Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been recently published in each speciality (Cardiology, Cardiac Surgery, Cardiac Imaging, Perioperative Medicine).
Cardiology
Summarised by Dr Sarah Catchpoole
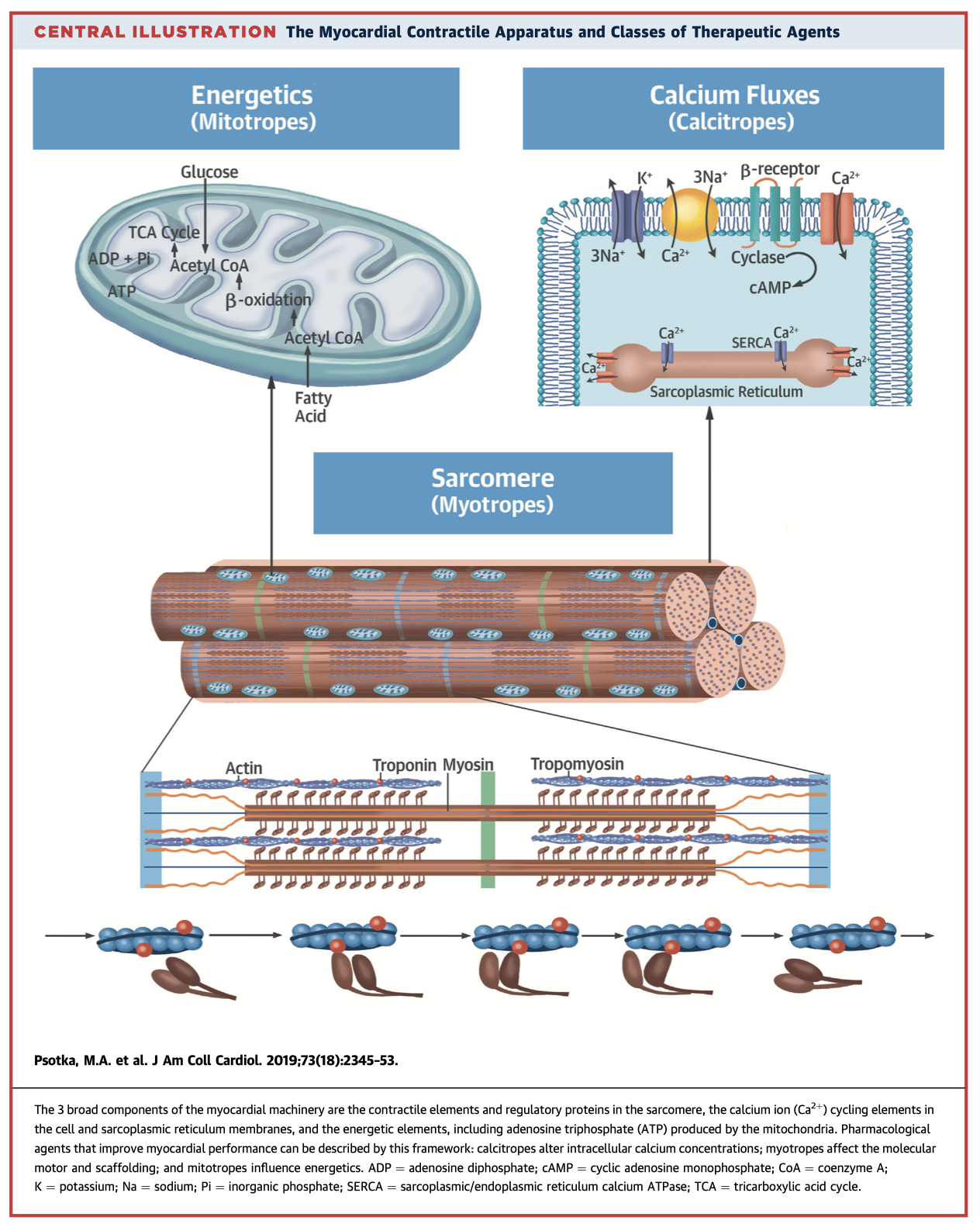
The term “inotrope” is too broad to effectively describe emerging and potential therapies for cardiac contractile function. In this review paper, the authors revise the physiology of the myocardial contractile apparatus and the targets of these novel pharmaceutical agents. They propose a new framework to more specifically categorise these molecules: (1) cardiac calcitropes, which modulate intracellular calcium concentrations; (2) cardiac myotropes, which directly affect myosin; and (3) cardiac mitotropes, which act on myocardial energetics.
