Welcome to the monthly SHDA Research Update. Our specialists have selected seminal papers that have been published recently in each speciality (cardiology, cardiac surgery, cardiac imaging, perioperative medicine).
This paper presents the results of the FIRE and ICE trial, a multicentre RCT that compared cryoballoon and radiofrequency ablation in 762 patients with drug-refractory, symptomatic, paroxysmal atrial fibrillation.
Prior to this trial, six previous studies had been conducted to compare these two techniques but all were small and/or non-randomised trials and results were conflicting. This large trial was therefore designed to close the evidence gap.
The researchers hypothesized that cryoballoon ablation would be non-inferior to radiofrequency ablation at the primary efficacy endpoint which was pre-specified as the first documented clinical failure at > 90 days after the ablation procedure. The 762 patients were followed up for a mean of 1.5 years. The primary efficacy end point was not significantly different between the two groups, occurring in 138 patients in the cryoballoon group and 143 in the radiofrequency group (HR 0.96; 95% CI 0.76, 1.22). The primary safety endpoint did not differ between the two groups (P = 0.24).
The study authors concluded that: “In this randomized trial, cryoballoon ablation was non-inferior to radiofrequency ablation with respect to efficacy for the treatment of patients with drug-refractory paroxysmal atrial fibrillation, and there was no significant difference between the two methods with regard to overall safety.”
FIRE and ICE quick take video
Nalliah CJ, et al. The role of obesity in atrial fibrillation. Eur Heart J. 2016 May 21.
This comprehensive review outlines all aspects of the role obesity plays in the pathogenesis of atrial fibrillation and the authors advocate for “incorporation of weight reduction strategies to optimize chances of durable rhythm control.”
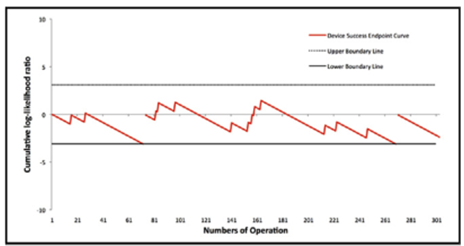
Nalliah et al. (2016) outline 8 population-based studies and three clinical studies that have shown significant association between obesity and atrial fibrillation. The largest clinical study was the LEGACY cohort of 825 obese patients with atrial fibrillation (Pathak et al. 2015) in which patients who lost >10% body weight had the most significant reduction in atrial fibrillation burden (see figure below).
The review also outlines the clinical and mechanistic evidence for a relationship between obesity and atrial fibrillation. There is evidence that weight loss is associated with cardiac remodelling, lower recurrence of atrial fibrillation and improved AF-free survival following ablation. Studies have also shown electrophysiological atrial changes in patients with weight gain or obesity and that pericardial fat deposits are associated with AF.
The authors concluded that:
“Obesity often co-exists with multiple AF risk factors that improve in response to weight loss, making a consolidated approach of weight loss and AF risk factor management preferable. However, weight loss for AF remains in its infancy, and its broad adoption as a management strategy for AF remains to be defined.”
Dr Thomas Lüscher, Editor-in-Chief of the European Heart Journal has written an accompanying editorial to the Nalliah et al. (2016) paper above, which was included as one of a series of four papers on atrial fibrillation in this special journal issue. Dr Lüscher comments on the four papers which assess different aspects of this condition including risk factors and mechanisms.
One of the studies, by Perez et al. (2016) utilised data from 8,832 postmenopausal women who were participants in the Women’s Health Initiative. The researchers observed an association between total lean body mass and AF that was significant even after adjustment for total fat mass (HR 1.22 per 5 kg increase in lean body mass). They concluded that “greater lean body mass is a strong independent risk factor for atrial fibrillation.”
Another study by Singh et al. (2016) presented the results of the MAGIC-AF trial which investigated stepwise ablation using low dose ibutilide in AF patients. The primary efficacy endpoint was achieved in similar numbers in both the ibutilide and placebo groups (56% vs 49% respectively, N.S.) and there were no significant differences in complications between the two groups.
“The epidemic of atrial fibrillation requires more intensive research into the complex mechanisms of this arrhythmia,” stated Dr Lüscher.
