Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been recently published in each speciality (Cardiology, Cardiac Surgery, Cardiac Imaging, Perioperative Medicine).
Cardiology
Summarised by Sarah Catchpoole
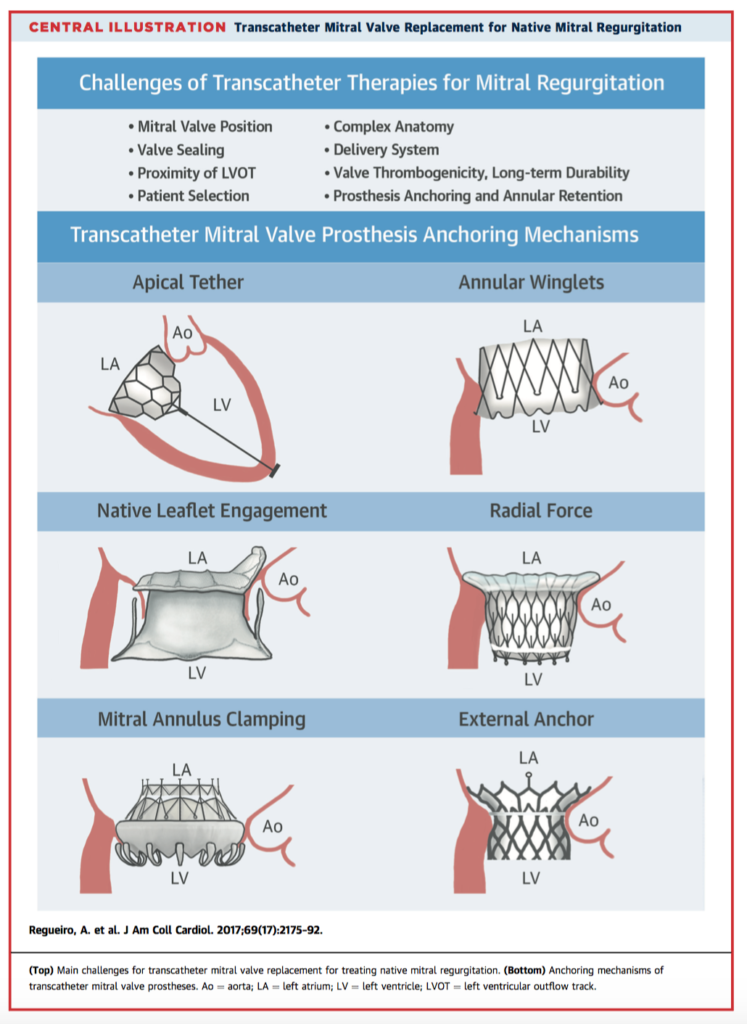
While transcatheter mitral valve repair has become established practice, less is known about transcatheter mitral valve replacement (TMVR). This review summarises the development, challenges, and future potential of TMVR, as well as the devices currently in pre-clinical or clinical evaluation. Results from early clinical trials involving 115 patients are also presented. To date, average technical success is high (88%, range 75 – 100%) with comparable haemodynamic results to repair or replacement, and average 30 day mortality of 23% (range 0-53%). These early results are promising, however further trials are needed to confirm efficacy, cost-benefit and safety.