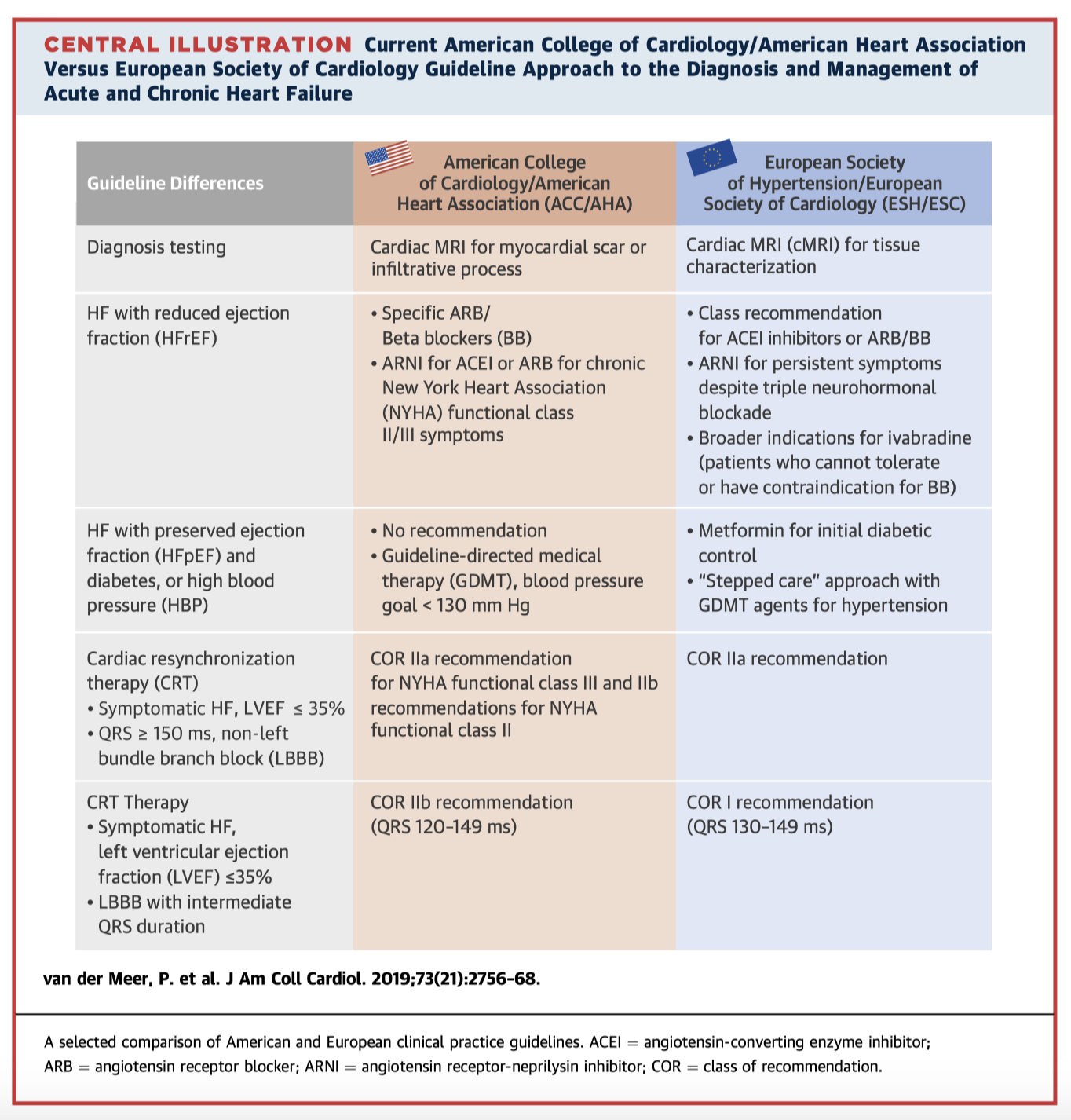
The American College of Cardiology/American Heart Association guidelines for the management of heart failure were last updated in 2013 with revisions in 2016 and 2017, while the European Society of Cardiology guidelines were last updated in 2016. This focused review highlights key similarities and differences between the two guidelines, including levels of evidence for specific recommendations. In addition, the authors review new studies published since the last updates which may influence clinical practice and future guideline revisions.