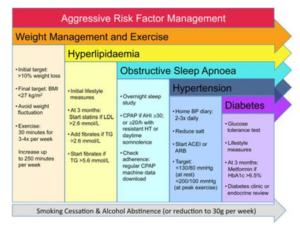
Figure legend: Aggressive risk factor management in patients with obesity and atrial fibrillation. Adapted from Pathak et al. BMI, body mass index; LDL, low-density lipoprotein; TG, triglyceride; BP, blood pressure; ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker, AHI, apnoea–hyponoea index; CPAP, continuous positive airway pressure (from Lau et al. European Heart Journal (2016) 37, 1573).
Cardiac Imaging
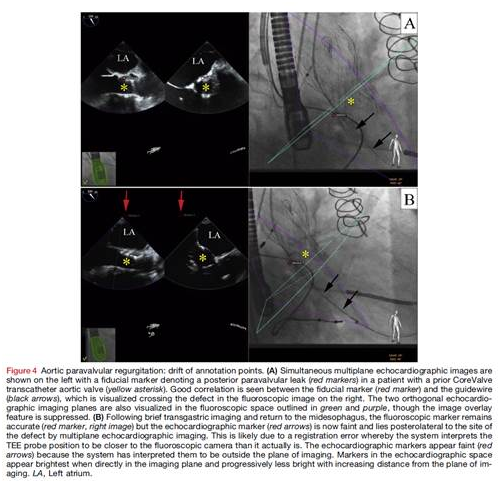
Thaden JJ, et al. Echocardiographic and Fluoroscopic Fusion Imaging for Procedural Guidance: An Overview and Early Clinical Experience. J Am Soc Echocardiogr. 2016 Jun.
This is an excellent critical overview of procedural guidance using echocardiographic-fluoroscopic fusion imaging. Technical considerations and applications for fusion imaging are outlined including sources of image registration error.
In the overview the authors also outline strengths, limitations, and potential clinical applications of this relatively new technology. Recommendations for future clinical research to further determine its benefits are also presented.
This prospective study of 266 patients with nonvalvular atrial fibrillation investigated how diastolic function affects the risk of left atrial appendage (LAA) thrombus. This study follows on from results of previous retrospective studies in patients with nonvalvular atrial fibrillation that have observed an association between the diastolic function E/e’ ratio and e’ velocity and the formation of spontaneous echo contrast and LAA thrombi.
Transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE) were used to measure a number of parameters including mitral inflow E velocity and tissue doppler septal and lateral mitral annulus velocities; E/e’ ratios were also calculated.
Patients that had LAA thrombus (6.4%) were significantly more likely to have a higher mean CHA2DS2-VASc score (4.6 vs 3.0; P < 0.001), a higher mean lateral E/e’ ratio (19.4 vs 10.2, P < 0.001), and a lower mean lateral e’ velocity (P = 0.001).
The authors concluded that:
“To our knowledge, this is the first study to prospectively and simultaneously correlate commonly used diastolic function parameters with LAA thrombus formation in patients with NVAF. We demonstrated that a normal E/e’ ratio seems to be protective from LAA thrombus formation, and there was a stepwise increase in LAA risk with worsening diastolic function measures.”
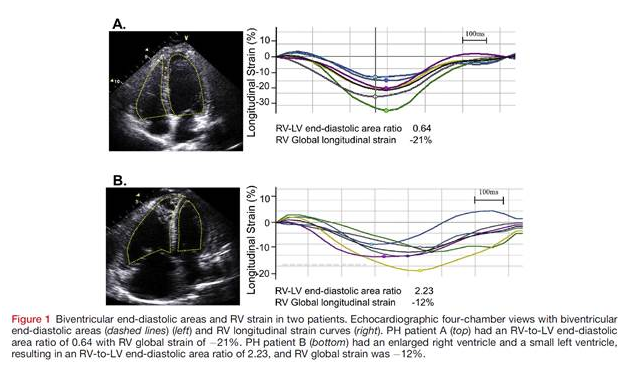
This prospective study of 139 patients with precapillary pulmonary hypertension (WHO class I) found that the RV-to-LV end-diastolic area ratio was predictive of 5-year survival. The researchers used speckle-tracking echocardiography to measure RV free wall and global strain. The RV-to-LV end-diastolic area ratio, as an index of biventricular cardiac remodelling, was measured using the apical four-chamber view.