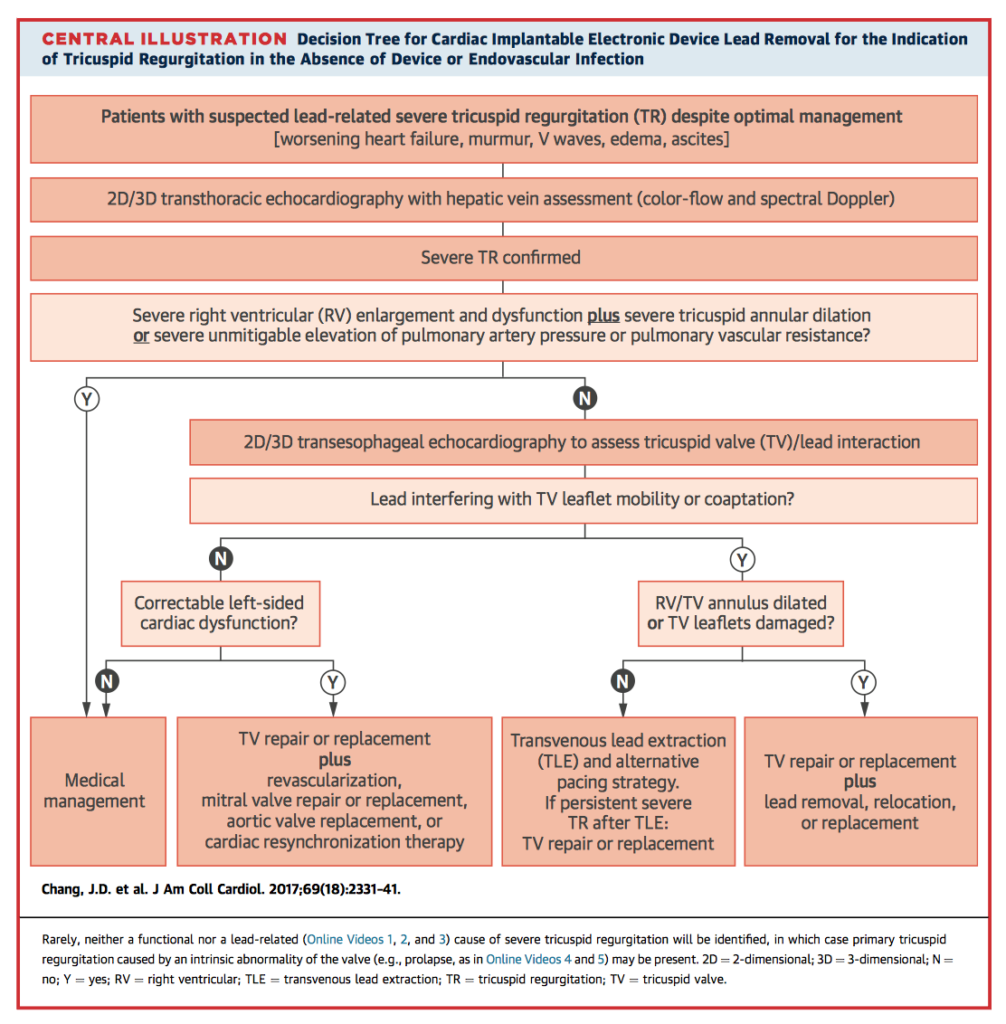
Tricuspid regurgitation (TR) is associated with increased mortality and occurs at higher rates in patients with cardiac implantable electronic devices (CIEDs). Chang et al. discuss likely mechanisms, including damage during insertion, interference with valve structures secondary to either direct mechanical effects or long-term tissue changes, and pacing-related dysfunction. Diagnosis and management of CIED related TR, including indications for lead removal, are summarised in the central illustration below. The authors emphasise the need for greater awareness of this potentially reversible cause of TR in the clinical environment.
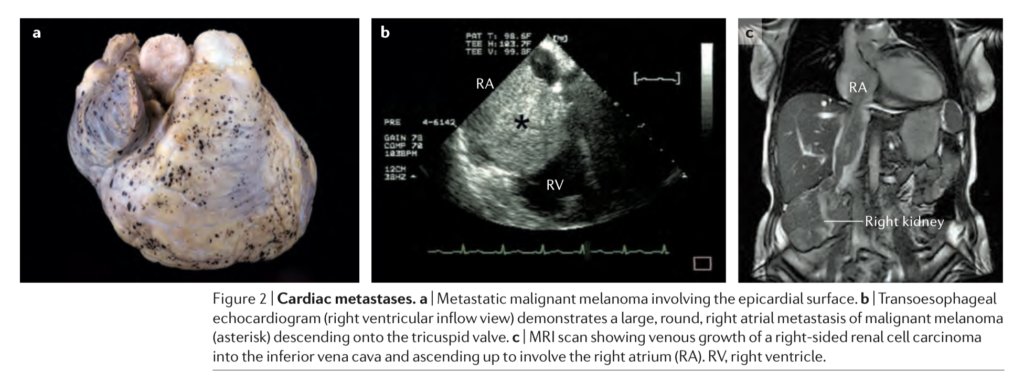
Our understanding of cardiac tumours has changed significantly thanks to contemporary research, including advances in molecular genetics, new drug therapies and the updated WHO 2015 classification system. This review provides an excellent update or summary resource to clinicians regarding this rare but often distressing diagnosis. Both benign and malignant tumours are covered individually in some detail, encompassing the presenting clinical context, associations, radiological features, diagnosis, prognosis and recommendations.