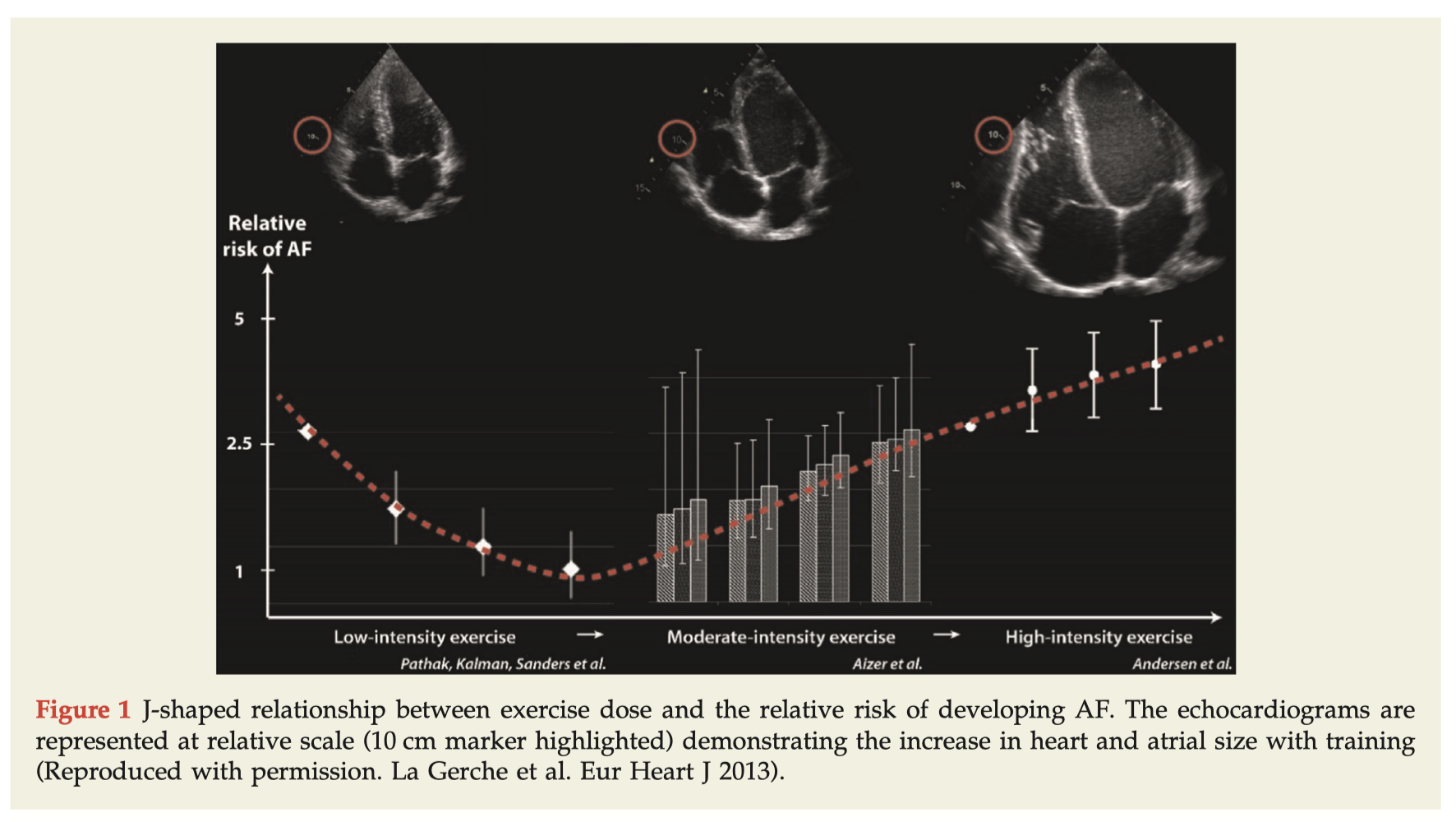
There is a growing body of evidence supporting a link between endurance exercise and higher incidence of atrial fibrillation (AF). This paper critically reviews the available literature behind this association, which is largely derived from retrospective cohort or case control studies and using male populations. Secondly, the authors postulate potential underlying mechanisms contributing to the increased risk of AF, as supported by correlates in non-athletes. These include left atrial enlargement (Figure 1), increased atrial pressures during exercise, increased vagal tone and bradyarrhythmias, and inflammation and myocardial fibrosis.
Cardiac Surgery
Summarised by Dr Andrew Haymet
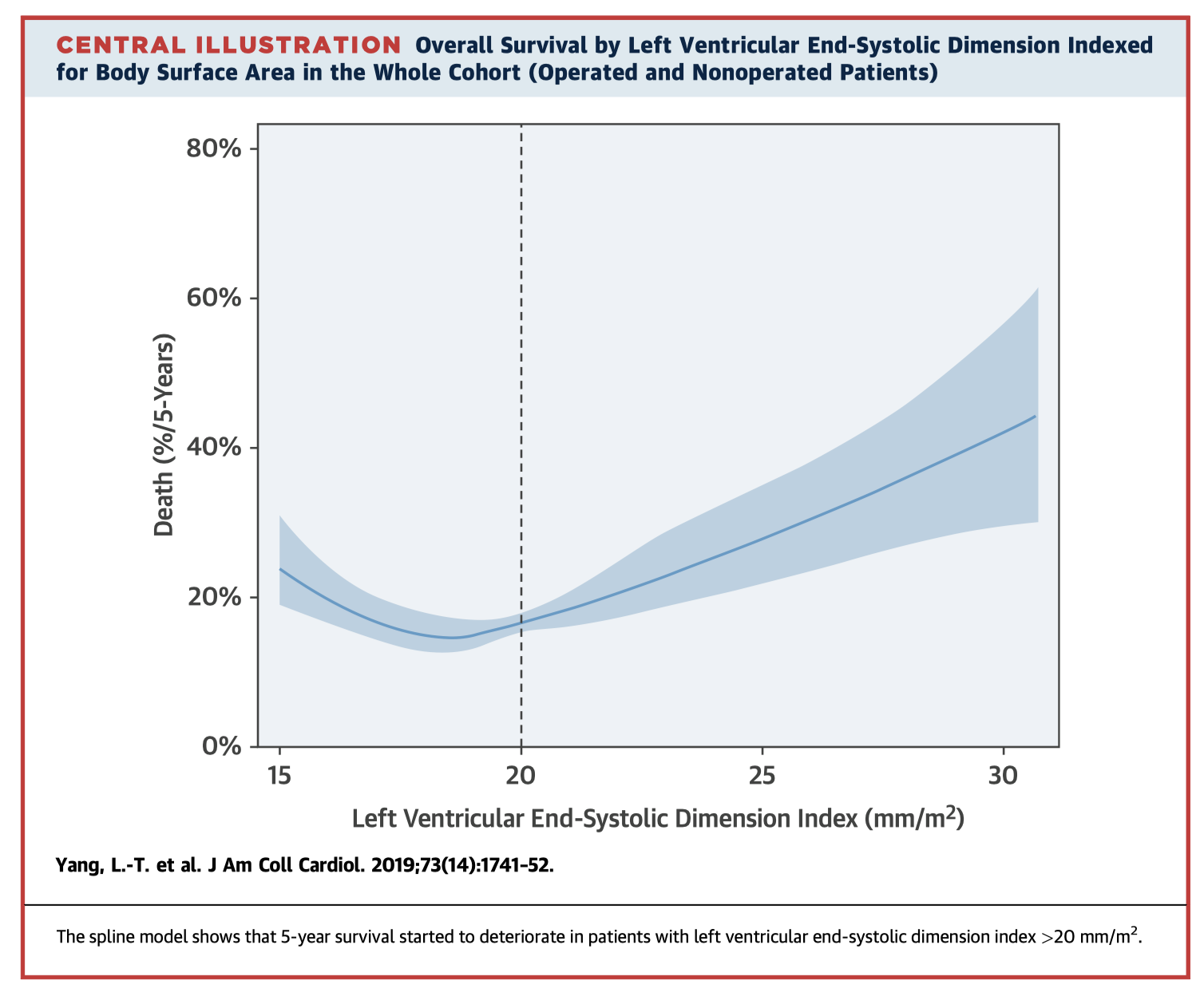
This study aimed to assess the prognostic value of left ventricular dimensions in significant AR. 748 consecutive patients underwent surgery from 2006 to 2017. Most patients had Class I guideline