There were 72 (52%) deaths over the 5 year study period and patients with RV-to-LV end-diastolic area ratios ≥ 0.93 were at significantly increased risk of death (HR 1.84; P=0.019).
The authors concluded that:
“Biventricular remodelling by the echocardiographic RV-to-LV end-diastolic area ratio correlated with hemodynamic data and was predictive of long-term outcomes in patients with PH.”
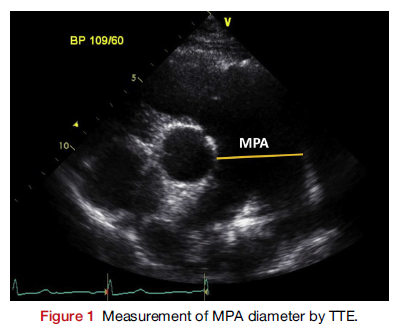
In this prospective study of 298 patients with pulmonary arterial hypertension (PAH), 46 (15.4%) patients with dilated main pulmonary artery (PA) were identified. The aim of the study was to determine the prevalence of PA enlargement and the relationship between main PA diameter, measured by TEE, and mechanical complications related to sudden cardiac death.
In patients with PAH the mean diameter of the main PA was 51.0 ± 9.0 mm. Mechanical complications were identified by cardiac CT in 16/46 (34.8%) of patients and included extrinsic left main coronary artery compression by the main PA (32.6%), airway compression (4.3%), and thrombus in the PA (8.7%). The main PA was significantly larger in patients with complications (55.6 mm vs. 46.7 mm; P = 0.012). Two parameter, main PA diameter and tricuspid regurgitation area, were predictive of complications.
The authors concluded that:
“These findings indicate that close monitoring for dilatation of the PA and a more aggressive diagnostic approach toward mechanical complications are warranted in patients with PAH who present with progressive PA dilatation.”
Cardiac Surgery – Summarised by Andrew Haymet
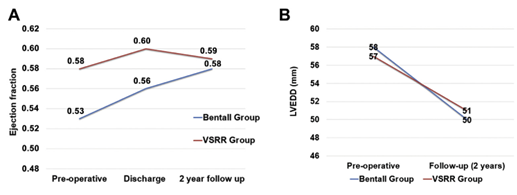
This study retrospectively compared the outcomes of primary cusp repair with root reimplantation (VSRR, n=45) to those of Bentall procedures (n=120). 710 patients with bicuspid aortic valves underwent aortic root procedures between 2002-2014. Only patients presenting with noncalcific bicuspid valves were included (n=165). 30-day and in-hospital mortality was zero; in-hospital stroke rate was 0.8% (n=1) in the Bentall group and 0 in the VSRR group (p=0.54). There were 14 transient ischaemic or stroke events in the Bentall group and zero in the VSRR group. Five-year actuarial survival was similar (100% vs 98% +/- 2%, p=0.8). Primary cusp repair with root reimplantation was shown to achieve similar midterm outcomes compared to Bentall procedures.
LV remodelling in Bentall (blue) and VSRR (red) for preoperative and 2-year follow-up, shown as LVEF (A) and LV end-diastolic dimension (B)
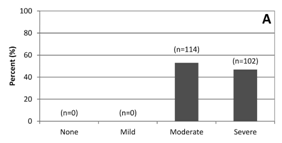
Recurrence of functional tricuspid regurgitation (TR) has been shown to be high after repair. Results of repair with undersized rigid nonplanar annuloplasty rings in 216 patients between 2007 and 2013 were evaluated. At a mean follow up of 33.0+/- 24.0 months, TR grade was none or mild in 81% of patients (130/160), moderate in 16% (26 of 160) and severe in 2% (4/160). There were no reoperations for recurrent TR, nor did any patients develop tricuspid stenosis or ring dehiscence. The authors concluded this method to be safe and highly effective with near absence of recurrent severe TR at midterm follow-up.
Changes in TR grades preoperatively (A) and during follow up (C).