Cardiac Surgery
Summarised by Andrew Haymet
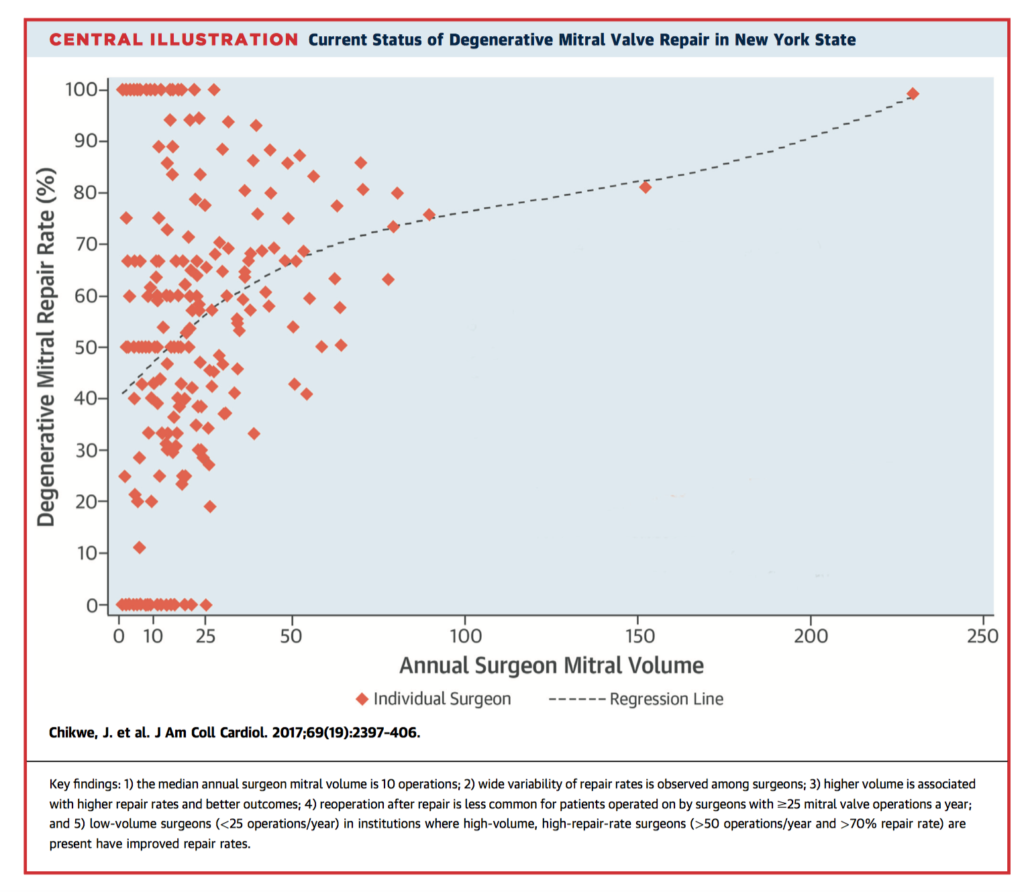
Degenerative mitral valve repair rates remain highly variable, despite established benefits of repair over replacement. The role of surgeon-specific factors is not clear. 5,475 patients within a mandatory New York State database who underwent mitral valve operations between 2002 and 2013 for degenerative mitral valve disease were identified. Mean annual surgeon volume of any mitral valve operation was 10 (range 1-230). Mean repair rate was 55% (n=20,797 of 38,128). Higher total annual surgeon volume was associated with increased repair rates of degenerative mitral valve disease (adjusted odds ratio [OR]: 1.13 for every additional 10 mitral operations; 95% confidence interval [CI]: 1.10 to 1.17; p < 0.001); a steady decrease in reoperation risk until 25 total mitral operations annually; and improved 1-year survival (adjusted hazard ratio: 0.95 for every additional 10 operations; 95% CI: 0.92 to 0.98; p = 0.001). The authors concluded that individual surgeon volume was a determinant of mitral repair rate, freedom from reoperation, and survival.