indications for surgery (79%), and fewer had Class II (14%) or no Class I/II indications (7%). At a median follow-up of 4.9 years, 17% of patients had died. Higher LV end-systolic dimension index (LVESDi) was associated with all-cause mortality. Compared with patients having LVESDi <20 mm/m2, those with LVESDi 20 to 25 (HR 1.53) and >25 (HR 2.23) had increased risks of death. These results challenge traditional recommendations of waiting until severe LV dilatation and suggest operating earlier may result in improved outcomes.
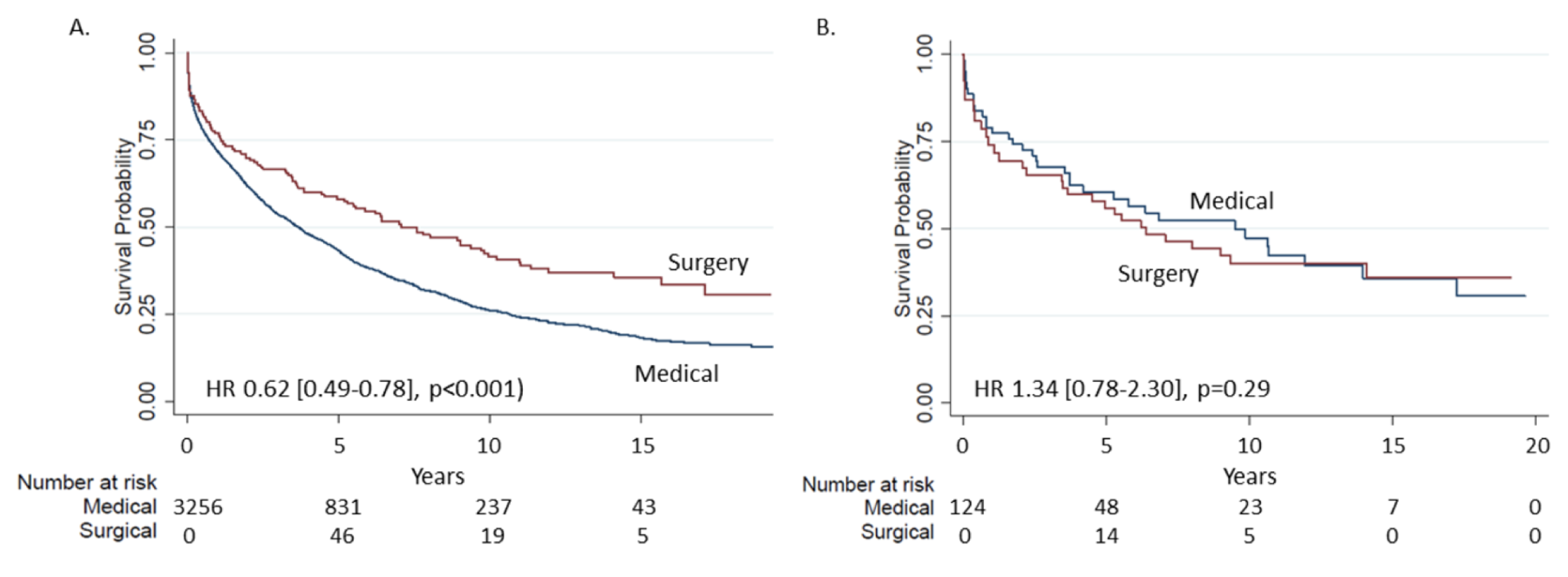
Patients with isolated TR in the absence of left sided valvular dysfunction are historically managed nonoperatively. This retrospective analysis of 3,276 adult patients aimed to compare survival for patients with severe isolated severe TR who underwent surgery to those who did not. In a propensity-matched sample considering surgery as a time-dependent covariate, there was no difference in overall