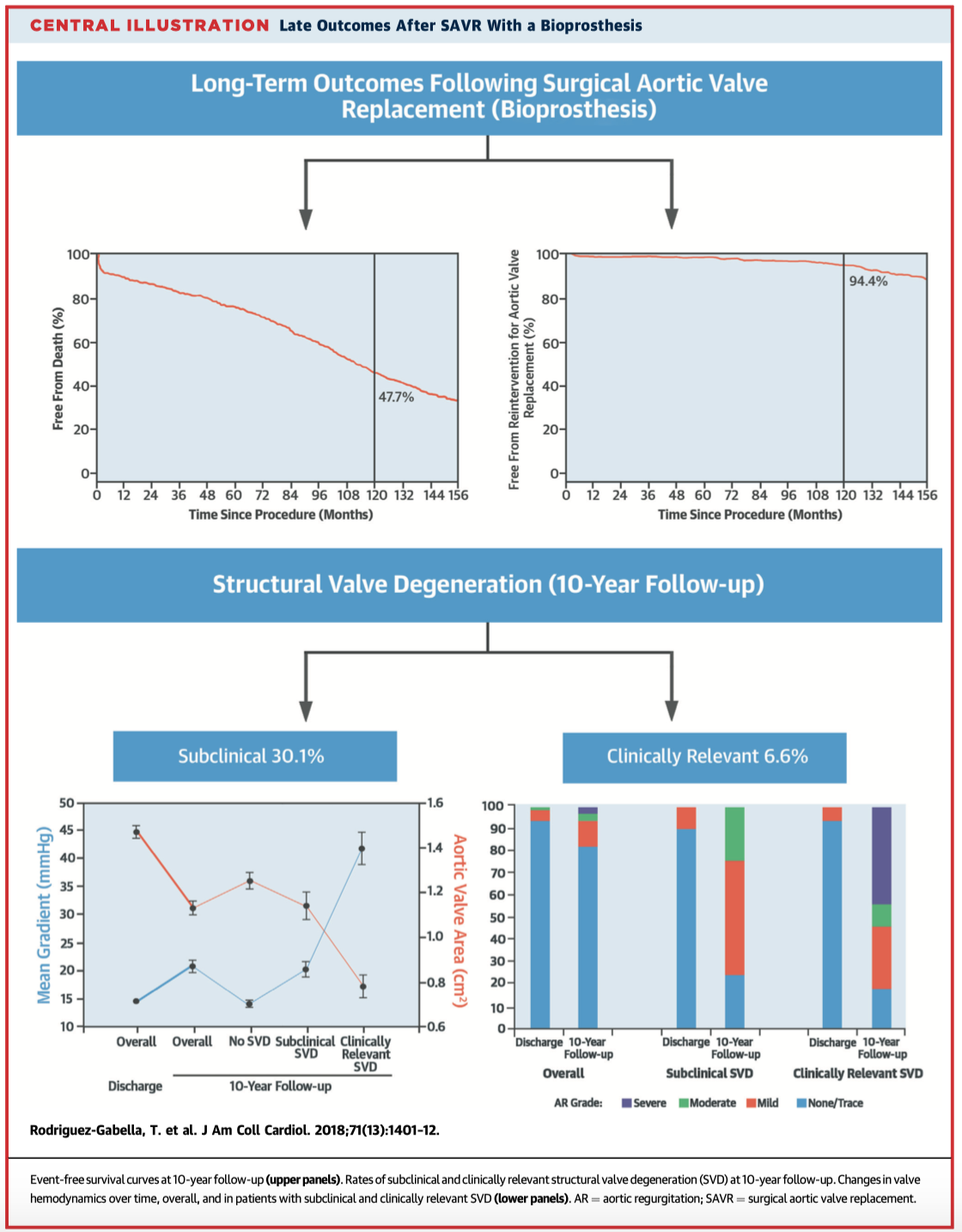
This study looked at the long-term outcomes of 672 consecutive patients who underwent bioprosthetic SAVR. At a median follow-up of 10 years (IQR 5 to 13 years), 64.3% of patients had died. Older age, left ventricular dysfunction, atrial fibrillation, chronic obstructive pulmonary disease, greater body mass index, and diabetes mellitus were associated with an increased mortality risk. The 10-year mortality rate in elderly patients was considerable, chiefly determined by their older age and the presence of comorbidities.