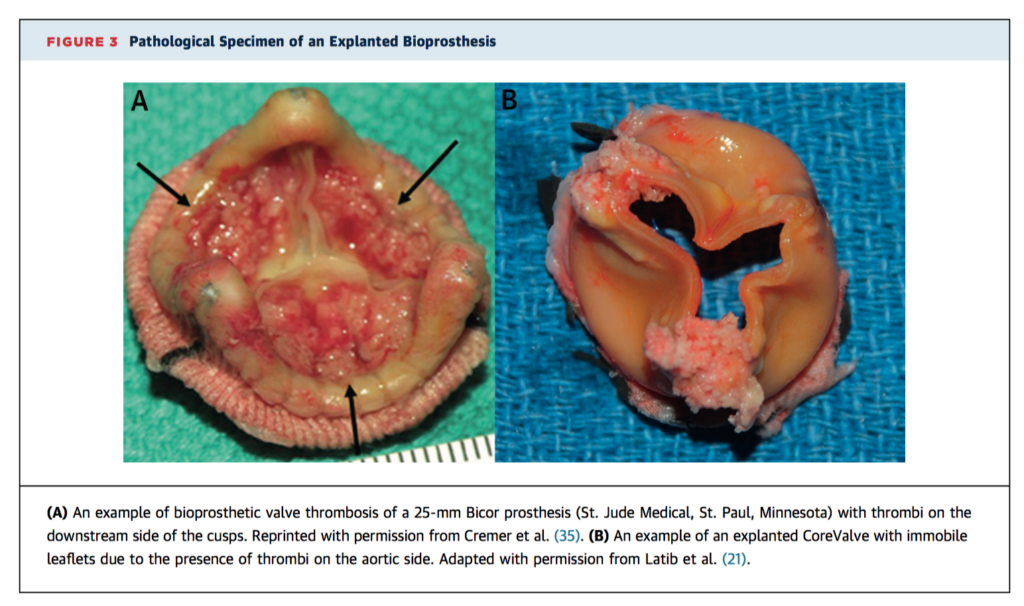
Puri R, et al. Bioprosthetic Valve Thrombosis. J Am Coll Cardiol. 2017 May 2.
Bioprostheses now comprise 80% of all surgical aortic valve replacements (SAVR) in the USA. Bioprosthetic valve thrombosis (BPVT) is considered a clinically rare event. Tremendous interest has been generated in this phenomenon of late because of recent systematic echocardiographic analyses, the increasing momentum of transcatheter heart valve (THV) technologies, and the highly sensitive nature of 4D computed tomographic imaging. There are currently no systematic prospective data regarding optimal treatment approach in THV recipients. Clinical suspicion of BPVT should be raised if BPV recipients present with dyspnoea and/or rising transvalvular gradients at any time post implantation. In the absence of clinically overt BPV obstruction, OAC therapy is recommended with follow up echocardiography 1-2 months following treatment initiation.
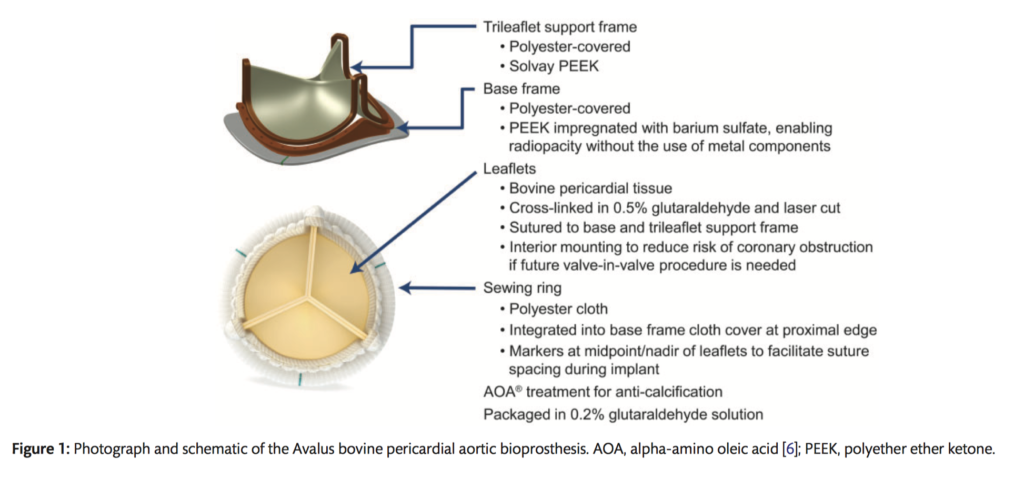
This prospective, non-randomized, multicentre study evaluated the safety, effectiveness and haemodynamic performance of a new bovine stented aortic valve bioprosthesis (Avalus). Death, valve-related adverse events (AE’s), functional recovery, and haemodynamic performance were evaluated at discharge, 3-6 months, and 1 year. Linearized rates were <2 x OPC (objective performance criteria) for death and valve-related thromboembolism, valve thrombosis, all and major PVL and endocarditis, but >/= 2 for all and major bleeding. Total number of valve-years was 459.5 (n=686). Survival at 1 year (n=270) was 96.4%. Patients showed sound functional recovery, and haemodynamic performance was within expected parameters. A good safety profile and clinical efficacy was demonstrated in all parameters for the Avalus valve except for bleeding rates. This may be related to long term, non-valvular anticoagulation and the length of follow up for this cohort.