survival between patients who received medical versus surgical management (HR 1.34). The authors concluded that that in patients with isolated severe TR, surgery is not associated with improved long-term survival.
Many patients with bicuspid aortic valve (BAV) develop AR but are not considered for valve repair, partly due to the limited long term data available pertaining to repair durability. This systematic review of 92 full papers aimed to evaluate durability and survival following BAV repair. The authors concluded that BAV repair is associated with acceptable long term survival. Ongoing standardized outcome assessments will further refine surgical techniques associated with excellent repair durability.
Cardiac Imaging
Summarised by Dr Sarah Catchpoole
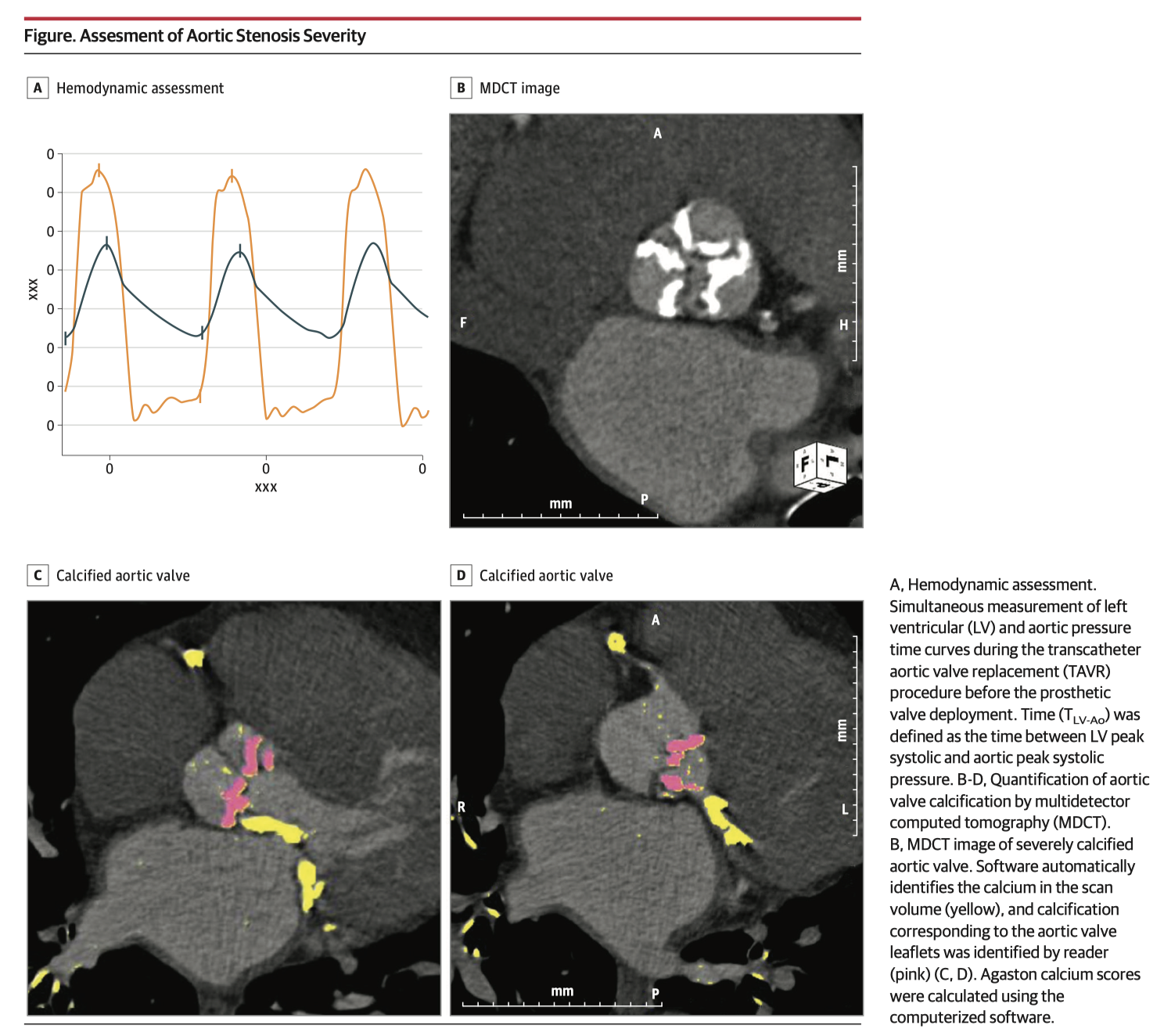
Low-gradient severe AS remains challenging to diagnose. This cohort study of 123 patients with AS undergoing transcatheter valve intervention has found that time