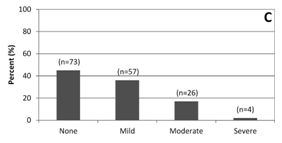
The learning process and quality of care of right minithoracotomy sutureless aortic valve replacement (AVR) was evaluated in 300 consecutive patients between 2011 and 2015. Departmental and individual learning curves were calculated using sequential probability cumulative sum failure analysis. Two composite end points of technical success and 30-day complications were used as quality indicators. AVR was successful in 99% of patients (298/300), with overall mortality of 0.7% (2 patients). Cumulative sum analysis did not reveal any significant learning effects for technical success, however 30-day complications showed a series of initial failures at the start of the study, which was rectified with internal auditing. The authors concluded that right minithoracotomy sutureless AVR delivers excellent results, and that outcomes rapidly improve with experience.
Overall institution CUSUM curve for device success end point.
Isolated mitral valve cleft is an uncommon cause of congenital mitral regurgitation. Typically the aortic or anterior leaflets are affected with rare involvement of the mural or posterior leaflet. To the best of the authors’ knowledge, this was the first reported case of a “true” cleft in both the aortic and mural mitral valve leaflets. Transthoracic echocardiography provided initial suspicion of this lesion, with confirmation by transoesophageal echocardiography and intraoperative findings. Repair was achieved by apposition of both the anterior and posterior mitral clefts with sutures, and posterior ring annuloplasty with bovine pericardium. This case demonstrated that real-time three-dimensional echocardiography was highly predictive of detailed surgical anatomy and will prove indispensable in differentiating rare mitral valve malformations and normal anatomical variants.
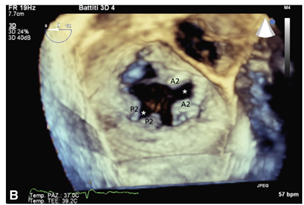
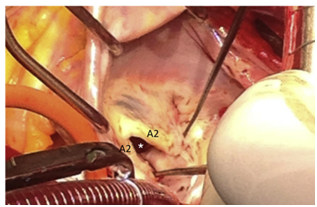
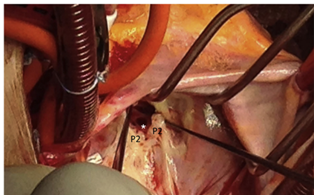
(B) A large cleft within the aortic scallop A2 is shown to reach the mitral annulus inferior to the mitroaortic junction, with a second cleft within the mural scallop P2. Corresponding intraoperative views of these clefts are shown.
This expert review outlines the importance of valve phenotype and the Sievers classification of the bicuspid aortic valve (BAV) with a particular focus on the information important to the perioperative echocardiographer. BAV occurs in 1-2% of the population and repair is becoming more common, particularly in younger patients wishing to avoid prosthetic aortic valves and their associated complications.
Topics covered include classification of the BAV, Sievers type 0, 1 and 2 BAV, characteristics in advanced disease, aortic anomalies associated with BAV, decision-making in BAV repair, and different categories of repairable BAVs.
The authors emphasised that the cusps have to be fairly normal for the BAV to be preserved and that the perioperative echocardiographer must pay attention to cusp quality in order to determine valve repairabilty.
The authors of the review concluded:
“The Sievers classification of BAVs has become an accepted standard by experts in the field to describe the phenotypic variation within the framework of the functional aortic annulus as a platform for planning surgical repair.”
This prospective study of 74 previously untreated patients with idiopathic pulmonary arterial hypertension (IPAH) showed that the RV M/V ratio was a good predictor of prognosis. Baseline measurements including echocardiographic and cardiac MRI were recorded. Patients were followed for a mean of 541 days and monitored for clinical worsening.
At 2 years 46% of patients had presented with clinical worsening. At baseline, independent predictors of clinical worsening were pericardial effusion and cardiac index. Utilising statistical methods including linear regression analysis and actuarial freedom from clinical worsening, the researchers determined that low values of RV M/V ratio independently predicted poor outcome.
The authors concluded that:
“This finding is of great interest because it may allow clinicians to better stratify patients with a normal CI, identifying at an early stage those patients at a higher risk of right-sided HF development before hemodynamic instability appears.”