Cardiac Imaging
Summarised by Sarah Catchpoole
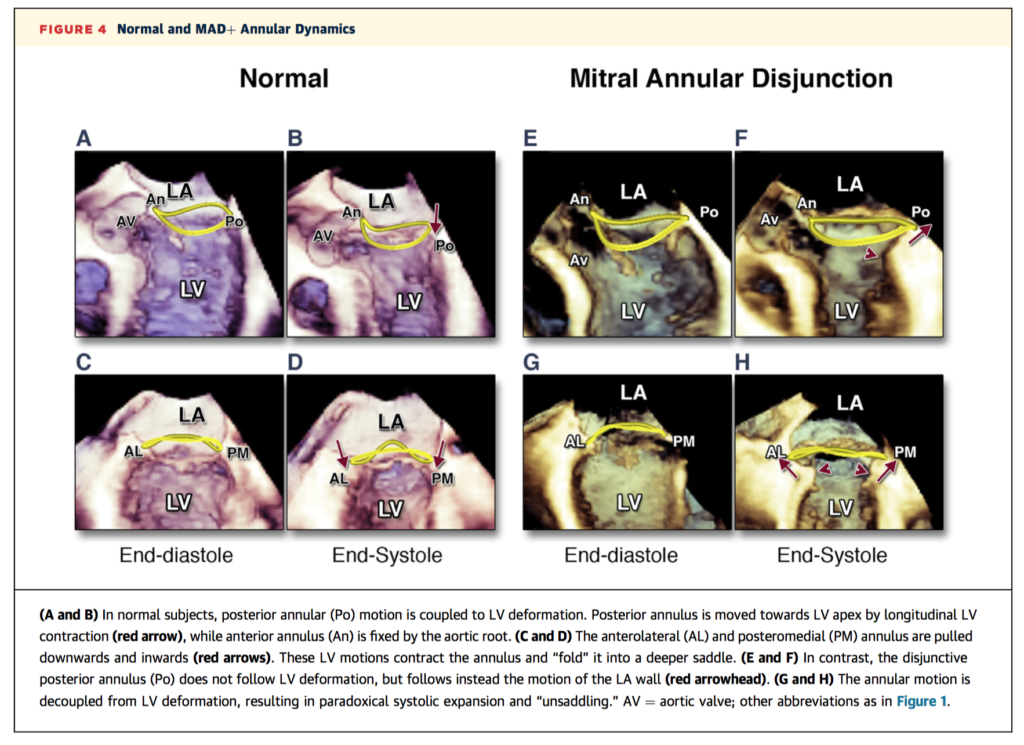
This is the first study to examine the 3D structure of the mitral annulus and its contribution to mitral valve prolapse (MVP), a leading cause of mitral regurgitation. 156 patients including those with MVP, heart failure and control subjects were recruited prospectively and underwent 3D transoesophageal echocardiography. Of the 101 patients with MVP, 42 were found to have mitral annular disjunction (MAD), defined as separation of the atrial-wall mitral valve junction from its ventricular attachment. MAD was associated with abnormal dynamics, paradoxical systolic flattening, and larger regurgitant orifice area (p < 0.0001 for all). The authors suggest these insights regarding the pathophysiology could have implications for surgical correction, including the potential benefits of annuloplasty compared to leaflet-oriented interventions such as mitral valve repair.