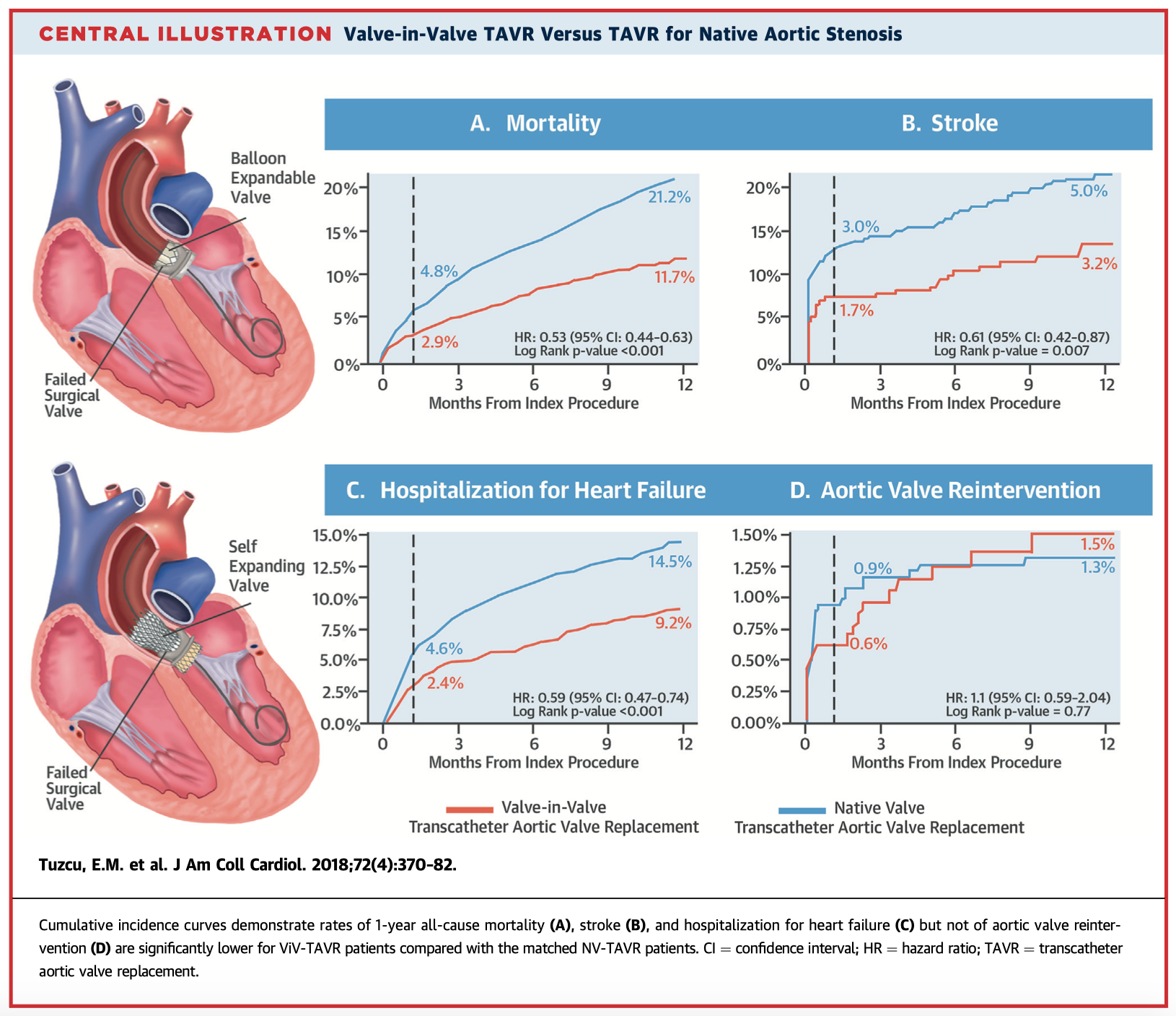
This study of 1,150 patients sought to evaluate the safety and effectiveness of Valve-in-Valve (ViV) TAVR for failed SAVR by comparing it with the benchmark of native valve (NV) TAVR. Unadjusted analysis revealed lower 30-day mortality (2.9% vs. 4.8%), stroke (1.7% vs. 3.0%), and heart failure hospitalisations (2.4% vs. 4.6%) in the ViV-TAVR compared with NV-TAVR group. Comparison with the benchmark NV-TAVR shows ViV-TAVR to be a safe and effective procedure in patients with failed SAVR who are at high risk for repeat surgery.
