ELSO was founded in 1989 and is since collecting valuable data on extracorporeal life support with currently about 350 active centres worldwide contributing ECMO patient data. An annual meeting has since been held in North America, regional meetings have only developed in more recent times. This was the 3rd Asian Pacific meeting after Beijing in 2013 and Kyoto in 2015.
The excellent program was put together by John Fraser and his team with many national and international leaders in the field sharing their views. The exhibition hall served as a great melting pot to meet and exchange experiences with physicians and allied ECMO team members from around the globe (see picture below).
My personal conference highlights:
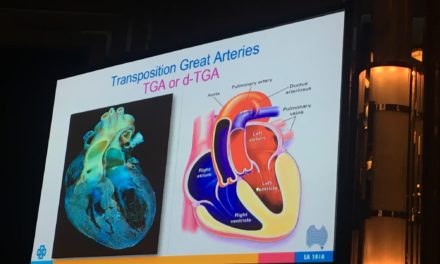
- Pre-conference held at the all new and shiny Gold Coast University Hospital started with a variety of workshops including ECMO in paediatrics, the La Pitié Salpetrière mechanical circulatory support, advanced ECMO and a totally hands on ECMO simulation training by ‘learnECMO’ and an innovative team from Hong Kong (see picture below).
- The well-attended session on ECPR, which is initiation of ECMO during cardiac arrest, was fascinating. The discussion in this section covered the whole spectrum of opinions. Proficiently executed ECPR will yield survival of 20-25% for out of hospital cardiac arrest in experienced centres. Some may consider this low survival levels, these patients though have refractory VT/VF cardiac arrest and are virtually dead. Survival after cardiac arrest drops off sharply over time even for shockable initial rhythms. After 20 min 90% of those who survive will have had return of spontaneous circulation [ROSC] and after 40 min the survival approaches zero. Achieving 20-25% survival in this group understandably draws a lot of attention. Questions regarding its applicability and general economic viability though were discussed. Cost implications, the infrastructure necessary and the very few numbers of patients make this a Western World endeavour similar to other high cost per quality life year gained therapies.
- What’s news for VV-ECMO? VV-ECMO is well established since the 2009 flue epidemic yet is still finding its exact place in the intensive care world. The ART trial (alveolar recruitment in ARDS trial, released in JAMA 2017), a RCT comparing an ‘open lung’ strategy with recruitment and higher PEEP to a standard ARDSnet ventilation. Increased mortality for the recruitment group, rose questions about the trial itself but also beyond about the place and timing of VV-ECMO in managing ARDS. An entertaining debate was held and one can only look forward the results of the EOLIA study early next year which will shed further light on the evidence for VV-ECMO.
The type of research that would help us to move forward in ECMO also sparked some discussion. Large RCTs versus selected, careful observational cohort studies reducing the risk of mixing fundamentally different patient group and diluting potential signals – the jury is out on that.
- And last but not least Bob Bartlett the ‘father’ of ECMO put on the swim cap with one of the local ECMO survivors (see picture below) and talking on ‘What I would advise my 30-year-old self’. It was refreshing to hear that he emphasised broad clinical experience and the joy of patient care rather than saying research, research, research.
This only leaves to mention the great effort for the Asian attendees, which for some was major undertaking to come to Australia. There is more ECMO in Asia than we all know of. In this sense, we are all looking forward to see you at the NEXT APELSO held in Bangkok, Thailand 2019.