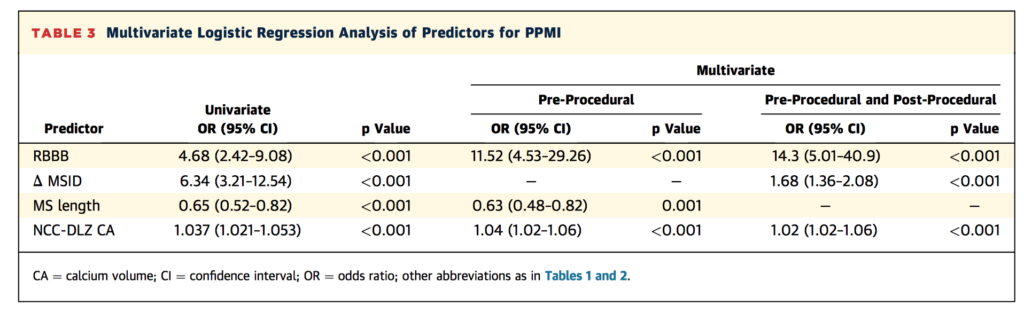
In this retrospective single-centre study, Maeno et al sought to determine risk factors for permanent pacemaker implantation (PPMI) after third generation balloon expandable TAVR. Of the 240 eligible participants, 35 (14.6%) required new PPMI. After mutli-variate logistic regression analysis, the noncoronary cusp device-landing zone calcium volume (NCC-DLZ CA) was found to be the best independent predictor of new PPMI, while right bundle branch block (RBBB), shorter membranous septum length and ventricular implantation depth were important synergistic risk factors. In combination, the authors have identified a highly predictive model with 94.3% sensitivity, 83.8% specificity, and negative predictive value of 98.8%.
Transcatheter aortic valve replacement (TAVR) under conscious sedation using transthoracic echocargiogram (TTE) for guidance is a comparable and cost-effective alternative to TAVR under general anaesthesia with transoesophageal echogradiography (TOE). In this study of 454 consecutive patients (234 TTE, 220 TOE), there was no difference in paravavular regurgitation at discharge (33% vs 38%, respectively, p = .326) and at 6 and 12 month follow up. However, TTE was associated with postdilation (38% vs 17%; P < .001) and requirement for a second valve (7% vs 2%, p = 0.26). The authors suggest further trials are needed to understand the higher risk of intraprocedural events for TTE compared to TOE, and that there is perhaps a predictable cohort of patients who could benefit equally from the cost effective TTE alternative.
Perioperative Medicine
Summarised by Andrew Haymet
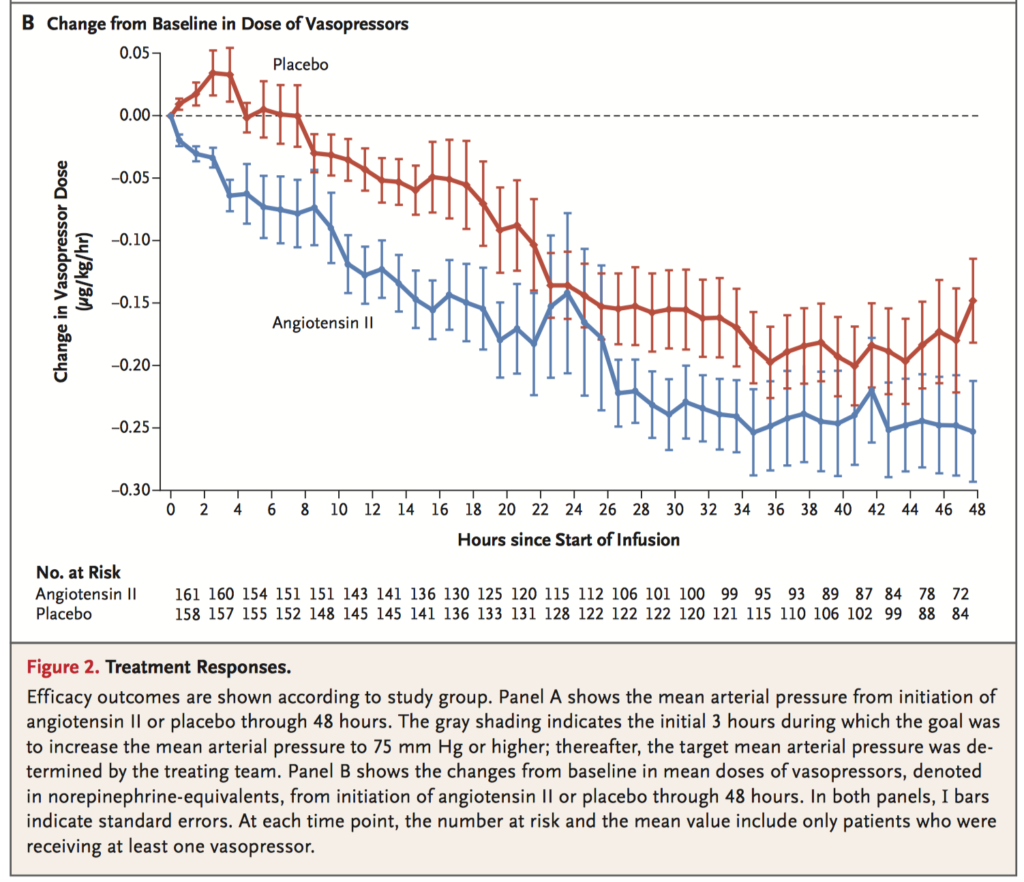
Vasodilatory shock that is refractory to high dose pressor support is associated with high mortality. 344 patients who were receiving more than 0.2 µg of norepinephrine per kilogram body mass were randomly assigned to one of two regimens to investigate the effectiveness of angiotensin II for the treatment of this condition. 