Welcome to the monthly SHDA Research Update. Our specialists have selected 3 seminal papers that have been recently published in each speciality (perioperative medicine, cardiac imaging, cardiothoracic surgery, cardiology).
Perioperative Medicine
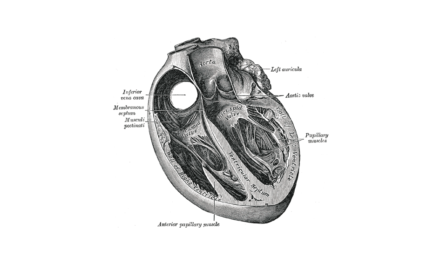
Obase et al. assessed the utility of 3D transoesophageal echocardiography (TOE) in measuring mitral chordal length. Transgastric full-volume sets were obtained from 22 patients and 146 primary chords were examined prior to mitral valve surgery. These measurements were then compared with surgical findings. The chordal length could be measured by 3D TOE in all 146 chords and correlated very closely to surgical findings, which validates this technique for chordal assessment.
While TOE is routinely used to assess the aorta, it is less commonly used to assess its branches. Salerno et al describe how to obtain TOE views of individual coronary arteries and how to detect significant stenosis in these vessels. Further descriptions are provided on how to interrogate the aortic arch vessels, the left internal mammary artery (and its flow characteristics), the posterior intercostal arteries and the renal, celiac and superior mesenteric arteries. These authors also provide some interesting case reports on how these techniques can change surgical management.
Cardiac ultrasound is an essential component of successful Extracorporeal Life Support (ECLS) Programs. It is used to guide the type of support required, safe cannulation, ongoing management and weaning, as well as surveillance for complications. This brief communication from the Council on Perioperative Echocardiography outlines the clinical utility of cardiac ultrasound in the safe provision of modern ECLS.
Cardiac Imaging
Significant paravalvular regurgitation post TAVI still remains a concern, & predicting the residual regurgitation has to date been challenging. Mihara et al. have devised a simple visual assessment (0-3) of aortic valve calcification near the annulus, using circumferential and radial lengths as well as the calcification protruding into the left ventricular outflow tract. This new assessment of annular calcification as opposed to leaflet calcification has some promising results in predicting the degree of paravalvular regurgitation.
Secondary mitral valve regurgitation in patients with significant aortic incompetence is a known phenonomen and has been attributed to papillary muscle displacement and tethering of the mitral leaflets affecting true coaptation. Regeer et al. evaluated the geometry of the mitral valve and subvalvular apparatus using 3D echo in 129 patients undergoing aortic valve/root surgery for AR grade ≥ 2. MR ≥ 2 was present in 23% of these patients. On multivariate logistic regression analysis, lower LVEF and larger left atrial volume were independently associated with MR grade ≥2 after correcting for tenting area and inter-papillary muscle distance.
Islas et al. have assessed the safety of TAVI with and without balloon predilation (BPD). They assessed the aortic annulus and root, leaflet mobility and degree of calcification, orifice characteristics, valve area, and aortic regurgitation using TOE in 249 patients, then selected 79 patients on the basis of specific criteria to undergo TAVI without BPD. There was no significant difference in residual paravalvular regurgitation. However, patients who did not have predilation had a lower incidence of pacemaker insertion (6.3% vs 14.1%, p=.030), & lower procedure-related mortality (2.5% vs 11.8%, p=.018). Thus with careful echocardiographic evaluation TAVI without BPD is safe.
Cardiology
Mack et al. have reported the latest follow-up of the PARNTER I trial, which compared TAVI to SAVR in high risk patients. This represents the longest follow-up of randomized patients to date. At 5 years, risk of death was 67·8% in the TAVI group vs. 62·4% in the SAVR group (HR 1.04, 95% CI 0.86 – 1.24, p=0·76). There was no SVD required AVR in either group. Moderate or severe AR occurred in 40 (14%) of 280 patients in the TAVR group and two (1%) of 228 in the SAVR group (p<0·0001), and was associated with increased 5-year risk of mortality in the TAVR group (72.4% for moderate or severe aortic regurgitation vs 56.6% for those with mild aortic regurgitation or less, p=0·003).
 The TriGuard HDH Embolic Deflection Device is a porous “shield” designed to be placed over the aortic arch vessels to reduce the passage of embolic material. In the DEFLECT III trial 85 patients undergoing TAVI were randomized to TriGuard protection vs. no protection. Technical success (3-vessel cerebral coverage), was achieved in 88.9% of cases. The primary safety endpoint (composite of death, stroke, bleeding, acute kidney injury, & major vascular complications) was similar between groups (21.7% of TriGuard vs. 30.8%, p=0.34). TriGuard use was associated with greater freedom from new ischaemic brain lesions detected by diffusion-weighted MRI (26.9 vs. 11.5%), fewer new neurologic deficits detected by the NIH Stroke Scale (3.1% vs. 15.4%), & improved Montreal Cognitive Assessment (MoCA) & memory task scores.
The TriGuard HDH Embolic Deflection Device is a porous “shield” designed to be placed over the aortic arch vessels to reduce the passage of embolic material. In the DEFLECT III trial 85 patients undergoing TAVI were randomized to TriGuard protection vs. no protection. Technical success (3-vessel cerebral coverage), was achieved in 88.9% of cases. The primary safety endpoint (composite of death, stroke, bleeding, acute kidney injury, & major vascular complications) was similar between groups (21.7% of TriGuard vs. 30.8%, p=0.34). TriGuard use was associated with greater freedom from new ischaemic brain lesions detected by diffusion-weighted MRI (26.9 vs. 11.5%), fewer new neurologic deficits detected by the NIH Stroke Scale (3.1% vs. 15.4%), & improved Montreal Cognitive Assessment (MoCA) & memory task scores.
Cardiothoracic Surgery
David et al. describe the longest follow-up of valve-sparing aortic root replacements from a single institution to date. A reimplantation technique was used in 296 patients (the David procedure), a remodeling technique was used 75, cusp repair was performed in 36.6%, and reinforcement of the free margin in 24.2%. Survival at 18 years was 76.8% ± 4.31%, which was lower than an age & gender matched general population. Freedom from reoperation at 18 years was 94.8% ± 2.0% (8 patients for recurrent AI and 2 patients for infective endocarditis). The authors concluded that a slow but progressive deterioration of aortic valve function seems to occur during the first 2 decades. However preoperative AI and cusp repair had no adverse effect on valve function.
Coronary ostial reimplantation during aortic root replacement is usually performed using the “button technique”, but there are still concerns about the incidence of coronary pseudoaneurysm formation, bleeding, and distortion of the coronary geometry. The authors describe an adapted trapdoor technique, which is commonly used in the arterial switch operation in children. They performed it routinely in their adult aortic root replacements, and in 14 that underwent postop imaging for non-ischaemic reasons there were no stenoses, aneurysms, or malposition of the coronaries detected.
Vallabhajosyula et al. compared DHCA with retrograde cerebral perfusion (RCP) (n=301) to MHCA (≥25℃) with antegrade cerebral perfusion (ACP, established via axillary or innominate artery cannulation) (n=75) in patients undergoing transverse hemiarch replacement for aortic aneurysm disease. MHCA+ACP resulted in significantly improved cross-clamp times (128 ± 46 vs 163 ± 57 min, p<0.01) and CPB time (167 ± 49 vs 222 ± 61 min, p<0.01), and reduced transfusion requirements (38% vs 61%, p<0.01). Other postoperative outcomes, including stroke and mortality, were similar.