Summarised by Dr Sarah Catchpoole
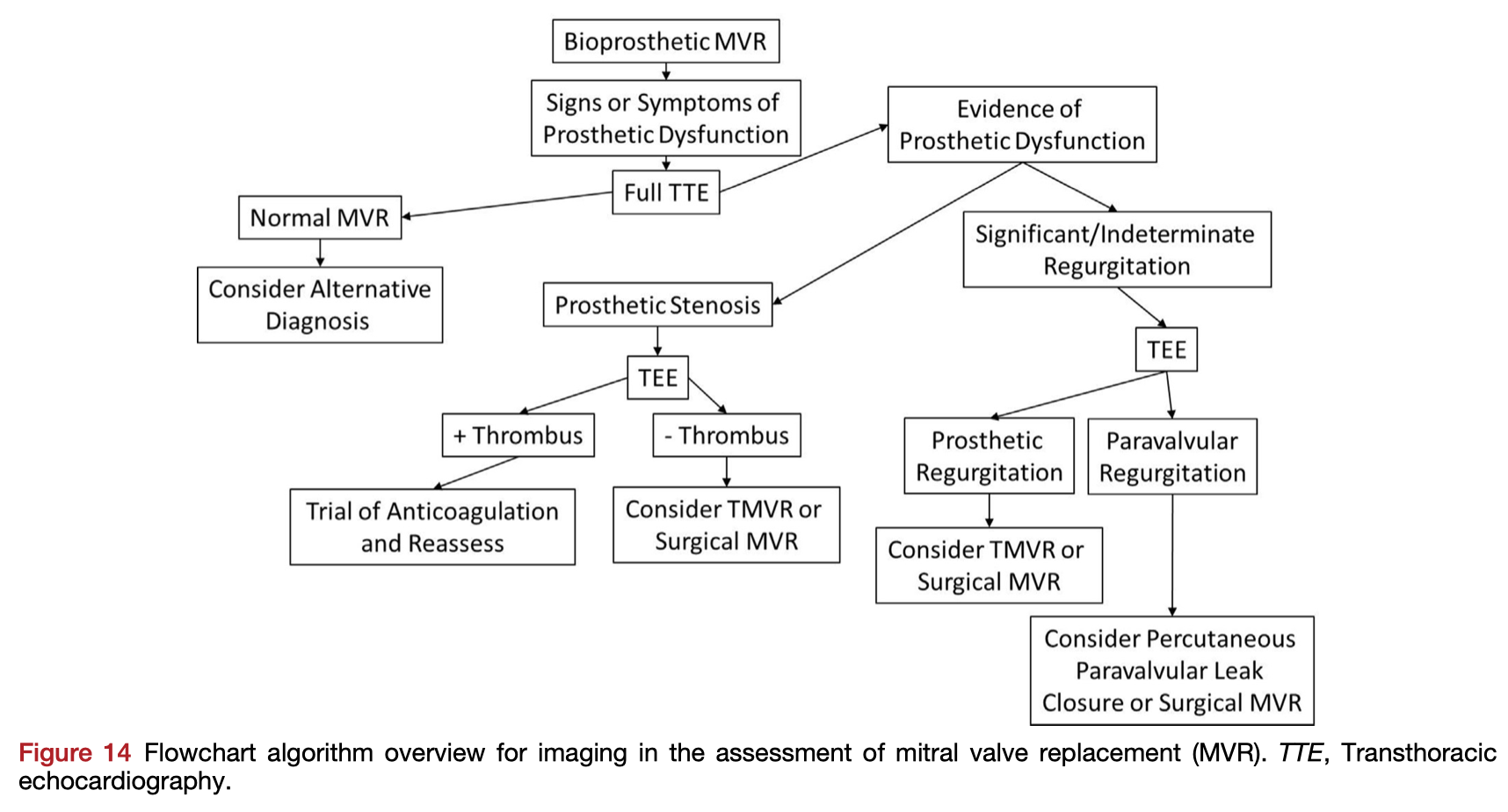
Transcatheter Valve-in-Valve implantation could avoid repeat open heart surgery in the setting of the failing mitral bioprosthesis. This paper recommends 2D and 3D echocardiographic imaging techniques for all stages of the transcatheter valve replacement process, including pre-procedural work up and planning, intraprocedural guidance, and post-procedural evaluation.