163 received angiotensin II, and 158 received placebo. Primary endpoint was a response with mean arterial pressure at 3 hours after the start of infusion, with a response defined as at least 10mmHg increase from baseline or reaching a nominal value of 75mmHg without concomitant increases in other vasopressors. The primary end point was reached by more patients in the angiotensin II group (114 of 163 patients, 69.9%) than in the placebo group (37 of 158 patients, 23.4%) (odds ratio, 7.95; 95% confidence interval [CI], 4.76 to 13.3; P<0.001). Angiotensin II was found to increase blood pressure in patients with vasodilatory shock that was unresponsive to high doses of conventional vasopressors.
This systematic review and meta-analysis of 6 observational studies with 137 patients aimed to assess differences in grade of mitral regurgitation (MR) between preoperative and intraoperative evaluations. The primary outcome was the difference between the preoperative and intraoperative MR grade under “GA-only” or “after-haemodynamic matching (HM).” Risk of MR underestimation was found under “GA-only” (SMD: 0.55; 95% confidence interval [CI], 0.31–0.79, p = 0.00001), but not “after-HM” (SMD: –0.16; 95% CI, –0.46 to 0.13, p=0.27). The overall reported incidence of misdiagnoses was slightly more common under “GA-only” (mean 48%, 39% underestimation, 9% overestimation; range: 32%–57%) than “after-HM” (mean 41%, 12% underestimation, 29% overestimation; range: 33%–50%). Intraoperative assessment under “GA-only” significantly underestimated MR. Afterload manipulation can be used to obtain a more accurate intraoperative evaluation, although HM carries high risk of clinically significant overestimation.
Atrial fibrillation (AF) is a common complication after cardiac surgery. This retrospective observational study evaluated the all-comer strategy of epicardial amiodarone application for the prevention of postoperative AF. A cohort of 200 cardiac surgery patients who had no prior history of AF were treated with either no amiodarone (historical control, n=100), epicardial amiodarone mixed in a topical hydrogel (n=50) or epicardial application of an amiodarone-soaked sealant patch (n=50). The incidence of postoperative AF did not significantly differ between the three groups, with 29 of 100 (29%) having new AF in the historical control group, compared with 18 of 50 (36%) in the amiodarone-hydrogel group, and 18 of 50 ( 36%) in the amiodarone-patch group (P=0.56). Routine application of topical amiodarone was not associated with a reduction in the incidence of new-onset postoperative atrial fibrillation in this study.