between left ventricular and aortic systolic pressure peaks (TLV-Ao) provided a useful index of AS severity. Greater TLV-Ao was independently associated with severe aortic valve calcification, and provided incremental diagnostic value when compared with conventional echocardiographic variables. Of note, in patients with low-gradient AS, TLV-Ao was the only parameter associated with severe calcification.
Percutaneous occlusion of the left atrial appendage (LAA) is growing in popularity as a less invasive alternative in patients who cannot tolerate systemic anticoagulation for prevention of thromboembolism. This well-illustrated comprehensive review focuses on echocardiographic imaging in the peri-procedural period, including LAA anatomy and patient selection, available LAA devices and sizing, intra-procedural guidance, and post-procedural device evaluation.
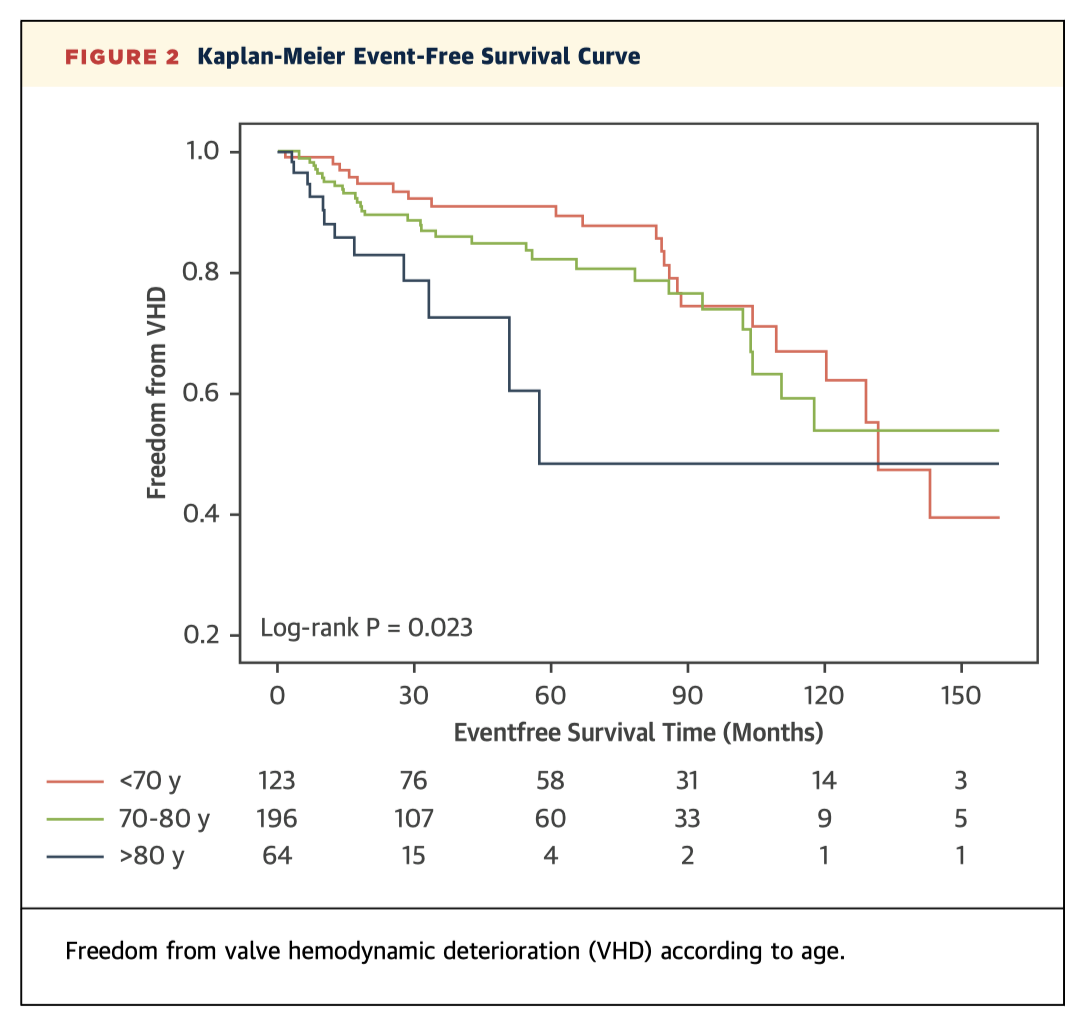