Overall incidence of leaflet thrombosis after transcatheter aortic valve replacement (TAVR) using active 4D CT surveillance is between 7-14%. In this cohort of 612 patients, targeted use of 4D CT (where there was clinical or echocardiographic suspicion of leaflet thrombosis) found thrombosis in 30.9% of TAVR patients, and 32.6% of surgical AVR patients. The authors suggest selective use of 4D CT has a high detection rate for leaflet thrombosis and could avoid unnecessary anticoagulation.
Summarised by Dr Andrew Haymet
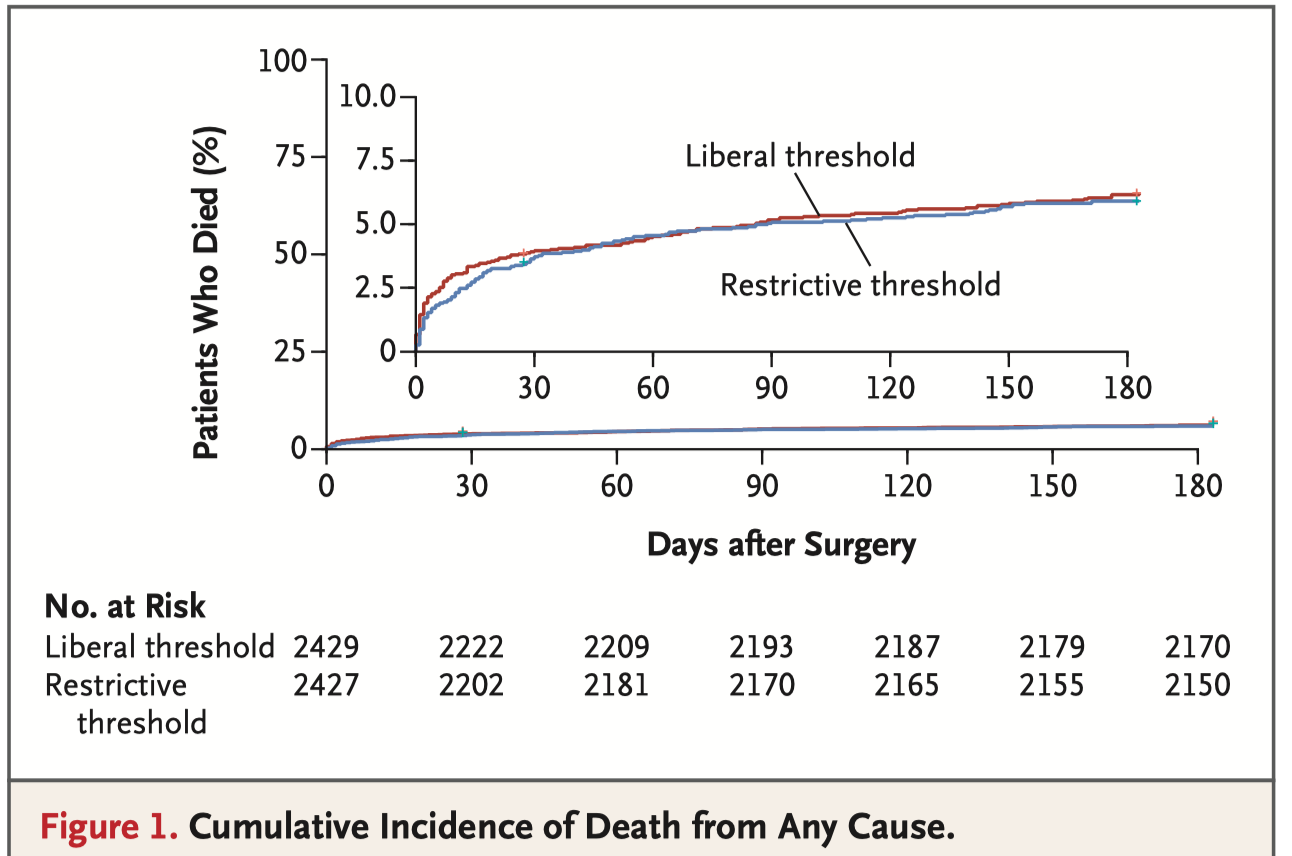
These are the 6 month results of the TRICS III trial (the outcomes at day 28 postop were previously reported). In this trial 5,243 moderate to high risk adults undergoing cardiac surgery were randomly assigned to a restrictive red cell transfusion strategy (i.e. Hb < 7.5g/dL intraoperatively or postoperatively), or a liberal strategy (i.e. transfuse if Hb < 9.5g/dL postoperatively in ICU, or <8.5g/dL in a non ICU ward). At 6 months a composite of all-cause death, MI, stroke & new onset renal failure was not different (17.4% restrictive vs. 17.1% liberal, OR 1.02, NS). These findings are similar to the earlier findings at 28 days.
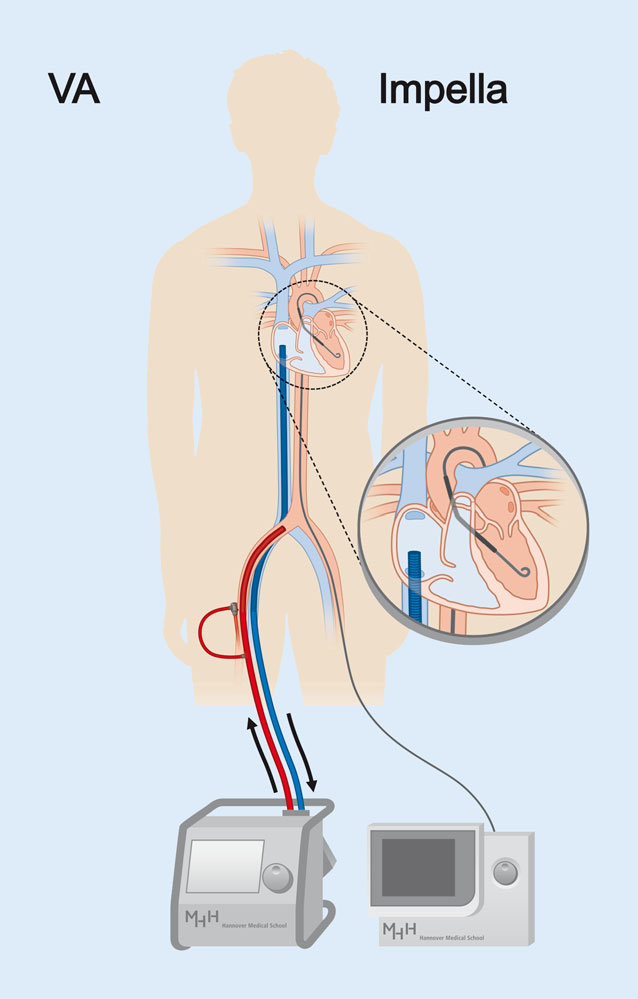
Venting is an important concept in myocardial protection during cardiopulmonary bypass that reduces ventricular distention and myocardial oxygen consumption. Venting in peripheral VA ECMO is difficult because of the lack of central access. One proposed method is through the use of an Impella device across the aortic valve to empty the ventricle. This was a retrospective review of 12 patients who underwent this strategy. Compared to 47 VA ECMO patients without LV venting during the same period, they had improved survival and LV function on echocardiography, suggesting this could be a useful strategy in some patients.
The use of transcatheter mitral valve therapies are expanding rapidly. This review discusses the anaesthetic considerations for patients undergoing both transcatheter mitral valve replacement (TMVR) and transcatheter mitral valve repair (TMVRep). The authors describe their institutional experience, including potential pitfalls and complications, concluding with a discussion of the role of transoesophageal echocardiography in these patients.