This prospective longitudinal cohort study followed 383 patients who underwent surgical bioprosthetic AVR between 1994-2009. Patients were followed up over a median of 113.2 months, or 4023 valve-years. The overall incidence of valve haemodynamic deterioration (VHD) was 18.3% (n=70, 4.8% per valve year) after a median of 32.4 months. VHD was associated with higher serum creatinine, arterial hypertension, porcine AVR, and patient-prosthesis mismatch. Of note, elderly patients were also more likely to develop VHD (Figure 2) – challenging previous findings that tissue valves in younger populations deteriorate faster.
Perioperative Medicine
Summarised by Dr Andrew Haymet
Significant TR recurs after tricuspid valve repair for functional TR in 15-20% within the first year and 30-70% within 5 years. This retrospective study of 54 patients with functional TR hypothesized that pre-repair tricuspid valve annular diameter (TVAD) is predictive of repair failure. The authors concluded that preoperative TVAD (diastole ≥4.2 cm; systole ≥3.7 cm), RV width (>4.88 cm), and postoperative RV function were all significant predictors of repair outcome. Earlier TV repair and optimizing right heart function may improve repair outcome.
Scoring systems used in cardiac surgery, such as the European System for Cardiac Operative Risk Evaluation and the Society of Thoracic Surgeons scoring systems, do not adjust for events that take place intraoperatively. The authors of this single–centre prospective cohort study of 4,446 consecutive cardiac surgical patients hypothesized that various intensive care unit scoring systems could predict not only in hospital mortality, but also other significant complications and long term survival after cardiac surgery. They concluded that the Intensive Care National Audit and Research Centre (ICNARC) scoring system is simple and can be used as an early warning screening tool to predict which patients are at higher risk of postoperative organ failure.













